Abstract
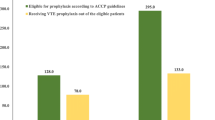
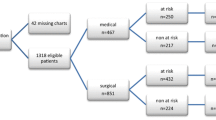
Background Venous thromboembolism (VTE) is a major cause of death among hospitalized patients. Many VTE prophylaxis guidelines have been developed, including the American College of Chest Physicians (ACCP). VTE prophylaxis is required in specific patients; however, its practice is not always optimal, and often depends on the hospitals’ protocols. In Lebanon, information about the appropriateness of VTE prophylaxis in health care centers is lacking. Objective The primary objective of this study was to evaluate the pattern of VTE prophylaxis application, including agents, doses, duration of treatment, and route of administration, in Lebanese health care centers. Methods A Lebanese multi-center, prospective, chart review study was conducted over 4 months. Data on demographics, VTE prophylaxis medication, dose, route, duration, and associated risk factors were collected by pharmacy students. The appropriateness of VTE prophylaxis was determined as per ACCP guidelines. Patients receiving VTE treatment were excluded from the study. Institutional review board (IRB) approval was obtained from each hospital center. Results A total of 840 patients were included. Both gender groups were equally represented in the sample and the mean age was 59 ± 19.53 years. The majority (639/840, 76.1%) of the sample were at high risk for deep venous thrombosis (DVT), and inappropriate VTE prophylaxis was reported in 35% of the low-risk group, in 70% of the moderate-risk group, and in 39% of the high-risk group (P < 0.0001). Comparing proper VTE prophylaxis practice between intensive care unit (ICU) and non-ICU patients, there was no statistical difference observed in teaching hospitals (67.2% vs. 65.5%, P = 0.312). However, in non-teaching hospitals, appropriate VTE prophylaxis practice was more prevalent in ICU than non-ICU patients (65.9% vs. 51.2%, P = 0.004). The average duration of VTE prophylaxis was less than 10 days. Missing data was a major limitation for this study, where, for instance, the duration of prophylaxis could not be accurately abstracted in half of the sample. Another limitation was the absence of laboratory results needed for clinical assessment of the regimen used. Conclusion This study reflected the importance of assessing VTE prophylaxis in Lebanese hospitals, thus, the need for implementing established guidelines to improve the overall patient safety.
Similar content being viewed by others
References
Anderson FA Jr, Wheeler HB, Goldberg RJ et al (1992) The prevalence of risk factors for venous thromboembolism among hospital patients. Arch Intern Med 152:1660–1664. doi:10.1001/archinte.152.8.1660
Samama CM (2001) Venous thromboembolism deserves your attention. Crit Care 5:277–279. doi:10.1186/cc1046
Hacking N, Hellewell A, Sadler P (2006) Prevention of deep vein thrombosis and pulmonary embolus. Anaesth Intensive Care Med 7(12):449–452. doi:10.1053/j.mpaic.2006.09.010
White RH (2003) The epidemiology of venous thromboembolism. Circulation 107(23 Suppl 1):I4–I8
Alonso Ortiz del Rio C, Medrano Ortega FJ, Romero Alonso A, Villar Conde E, Calderon Sandubete E, Marin Leon I et al. Prevention of thromboembolic venous disease in medical patients. 1998–2007 National Guideline Clearinghouse
Scottish Intercollegiate Guidelines Network (SIGN) (2002) Prophylaxis of venous thromboembolism. A national clinical guideline. SIGN, Edinburgh, Scotland; Oct 2002, 47 p. SIGN publication, no. 62, [214 references]. 1998–2007 National Guideline Clearinghouse
Joint Commission on Accreditation of Healthcare Organizations/National Quality Forum (2004) Joint Commission, National Quality Forum to work on deep vein thrombosis prevention and care project, vol 85(3), pp 607–624
Marr WL (2006) Deep venous thrombosis recommendations. J Vasc Nurs 24(3):91–93. doi:10.1016/j.jvn.2006.06.013
Geerts WH, Pineo GF, Heit JA et al (2004) Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 126(3 Suppl):338S–400S. doi:10.1378/chest.126.3_suppl.338S
Geerts WH, Heit JA, Clagett GP et al (2001) Prevention of venous thromboembolism. Chest 119:132S–175S. doi:10.1378/chest.119.1_suppl.132S
Mant M (2004) Clinical guide—DVT prophylaxis in orthopedics. The Thrombosis Interest Group of Canada. Home page at: http://www.tigc.org. Accessed April 2008
Anonymous (2007) Venous thromboembolism: reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in inpatients undergoing surgery. National Institute for Health and Clinical Excellence (NICE) clinical guideline 46
