Abstract
Purpose
PROMIS-Preference (PROPr) is a generic, societal, preference-based summary score that uses seven domains from the Patient-Reported Outcomes Measurement Information System (PROMIS). This report evaluates construct validity of PROPr by its association with social determinants of health (SDoH).
Methods
An online panel survey of the US adult population included PROPr, SDoH, demographics, chronic conditions, and four other scores: the EuroQol-5D-5L (EQ-5D-5L), Health Utilities Index (HUI) Mark 2 and Mark 3, and the Short Form-6D (SF-6D). Each score was regressed on age, gender, health conditions, and a single SDoH. The SDoH coefficient represents the strength of its association to PROPr and was used to assess known-groups validity. Convergent validity was evaluated using Pearson correlations between different summary scores and Spearman correlations between SDoH coefficients from different summary scores.
Results
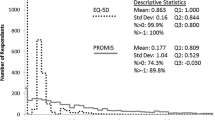
From 4142 participants, all summary scores had statistically significant differences for variables related to education, income, food and financial insecurity, and social interactions. Of the 42 SDoH variables tested, the number of statistically significant variables was 27 for EQ-5D-5L, 17 for HUI Mark 2, 23 for HUI Mark 3, 27 for PROPr, and 27 for SF-6D. The average SDoH coefficients were − 0.086 for EQ-5D-5L, − 0.039 for HUI Mark 2, − 0.063 for HUI Mark 3, − 0.064 for PROPr, and − 0.037 for SF-6D. Despite the difference in magnitude across the measures, Pearson correlations were 0.60 to 0.76 and Spearman correlations were 0.74 to 0.87.
Conclusions
These results provide evidence of construct validity supporting the use of PROPr monitor population health in the general US population.



Similar content being viewed by others
Data availability
References
Ashraf, K., Ng, C. J., Teo, C. H., & Goh, K. L. (2019). Population indices measuring health outcomes: A scoping review. Journal of Global Health. https://doi.org/10.7189/jogh.09.010405
Kindig, D. A. (2000). Purchasing population health: Paying for results. Ann Arbor: University of Michigan Press.
Breslow, L. (2006). Health measurement in the third era of health. American Journal of Public Health, 96(1), 17–19. https://doi.org/10.2105/ajph.2004.055970
Jones, N., Jones, S. L., & Miller, N. A. (2004). The Medicare Health Outcomes Survey program: Overview, context, and near-term prospects. Health and Quality of Life Outcomes. https://doi.org/10.1186/1477-7525-2-33
Medicare Health Outcomes Survey. Retrieved April 10, 2020, from https://www.hosonline.org/
Cohen, S. B. (2003). Design strategies and innovations in the medical expenditure panel survey. Medical Care. https://doi.org/10.1097/01.mlr.0000076048.11549.71
McDowell, I. (2006). Measuring health: A guide to rating scales and questionnaires. New York: Oxford University Press.
Torrance, G. W. (1986). Measurement of health state utilities for economic appraisal. Journal of Health Economics, 5(1), 1–30. https://doi.org/10.1016/0167-6296(86)90020-2
Keeney, R. L., & Raiffa, H. (1993). Decisions with multiple objectives: Preferences and value trade-offs. Cambridge: Cambridge University Press.
Cherepanov, D., Palta, M., Fryback, D. G., & Robert, S. A. (2010). Gender differences in health-related quality-of-life are partly explained by sociodemographic and socioeconomic variation between adult men and women in the US: Evidence from four US nationally representative data sets. Quality of Life Research, 19(8), 1115–1124. https://doi.org/10.1007/s11136-010-9673-x
Coley, S. L., Leon, C. F. M. D., Ward, E. C., Barnes, L. L., Skarupski, K. A., & Jacobs, E. A. (2017). Perceived discrimination and health-related quality-of-life: gender differences among older African Americans. Quality of Life Research, 26(12), 3449–3458. https://doi.org/10.1007/s11136-017-1663-9
Robert, S. A., Cherepanov, D., Palta, M., Dunham, N. C., Feeny, D., & Fryback, D. G. (2009). Socioeconomic status and age variations in health-related quality of life: Results from the national health measurement study. The Journals of Gerontology Series B, 64B(3), 378–389. https://doi.org/10.1093/geronb/gbp012
Mills, S. D., Fox, R. S., Bohan, S., Roesch, S. C., Sadler, G. R., & Malcarne, V. L. (2020). Psychosocial and neighborhood correlates of health-related quality of life: A multi-level study among Hispanic adults. Cultural Diversity and Ethnic Minority Psychology, 26(1), 1–10. https://doi.org/10.1037/cdp0000274
Sellers, S. L., Cherepanov, D., Hanmer, J., Fryback, D. G., & Palta, M. (2013). Interpersonal discrimination and health-related quality of life among black and white men and women in the United States. Quality of Life Research, 22(6), 1313–1318. https://doi.org/10.1007/s11136-012-0278-4
Twardzik, E., Clarke, P., Elliott, M. R., Haley, W. E., Judd, S., & Colabianchi, N. (2019). Neighborhood socioeconomic status and trajectories of physical health-related quality of life among stroke survivors. Stroke, 50(11), 3191–3197. https://doi.org/10.1161/strokeaha.119.025874
Committee on Educating Health Professionals to Address the Social Determinants of Health; Board on Global Health; Institute of Medicine; National Academies of Sciences, Engineering, and Medicine. A framework for educating health professionals to address the social determinants of health. Washington (DC): National Academies Press (US); 2016 Oct 14. 3, Frameworks for addressing the social determinants of health. Available from: https://www.ncbi.nlm.nih.gov/books/NBK395979/
World Health Organization. (2010). A conceptual framework for action on the social determinants of health: debates, policy & practice, case studies. In A conceptual framework for action on the social determinants of health: debates, policy & practice, case studies. Geneva.
