Abstract
Purpose
Metabolic syndrome is a cluster of metabolic abnormalities including obesity, hypertension, hypertriglyceridemia, low high-density lipoprotein cholesterol, and hyperglycemia. Obstructive sleep apnea (OSA) is known to be associated with metabolic syndrome. However, it remains uncertain which sleep parameters of OSA are associated with metabolic syndrome. We aimed to clarify the relationship between sleep variables and the presence of metabolic syndrome in patients with OSA.
Methods
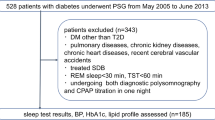
We prospectively recruited patients who visited the institute for the evaluation of sleep-disordered breathing. All patients underwent overnight polysomnography and sleep questionnaires. They were diagnosed with metabolic syndrome according to the 2007 consensus definition by the International Diabetes Federation. We applied multivariate logistic regression models to predict the presence of metabolic syndrome with variables related to sleep parameters.
Results
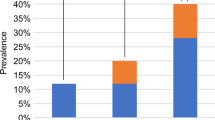
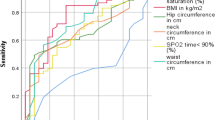
A total of 85 patients (43 men) were enrolled. The mean age (± standard deviation) was 52.0 ± 14.3 years. Metabolic syndrome was diagnosed in 39 (46%) patients. Patients with metabolic syndrome had a significantly higher apnea-hypopnea index (AHI) compared with patients without metabolic syndrome. An AHI greater than 15/h during REM sleep was a significant independent predictor of metabolic syndrome (adjusted OR, 7.08; 95% CI, 1.60–31.41; p = 0.010) after adjusting for age, body mass index, and non-REM AHI ≥ 15/h. In partial correlation analysis, REM AHI was significantly associated with the presence of metabolic syndrome after adjusting for age and BMI (r = 0.229, p = 0.042).
Conclusion
Korean patients with OSA frequently had comorbid metabolic syndrome. Moderate to severe OSA during REM sleep may be a predictor of metabolic syndrome.
Similar content being viewed by others
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235. https://doi.org/10.1056/NEJM199304293281704
Koo DL, Nam H, Thomas RJ, Yun CH (2018) Sleep disturbances as a risk factor for stroke. J Stroke 20(1):12–32. https://doi.org/10.5853/jos.2017.02887
Kostapanos MS, Mikhailidis DP, Elisaf MS, Steiropoulos P, Papanas N (2012) Obstructive sleep apnoea syndrome and cardiovascular risk. Arch Med Sci 8(6):1115–1116. https://doi.org/10.5114/aoms.2012.32425
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr, International Diabetes Federation Task Force on E, Prevention, National Heart L, Blood I, American Heart A, World Heart F, International Atherosclerosis S, International Association for the Study of O (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645. https://doi.org/10.1161/CIRCULATIONAHA.109.192644
Coughlin SR, Mawdsley L, Mugarza JA, Calverley PM, Wilding JP (2004) Obstructive sleep apnoea is independently associated with an increased prevalence of metabolic syndrome. Eur Heart J 25(9):735–741. https://doi.org/10.1016/j.ehj.2004.02.021
Somers VK, Dyken ME, Clary MP, Abboud FM (1995) Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest 96(4):1897–1904. https://doi.org/10.1172/JCI118235
Alzoubaidi M, Mokhlesi B (2016) Obstructive sleep apnea during rapid eye movement sleep: clinical relevance and therapeutic implications. Curr Opin Pulm Med 22(6):545–554. https://doi.org/10.1097/MCP.0000000000000319
Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MW (2011) The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath 15(3):377–384. https://doi.org/10.1007/s11325-010-0343-6
Hoddes E, Zarcone V, Smythe H, Phillips R, Dement WC (1973) Quantification of sleepiness: a new approach. Psychophysiology 10(4):431–436. https://doi.org/10.1111/j.1469-8986.1973.tb00801.x
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM, American Academy of Sleep M (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American Academy of sleep medicine. J Clin Sleep Med 8(5):597–619. https://doi.org/10.5664/jcsm.2172
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr., Spertus JA, Costa F, American Heart A, National Heart L, Blood I (2005) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation 112(17):2735–2752. https://doi.org/10.1161/CIRCULATIONAHA.105.169404
Acosta-Castro P, Hirotsu C, Marti-Soler H, Marques-Vidal P, Tobback N, Andries D, Waeber G, Preisig M, Vollenweider P, Haba-Rubio J, Heinzer R (2018) REM-associated sleep apnoea: prevalence and clinical significance in the HypnoLaus cohort. Eur Respir J 52 (2). doi:https://doi.org/10.1183/13993003.02484-2017
Ramachandran A, Snehalatha C, Satyavani K, Sivasankari S, Vijay V (2003) Metabolic syndrome in urban Asian Indian adults--a population study using modified ATP III criteria. Diabetes Res Clin Pract 60(3):199–204
Lam JC, Mak JC, Ip MS (2012) Obesity, obstructive sleep apnoea and metabolic syndrome. Respirology 17(2):223–236. https://doi.org/10.1111/j.1440-1843.2011.02081.x
Shechter A, Foster GD, Lang W, Reboussin DM, St-Onge MP, Zammit G, Newman AB, Millman RP, Wadden TA, Jakicic JM, Strotmeyer ES, Wing RR, Pi-Sunyer FX, Kuna ST, Sleep Ahead Research Group of the Look Ahead Research G (2017) Effects of a lifestyle intervention on REM sleep-related OSA severity in obese individuals with type 2 diabetes. J Sleep Res 26(6):747–755. https://doi.org/10.1111/jsr.12559
Lin QC, Zhang XB, Chen GP, Huang DY, Din HB, Tang AZ (2012) Obstructive sleep apnea syndrome is associated with some components of metabolic syndrome in nonobese adults. Sleep Breath 16(2):571–578. https://doi.org/10.1007/s11325-011-0544-7
Leinum CJ, Dopp JM, Morgan BJ (2009) Sleep-disordered breathing and obesity: pathophysiology, complications, and treatment. Nutr Clin Pract 24(6):675–687. https://doi.org/10.1177/0884533609351532
Somers VK, Dyken ME, Mark AL, Abboud FM (1993) Sympathetic-nerve activity during sleep in normal subjects. N Engl J Med 328(5):303–307. https://doi.org/10.1056/NEJM199302043280502
Grace KP, Hughes SW, Horner RL (2013) Identification of the mechanism mediating genioglossus muscle suppression in REM sleep. Am J Respir Crit Care Med 187(3):311–319. https://doi.org/10.1164/rccm.201209-1654OC
McSharry DG, Saboisky JP, Deyoung P, Jordan AS, Trinder J, Smales E, Hess L, Chamberlin NL, Malhotra A (2014) Physiological mechanisms of upper airway hypotonia during REM sleep. Sleep 37(3):561–569. https://doi.org/10.5665/sleep.3498
Findley LJ, Wilhoit SC, Suratt PM (1985) Apnea duration and hypoxemia during REM sleep in patients with obstructive sleep apnea. Chest 87(4):432–436
Krieger J, Sforza E, Boudewijns A, Zamagni M, Petiau C (1997) Respiratory effort during obstructive sleep apnea: role of age and sleep state. Chest 112(4):875–884
Peppard PE, Ward NR, Morrell MJ (2009) The impact of obesity on oxygen desaturation during sleep-disordered breathing. Am J Respir Crit Care Med 180(8):788–793. https://doi.org/10.1164/rccm.200905-0773OC
Mokhlesi B, Finn LA, Hagen EW, Young T, Hla KM, Van Cauter E, Peppard PE (2014) Obstructive sleep apnea during REM sleep and hypertension. Results of the Wisconsin sleep cohort. Am J Respir Crit Care Med 190(10):1158–1167. https://doi.org/10.1164/rccm.201406-1136OC
Appleton SL, Vakulin A, Martin SA, Lang CJ, Wittert GA, Taylor AW, McEvoy RD, Antic NA, Catcheside PG, Adams RJ (2016) Hypertension is associated with undiagnosed OSA during rapid eye movement sleep. Chest 150(3):495–505. https://doi.org/10.1016/j.chest.2016.03.010
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ, National Heart L, Blood Institute Joint National Committee on Prevention DE, Treatment of High Blood P, National High Blood Pressure Education Program Coordinating C (2003) The seventh report of the joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 289(19):2560–2572. https://doi.org/10.1001/jama.289.19.2560
Mokhlesi B, Hagen EW, Finn LA, Hla KM, Carter JR, Peppard PE (2015) Obstructive sleep apnoea during REM sleep and incident non-dipping of nocturnal blood pressure: a longitudinal analysis of the Wisconsin sleep cohort. Thorax 70(11):1062–1069. https://doi.org/10.1136/thoraxjnl-2015-207231
Tiihonen M, Partinen M, Narvanen S (1993) The severity of obstructive sleep apnoea is associated with insulin resistance. J Sleep Res 2(1):56–61
Ip MS, Lam B, Ng MM, Lam WK, Tsang KW, Lam KS (2002) Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med 165(5):670–676. https://doi.org/10.1164/ajrccm.165.5.2103001
Chami HA, Gottlieb DJ, Redline S, Punjabi NM (2015) Association between glucose metabolism and sleep-disordered breathing during REM sleep. Am J Respir Crit Care Med 192(9):1118–1126. https://doi.org/10.1164/rccm.201501-0046OC
Grimaldi D, Beccuti G, Touma C, