Abstract
Purpose
The aim of this study was to evaluate the effectiveness of inspiratory muscle training (IMT) on sleep and functional capacity to exercise in subjects with obstructive sleep apnea (OSA).
Methods
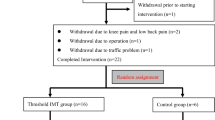
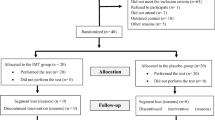
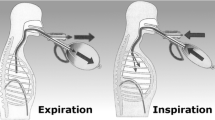
This is a controlled, randomized, double-blind study conducted in 16 OSA patients divided into two groups: training (IMT: n = 8) and placebo-IMT (P-IMT: n = 8). IMT was conducted during 12 weeks with a moderate load (50–60% of maximal inspiratory pressure—MIP), while P-IMT used a load < 20% of MPI. Total daily IMT time for both groups was 30 min, 7 days per week, twice a day.
Results
There was no difference comparing IMT to P-IMT group after training for lung function (p > 0.05) and respiratory muscle strength (p > 0.05). Maximal oxygen uptake (VO2Max) was not significantly different between IMT and P-IMT group (mean difference − 1.76, confidence interval (CI) − 7.93 to 4.41, p = 0.71). The same was observed for the other ventilatory and cardiometabolic variables measured (p > 0.05). A significant improvement in sleep quality was found when Pittsburgh Sleep Quality Index (PSQI) values of IMT and P-IMT group after training were compared (mean difference: 3.7, confidence interval 95% (CI95%) 0.6 to 6.9, p = 0.02) but no significant changes were seen in daytime sleepiness between both groups after the intervention (mean difference: 3.4, CI 95%: − 3.3 to 10.0; p = 0.29).
Conclusion
According to these results, 12 weeks of moderate load IMT resulted in improved sleep quality, but there were no significant repercussions on functional capacity to exercise or excessive daytime sleepiness.

Similar content being viewed by others
References
Jackson MJ, O'Farrell S (1993) Free radicals and muscle damage. Br Med Bull 49(3):630–641
Bradley TD, Floras J (2009) Obstructive sleep apnea and its cardiovascular consequences. Lancet 373(9657):82–93. https://doi.org/10.1016/S0140-6736(08)61622-0
Rizzi CF, Cintra F, Risso T, Pulz C, Tufik S, de Paola A, Poyares D (2010) Exercise capacity and obstructive sleep apnea in lean subjects. Chest 137(1):109–114. https://doi.org/10.1378/chest.09-1201
Chien MY, YT W, Lee PL, Chang YJ, Yang PC (2010) Inspiratory muscle dysfunction in patients with severe obstructive sleep apnoea. Eur Respir J 35(2):373–380. https://doi.org/10.1183/09031936.00190208
Deacon N, Jen R, Li Y, Malhotra A (2016) Treatment of obstructive sleep apnea. Prospects for personalized combined modality therapy. Ann Am Thorac Soc 13(1):101–108. https://doi.org/10.1513/AnnalsATS.201508-537FR
Kline CE, Crowley EP, Ewing GB, Burch JB, Blair SN, Durstine J, Davis JM, Youngstedt SD (2011) The effect of exercise training on obstructive sleep apnea and sleep quality: a randomized controlled trial. Sleep 34(12):1631–1640. https://doi.org/10.5665/sleep.1422
Iftikhar IH, Kline CE, Youngstedt SD (2014) Effects of exercise training on sleep apnea: a meta-analysis. Lung 192(1):175–184
Vranish JR, Bailey EF (2016) Inspiratory muscle training improves sleep and mitigates cardiovascular dysfunction in obstructive sleep apnea. Sleep 39(6):1179–1185
Hajghanbari B, Yamabayashi C, Buna TR, Coelho JD, Freedman KD, Morton TA, Palmer SA, Toy MA, Walsh C, Sheel AW, Reid WD (2013) Effects of respiratory muscle training on performance in athletes: a systematic review with meta-analyses. J Strength Cond Res 27(6):1643–1663
Bavarsad MB, Shariati A, Eidani E, Latifi M (2015) The effect of home-based inspiratory muscle training on exercise capacity, exertional dyspnea and pulmonary function in COPD patients. Iran J Nurs Midwifery Res 20(5):613–618. https://doi.org/10.4103/1735-9066.164588
Turner LA, Mickleborough TD, Mcconnell AK, Stager JM, Tecklenburg-Lund S, Lindley MR (2011) Effect of inspiratory muscle training on exercise tolerance in asthmatic individuals. Med Sci Sports Exerc 43(11):2031–2038. https://doi.org/10.1249/MSS.0b013e31821f4090
Corrêa AP, Ribeiro JP, Balzan FM, Mundstock L, Ferlin EL, Moraes RS (2011) Inspiratory muscle training in type 2 diabetes with inspiratory muscle weakness. Med Sci Sports Exerc 43(7):1135–1141. https://doi.org/10.1249/MSS.0b013e31820a7c12
Bertolazi AN, Fagondes SC, Hoff LS, Pedro VD, Barreto SSM, Johns MW (2009) Validação da escala de sonolência de Epworth em português para uso no Brasil. J Bras Pneumol 35(9):877–883