Gnanalingham KK (2003) Attitudes to the use of prophylaxis for thrombo-embolism in neurosurgical patients. J Clin Neurosci 10(4):467–469. doi:10.1016/S0967-5868(03)00060-2
Hull RD, Pineo GF, Stein PD et al (2001) Extended out-of-hospital low-molecular-weight heparin prophylaxis against deep venous thrombosis in patients after elective hip arthroplasty: a systematic review. Ann Intern Med 135:858–869
Koda-Kimble MA, Young LY, Kradjan WA, Guglielmo BJ, Alldredge BK, Corelli RL (2005) Applied therapeutics: the clinical use of drugs, 8th edn. Thrombosis Chap 16:1–25
Bates SM, Ginsberg JS (2004) Clinical practice. Treatment of deep-vein thrombosis. N Engl J Med 351:268–277. doi:10.1056/NEJMcp031676
Caprini JA, Tapson VF, Hyers TM et al (2005) Treatment of venous thromboembolism: adherence to guidelines and impact of physician knowledge, attitudes, and beliefs. J Vasc Surg 42(4):726–733. doi:10.1016/j.jvs.2005.05.053
Brunto L, Lazo J, Parker K (2005) Goodman and Gilman’s the pharmacological basis of therapeutics, 11th edn. Blood coagulation and anticoagulant, thrombolytic, and antiplatelet drugs. Chap 54, pp 1467–1486
Kleinbart J, Williams MV, Rask K. Chapter 31: prevention of venous thromboembolism. Available online at: http://www.ahcpr.gov/clinic/ptsafety/chap31a.htm. Accessed April 2008
Heit JA (2003) Risk factors for venous thromboembolism. Clin Chest Med 24:1–12. doi:10.1016/S0272-5231(02)00077-1
Haas SK (2002) Venous thromboembolic risk and its prevention in hospitalized medical patients. Semin Thromb Hemost 28:577–584. doi:10.1055/s-2002-36702
Risk assessment tool: are you at risk for DVT? Illinois State Medical Society. Home page at: http://www.isms.org
McCaffrey R, Bishop M, Adonis-Rizzo M et al (2007) Development and testing of a DVT risk assessment tool: providing evidence of validity and reliability. Worldviews Evid Based Nurs 4(1):14–20. doi:10.1111/j.1741-6787.2007.00074.x
The coalition to prevent deep venous thrombosis. DVT risk assessment tool. 2007 sanofi-aventis
Caprini JA, Arcelus JI, Reyna JJ (2001) Effective risk stratification of surgical and nonsurgical patients for venous thromboembolic disease. Semin Hematol 38(2 Suppl 5):12–19. doi:10.1053/shem.2001.25184
Second Thromboembolic Risk Factors (THRIFT II) Consensus Group (1998) Risk of and prophylaxis for venous thromboembolism in hospital patients. Phlebology 13:87–97
Thromboembolic Risk Factors (THRIFT) Consensus Group (1992) Risk of and prophylaxis for venous thromboembolism in hospital patients. BMJ 305:567–574
Aldrich D, Hunt DP (2004) When can the patient with deep venous thrombosis begin to ambulate? Phys Ther 84:268–273
Blättler W, Partsch H (2003) Leg compression and ambulation is better than bed rest for the treatment of acute deep venous thrombosis. Int Angiol 22:393–400
Partsch H (2001) Therapy of deep vein thrombosis with low molecular weight heparin, leg compression and immediate ambulation. Vasa—J Vascular Dis 30:195–204
Partsch H, Blättler W (2000) Compression and walking versus bed rest in the treatment of proximal deep venous thrombosis with low molecular weight heparin. J Vasc Surg 32:861–869. doi:10.1067/mva.2000.110352
Amaragiri SV, Lees TA (2000) Elastic compression stockings for prevention of deep vein thrombosis. Cochrane Database Syst Rev (1). doi:10.1002/14651858.CD001484
Agu O, Hamilton G, Baker D (1999) Graduated compression stockings in the prevention of venous thromboembolism. Br J Surg 86(8):992–1004. doi:10.1046/j.1365-2168.1999.01195.x
Francis CW (2007) Clinical practice. Prophylaxis for thromboembolism in hospitalized medical patients. N Engl J Med 356:1438–1444. doi:10.1056/NEJMcp067264
Leizorovicz A, Mismetti P (2004) Preventing venous thromboembolism in medical patients. Circulation 110:IV13–IV19. doi:10.1161/01.CIR.0000150640.98772.af
Hull RD, Raskob GE, Gent M et al (1990) Effectiveness of intermittent pneumatic leg compression for preventing deep vein thrombosis after total hip replacement. JAMA 263:2313–2317. doi:10.1001/jama.263.17.2313
Holzheimer RG (2004) Prophylaxis of thrombosis with low-molecular-weight heparin (LMWH). Eur J Med Res 9:150–170
Aventis (2004) Lovenox® (enoxaparin sodium injection) prescribing information. Aventis Pharmaceuticals Inc., Bridgewater, NJ
McGarry LJ, Stokes ME, Thompson D (2006) Outcomes of thromboprophylaxis with enoxaparin vs. unfractionated heparin in medical inpatients. Thromb J 4:17. doi:10.1186/1477-9560-4-17