Brooks, R. G., Rabin, R., & Charro, F. D. (2010). The measurement and valuation of health status using Eq-5D: a European perspective: Evidence from the EuroQol Biomed Research Programme. Dordrecht: Kluwer Academic Publishers.
Pickard, A., Law, E., Jiang, R., Oppe, M., Shaw, J., Xie, F., … Balch, A. (2019). United States valuation of EQ-5D-5L health states: an initial model using a standardized protocol. Value in Health, 22(8), 931–941. doi:10.1016/j.jval.2019.02.009
Feeny, D., Torrance, G. W., & Furlong, W. (1996). Health Utilities Index. In B. Spilker (Ed.), Quality of life and pharmacoeconomics in clinical trials (2nd ed., pp. 239–252). Philadelphia: Lippincott-Raven Press.
Feeny, D., Furlong, W., Torrance, G.W., Goldsmith, C.H., Zhu, Z., Depauw, S., … Boyle, M. (2002). Multiattribute and single-attribute utility functions for the Health Utilities Index Mark 3 System. Medical Care, 40(2), 113–128. doi:10.1097/00005650-200202000-00006
Brazier, J. E., & Roberts, J. (2004). The estimation of a preference-based measure of health from the SF-12. Medical Care, 42(9), 851–859. https://doi.org/10.1097/01.mlr.0000135827.18610.0d
Hanmer, J., Feeny, D., Fischhoff, B., Hays, R.D., Hess, R., Pilkonis, P.A., … Yu, L. (2015). The PROMIS of QALYs. Health and Quality of Life Outcomes, 13(1). doi:https://doi.org/10.1186/s12955-015-0321-6
Cella, D., Yount, S., Rothrock, N., Gershon, R., Cook, K., Reeve, B., … Rose, M. (2007). The Patient-Reported Outcomes Measurement Information System (PROMIS). Medical Care, 45(Suppl 1). doi:https://doi.org/10.1097/01.mlr.0000258615.42478.55
Embretson, S. E., & Reise, S. P. (2013). Item response theory. New York: Psychology Press. https://doi.org/10.4324/9781410605269
Dewitt, B., Feeny, D., Fischhoff, B., Cella, D., Hays, R.D., Hess, R., … Hanmer, J. (2018). Estimation of a preference-based summary score for the Patient-Reported Outcomes Measurement Information System: The PROMIS®-Preference (PROPr) scoring system. Medical Decision Making, 38(6), 683–698. doi:10.1177/0272989x18776637
Hanmer, J., Dewitt, B., Yu, L., Tsevat, J., Roberts, M., Revicki, D., … Cella, D. (2018). Cross-sectional validation of the PROMIS-Preference scoring system. Plos One, 13(7). doi:https://doi.org/10.1371/journal.pone.0201093
NORC . N.d. “AmeriSpeak: NORC’s Breakthrough Panel-Based Research Platform”. Retrieved April 13, 2020. https://amerispeak.norc.org/Pages/default.aspx
Hanmer, J. Developing the PROMIS-preference score for monitoring population health outcomes. https://osf.io/63548/.