Bertolazi AN, Fagondes SC, Hoff LS, Dartora EG, Miozzo IC, de Barba ME, Barreto SS (2011) Validation of the Brazilian Portuguese version of the Pittsburgh Sleep Quality Index. Sleep Med 12(1):70–75. https://doi.org/10.1016/j.sleep.2010.04.020
Pessoa IM, Houri Neto M, Montemezzo D, Silva LAM, Andrade AD, Parreira VF (2014) Predictive equations for respiratory muscle strength according to international and Brazilian guidelines. Braz J Phys Ther 18(5):410–418
Pereira CA, Duarte AA, Gimenez A, Soares MR (2014) Comparison between reference values for FVC, FEV1, and FEV1/FVC ratio in White adults in Brazil and those suggested by the Global Lung Function Initiative 2012. J Bras Pneumol 40(4):397–402
Hill K, Cecins NM, Eastwood PR, Jenkins SC (2010) Inspiratory muscle training for patients with cronic obstructive pulmonar disease: a pratical guide for clinicians. Arch Phys Med Rehabil 91(9):1466–1470. https://doi.org/10.1016/j.apmr.2010.06.010
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D'Agostino RB, Newman AB, Lebowitz MD, Pickering TG (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study: Sleep Heart Health Study. JAMA 283(14):1829–1836
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342(19):1378–1384
Roehrs T, Zorick F, Wittig R, Conway W, Roth T (1989) Predictors of objective level of daytime sleepiness in patients with sleep-related breathing disorders. Chest 95(6):1202–1206
Lombardi C, Parati G, Cortelli P, Provini F, Vetrugno R, Plazzi G, Vignatelli L, Di Rienzo M, Lugaresi E, Mancia G, Montagna P, Castiglioni P (2008) Daytime sleepiness and neural cardiac modulation in sleep-related breathing disorders. J Sleep Res 17(3):263–270. https://doi.org/10.1111/j.1365-2869.2008.00659.x
Mendelson M, Lyons OD, Yadollahi A, Inami T, Oh P, Bradley TD (2016) Effects of exercise training on sleep apnoea in patients with coronary artery disease: a randomised trial. Eur Respir J 48(1):142–150. https://doi.org/10.1183/13993003.01897-2015
Gibbons RJ, Balady GJ, Beasley JW, Bricker JT, Duvernoy WF, Froelicher VF, Mark DB, Marwick TH, McCallister BD, Thompson PD Jr, Winters WL, Yanowitz FG, Ritchie JL, Gibbons RJ, Cheitlin MD, Eagle KA, Gardner TJ, Garson A Jr, Lewis RP, O'Rourke RA, Ryan TJ (1997) ACC/AHA guidelines for exercise testing: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee on exercise testing). J Am Coll Cardiol 30(1):260–231
Ferretti G (2014) Maximal oxygen consumption in healthy humans: theories and facts. Eur J Appl Physiol 114(10):2007–2036. https://doi.org/10.1007/s00421-014-2911-0
Chien MY, Lee P, Tsai YF, Yang PC, YT W (2012) C-reactive protein and heart rate recovery in middle-aged men with severe obstructive sleep apnea. Sleep Breath 16(3):629–637. https://doi.org/10.1007/s11325-011-0549-2
Rizzi CF, Cintra F, Mello-Fujita L, Rios LF, Mendonca ET, Feres MC, Tufik S, Poyares D (2013) Does obstructive sleep apnea impair the cardiopulmonary response to exercise? Sleep 36(4):547–553. https://doi.org/10.5665/sleep.2542
Edwards AM, Cooke CB (2004) Oxygen uptake kinetics and maximal aerobic power are unaffected by inspiratory muscle training in healthy subjects where time to exhaustion is extended. Eur J Appl Physiol 93(1–2):139–144
Edwards AM (2013) Respiratory muscle training extends exercise tolerance without concomitant change to peak oxygen uptake: physiological, performance and perceptual responses derived from the same incremental exercise test. Respirology 18(6):1022–1027. https://doi.org/10.1111/resp.12100
Amann M, Blain GM, Proctor LT, Sebranek JJ, Pegelow DF, Dempsey JA (2010) Group III and IV muscle afferents contribute to ventilatory and cardiovascular response to rhythmic exercise in humans. J Appl Physiol (1985) 109(4):966–976. https://doi.org/10.1152/japplphysiol.00462.2010
Gandevia SC (2001) Spinal and supraspinal factors in human muscle fatigue. Physiol Rev 81(4):1725–1789
Funding
The Coordination for the Improvement of Higher Education Personnel (CAPES) provided financial support in the form of data collection funding. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Souza, A.K.F., Dornelas de Andrade, A., de Medeiros, A.I.C. et al. Effectiveness of inspiratory muscle training on sleep and functional capacity to exercise in obstructive sleep apnea: a randomized controlled trial. Sleep Breath 22, 631–639 (2018). https://doi.org/10.1007/s11325-017-1591-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1591-5