Rydberg EJ, Westfall JM, Nicholas RA (1999) Low-molecular-weight heparin in preventing and treating DVT. Am Fam Physician 59(6):1607–1612
Baglin TP, Keeling DM, Watson HG; British Committee for Standards in Haematology (2006) Guidelines on oral anticoagulation (warfarin): third edition—2005 update. Br J Haematol 132(3):277–285. doi:10.1111/j.1365-2141.2005.05856.x
Horton JD, Bushwick BM (1999) Warfarin therapy: evolving strategies in anticoagulation. Am Fam Physician 59(3):635–646
Spinler SA, Dobesh P (2005) Dose capping enoxaparin is unjustified and denies patients with acute coronary syndromes a potentially effective treatment. Chest 127:2288–2290. doi:10.1378/chest.127.6.2288
Mitsuyasu RT (2004) Adjusting enoxaparin by weight for DVT prophylaxis. Medscape Crit Care 5(2). Available online at: http://www.medscape.com/viewarticle/488078
Royal Darwin Hospital. Venous thromboembolism prophylaxis guidelines
Lacut K, Bressollette L, Le Gal G et al (2005) Prevention of venous thrombosis in patients with acute intracerebral hemorrhage. Neurology 65(6):865–869. doi:10.1212/01.wnl.0000176073.80532.a2
Bergqvist D, Agnelli G, Cohen AT et al (2002) Duration of prophylaxis against venous thromboembolism with enoxaparin after surgery for cancer. N Engl J Med 346:975–980. doi:10.1056/NEJMoa012385
Kanaan AO, Silva MA, Donovan JL et al (2007) Meta-analysis of venous thromboembolism prophylaxis in medically ill patients. Clin Ther 29(11):2395–2405. doi:10.1016/j.clinthera.2007.11.015
Cohen AT, Alikhan R (2001) Prophylaxis of venous thromboembolism in medical patients. Curr Opin Pulm Med 7:332–337. doi:10.1097/00063198-200109000-00014
Ageno W, Turpie AG (2005) What’s new for DVT prophylaxis for the medically ill. Dis Mon 51(2–3):194–199. doi:10.1016/j.disamonth.2005.03.015
Mismetti P, Laporte-Simitsidis S, Tardy B et al (2000) Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a meta-analysis of randomised clinical trials. Thromb Haemost 83:14–19
Clagett GP, Anderson FA, Heit J et al (1995) Prevention of venous thromboembolism. Chest 108:313S–334S
Khouli H, Shapiro J, Pham VP et al (2006) Efficacy of deep venous thrombosis prophylaxis in the medical intensive care unit. J Intensive Care Med 21(6):352–358. doi:10.1177/0885066606292880
Cook D, Meade M, Guyatt G et al (2004) Clinically important deep vein thrombosis in the intensive care unit: a survey of intensivists. Crit Care 8(3):R145–R152. doi:10.1186/cc2859
Todi SK, Sinha S, Chakraborty A et al (2003) Utilisation of deep venous thrombosis prophylaxis in medical/surgical intensive care units. Indian J Crit Care Med 7(2):103–105
Geerts W, Cook D, Selby R et al (2002) Venous thromboembolism and its prevention in critical care. J Crit Care 17(2):95–104. doi:10.1053/jcrc.2002.33941
Geerts W, Selby R (2003) Prevention of venous thromboembolism in the ICU. Chest 124(Suppl 6):357S–363S. doi:10.1378/chest.124.6_suppl.357S
Vincent J, Esteban A, Cook DJ et al (2000) Venous thromboembolism in the ICU: what is the epidemiology and what are the consequences? Update in Intensive Care Medicine, pp 45–50
Shorr AF, Jackson WL Jr (2005) Deep vein thrombosis in the intensive care unit: underappreciated, understudied, and undertreated. J Crit Care 20(4):301–303. doi:10.1016/j.jcrc.2005.08.003
Attia J, Ray JG, Cook DJ et al (2001) Deep vein thrombosis and its prevention in critically ill adults. Arch Intern Med 161(10):1268–1279. doi:10.1001/archinte.161.10.1268
Marik PE, Andrews L, Maini B (1997) The incidence of deep venous thrombosis in ICU patients. Chest 111:661–664. doi:10.1378/chest.111.3.661
Rubin A, Dinan W, Klapholz A et al (2006) Assessment of adequacy of deep venous thrombosis (DVT) prophylaxis in patients with hospital-acquired DVT in a community teaching hospital; Cabrini Medical Center, New York, NY. Chest 130(4):259S
Masroujeh R, Shamseddeen W, Isma’eel H et al (2008) Underutilization of venous thromboemoblism prophylaxis in medical patients in a tertiary care center. J Thromb Thrombolysis 26:138–141. doi:10.1007/s11239-007-0084-y
Mazboudi O, Lababidi HM (2007) Current trends of prophylaxis for deep vein thrombosis in a tertiary care hospital in Lebanon. Chest 132:630S
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zeitoun, A.A., Dimassi, H.I., El Kary, D.Y. et al. An evaluation of practice pattern for venous thromboembolism prevention in Lebanese hospitals. J Thromb Thrombolysis 28, 192–199 (2009). https://doi.org/10.1007/s11239-008-0298-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-008-0298-7