Hanmer, J., Cella, D., Feeny, D., Fischhoff, B., Hays, R.D., Hess, R., … Yu, L. (2017). Selection of key health domains from PROMIS® for a generic preference-based scoring system. Quality of Life Research, 26(12), 3377–3385. doi: 10.1007/s11136-017-1686-2
Hanmer, J., Cella, D., Feeny, D., Fischhoff, B., Hays, R. D., Hess, R., … Yu, L. (2018). Evaluation of options for presenting health-states from PROMIS® item banks for valuation exercises. Quality of Life Research, 27(7), 1835–1843. doi:10.1007/s11136-018-1852-1
Stolk, E., Ludwig, K., Rand, K., Hout, B. V., & Ramos-Goñi, J. M. (2019). Overview, update, and lessons learned from the International EQ-5D-5L valuation work: Version 2 of the EQ-5D-5L valuation protocol. Value in Health, 22(1), 23–30. https://doi.org/10.1016/j.jval.2018.05.010
-Item Short Form Survey from the RAND Medical Outcomes Study. (n.d.). Retrieved April 13, 2020. https://www.rand.org/health-care/surveys_tools/mos/12-item-short-form.html
NHIS - Questionnaires, Datasets, and Related Documentation. (2019). Retrieved April 13, 2020, from https://www.cdc.gov/nchs/nhis/nhis_questionnaires.htm
NHANES - National Health and Nutrition Examination Survey Homepage. (2020). Retrieved April 13, 2020, from https://www.cdc.gov/nchs/nhanes/index.htm
US Census Bureau. (2020). American Community Survey (ACS). Retrieved April 13, 2020, from https://www.census.gov/programs-surveys/acs/
Air Quality System (AQS). (2020). Retrieved April 13, 2020, from https://www.epa.gov/aqs
Uniform Crime Reporting (UCR) Program. (2018). Retrieved April 13, 2020, from https://www.fbi.gov/services/cjis/ucr
Evans, J. D. (1996). Straightforward statistics for the behavioral sciences. Pacific Grove, CA: Brooks/Cole Publishing Company.
Feeny, D. H., & Torrance, G. W. (1989). Incorporating utility-based quality-of-life assessment measures in clinical trials: Two examples. Medical Care, 27(S3), 190-S204. https://doi.org/10.1097/00005650-198903001-00016
Wolowacz, S. E., Briggs, A., Belozeroff, V., Clarke, P., Doward, L., Goeree, R., et al. (2016). Estimating health-state utility for economic models in clinical studies: An ISPOR good research practices task force report. Value in Health, 19(6), 704–719. https://doi.org/10.1016/j.jval.2016.06.001
Neumann, P.J., Sanders, G.D., Russell, L.B., Siegel, J.E. and Ganiats, T.G. eds. (2016). Cost-effectiveness in health and medicine. Oxford University Press. doi: 10.1093/acprof:oso/9780190492939.003
Fryback, D. G., Palta, M., Cherepanov, D., Bolt, D., & Kim, J. S. (2010). Comparison of 5 health-related quality-of-life indexes using item response theory analysis. Medical Decision Making, 30(1), 5–15. https://doi.org/10.1177/0272989X09347016
Liu, H., Cella, D., Gershon, R., Shen, J., Morales, L. S., Riley, W., & Hays, R. D. (2010). Representativeness of the patient-reported outcomes measurement information system internet panel. Journal of Clinical Epidemiology, 63(11), 1169–1178. https://doi.org/10.1016/j.jclinepi.2009.11.021
Hanmer, J., Cherepanov, D., Palta, M., Kaplan, R. M., Feeny, D., & Fryback, D. G. (2016). Health condition impacts in a nationally representative cross-sectional survey vary substantially by preference-based health index. Medical Decision Making, 36(2), 264–274. https://doi.org/10.1177/0272989x15599546
Tengs, T. O., & Wallace, A. (2000). One thousand health-related quality-of-life estimates. Medical Care, 38(6), 583–637. https://doi.org/10.1097/00005650-200006000-00004
Mcdonough, C. M., & Tosteson, A. N. A. (2007). Measuring preferences for cost-utility analysis. PharmacoEconomics, 25(2), 93–106. https://doi.org/10.2165/00019053-200725020-00003
Acknowledgements
I would like to extend my thanks to the participants in the survey without whom this work would not be possible. This work was supported by the Robert Wood Johnson Foundation (ID 74695).
Funding
This work was supported by the Robert Wood Johnson Foundation (ID 74695).
Author information
Authors and Affiliations
Contributions
JH was solely responsible for the study concept and design, acquisition of data, analysis and interpretation of data, drafting and revising, and final approval of the article to be published.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Consent to participate
Voluntary consent was obtained before participants could proceed to the survey, and participants were free to withdraw their participation at any time.
Consent for publication
The author hereby gives consent for publication this article in Quality of Life Research.
Ethical approval
University of Pittsburgh IRB PRO17080294.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hanmer, J. Cross-sectional validation of the PROMIS-Preference scoring system by its association with social determinants of health. Qual Life Res 30, 881–889 (2021). https://doi.org/10.1007/s11136-020-02691-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02691-3