Abstract
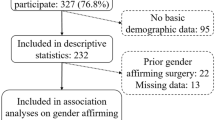
A key priority of transgender health research is the evaluation of long-term effects of gender affirmation treatment. Thus, accurate assessment of treatment receipt is critical. The data for this analysis came from an electronic medical records (EMR) based cohort of transgender individuals. A subset of cohort members were also asked to complete a self-administered survey. Information from the EMR was compared with survey responses to assess the extent of agreement regarding transmasculine (TM)/transfeminine (TF) status, hormone therapy receipt, and type of surgery performed. Logistic regression models were used to assess whether participant characteristics were associated with disagreement between data sources. Agreement between EMR and survey-derived information was high regarding TM/TF status (99%) and hormone therapy receipt (97%). Lower agreement was observed for chest reconstruction surgery (72%) and genital reconstruction surgery (84%). Using survey responses as the “gold standard”, both chest and genital reconstruction surgeries had high specificity (95 and 93%, respectively), but the corresponding sensitivities were low (49 and 68%, respectively). A lower proportion of TM had concordant results for chest reconstruction surgery (64% versus 79% for TF) while genital reconstruction surgery concordance was lower among TF (79% versus 89% for TM). For both surgery types, agreement was highest among the youngest participants. Our findings offer assurance that EMR-based data appropriately classify cohort participants with respect to their TM/TF status or hormone therapy receipt. However, current EMR data may not capture the complete history of gender affirmation surgeries. This information is useful in future studies of outcomes related to gender affirming therapy.
Similar content being viewed by others
References
Institute of Medicine. The health of lesbian, gay, bisexual, and transgender people: building a foundation for better understanding. Washington, DC: The National Academies Press; 2011.
Feldman J, Brown GR, Deutsch MB, Hembree W, Meyer W, Meyer-Bahlburg HFL, et al. Priorities for transgender medical and healthcare research. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):180–7.
Reisner SL, Deutsch MB, Bhasin S, Bockting W, Brown GR, Feldman J, et al. Advancing methods for US transgender health research. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):198–207.
Reisner SL, Poteat T, Keatley JA, Cabral M, Mothopeng T, Dunham E, et al. Global health burden and needs of transgender populations: a review. Lancet. 2016;388(10042):412–36.
Newell SA, Girgis A, Sanson-Fisher RW, Savolainen NJ. The accuracy of self-reported health behaviors and risk factors relating to cancer and cardiovascular disease in the general population: a critical review. Am J Prev Med. 1999;17(3):211–29.
Deutsch MB, Buchholz D. Electronic health records and transgender patients--practical recommendations for the collection of gender identity data. J Gen Intern Med. 2015;30(6):843–7.
Roblin D, Barzilay J, Tolsma D, Robinson B, Schild L, Cromwell L, et al. A novel method for estimating transgender status using electronic medical records. Ann Epidemiol. 2016;26(3):198–203.
Gardner IH, Safer JD. Progress on the road to better medical care for transgender patients. Curr Opin Endocrinol Diabetes Obes. 2013;20(6):553–8.
Quinn VP, Nash R, Hunkeler E, Contreras R, Cromwell L, Becerra-Culqui TA, et al. Cohort profile: study of transition, outcomes and gender (STRONG) to assess health status of transgender people. BMJ Open. 2017;7(12):e018121.
Cahill S, Singal R, Grasso C, King D, Mayer K, Baker K, et al. Do ask, do tell: high levels of acceptability by patients of routine collection of sexual orientation and gender identity data in four diverse American community health centers. PLoS One. 2014;9(9):e107104.
Goodman M, Steenland NK, Almon ML, Liff JS, Dilorio CK, Butler SO, et al. Prostate cancer treatment ascertained from several sources: analysis of disagreement and error. Ann Oncol. 2012;23(1):256–63.
Owen-Smith AA, Gerth J, Sineath RC, Barzilay J, Becerra-Culqui TA, Getahun D, et al. Association between gender confirmation treatments and perceived gender congruence, body image satisfaction, and mental health in a cohort of transgender individuals. J Sex Med. 2018;15:591–600.
Sineath RC, Woodyatt C, Sanchez T, Giammattei S, Gillespie T, Hunkeler E, et al. Determinants of and barriers to hormonal and surgical treatment receipt among transgender people. Transgend Health. 2016;1(1):129–36.
Berry MG, Curtis R, Davies D. Female-to-male transgender chest reconstruction: a large consecutive, single-surgeon experience. J Plast Reconstr Aesthet Surg. 2012;65(6):711–9.
Cregten-Escobar P, Bouman MB, Buncamper ME, Mullender MG. Subcutaneous mastectomy in female-to-male transsexuals: a retrospective cohort-analysis of 202 patients. J Sex Med. 2012;9(12):3148–53.
Spack NP. Management of transgenderism. JAMA. 2013;309(5):478–84.
Wroblewski P, Gustafsson J, Selvaggi G. Sex reassignment surgery for transsexuals. Curr Opin Endocrinol Diabetes Obes. 2013;20(6):570–4.
Zhao JJ, Marchaim D, Palla MB, Bogan CW, Hayakawa K, Tansek R, et al. Surgical site infections in genital reconstruction surgery for gender reassignment, Detroit: 1984-2008. Surg Infect. 2014;15(2):99–104.
Acknowledgements
This work would not be possible without continuous support and advice from the Stakeholder Advisory Group, which included representatives of the transgender community and health care providers and researchers who work with transgender people. We thank Dr. Lemuel Arnold, Dr. Nancy Baisch, Dr. John Blosnich, Dr. George Brown, Dr. Robin Dea, Ms. Cheryl Courtney-Evans, Dr. Shawn Giammattei, Ms. Monica Helms, Ms. Cadence Valentine, Mr. Willy Wilkinson, Ms. Savannah Winter and Mr. Evan Young for their valuable input and willingness to collaborate with us.
Funding
This research was supported by the Contract AD-12-11-4532 from the Patient Centered Outcome Research Institute and by the Grant R21HD076387 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors report competing interests.
Rights and permissions
About this article
Cite this article
Gerth, J., Becerra-Culqui, T., Bradlyn, A. et al. Agreement between medical records and self-reports: Implications for transgender health research. Rev Endocr Metab Disord 19, 263–269 (2018). https://doi.org/10.1007/s11154-018-9461-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-018-9461-4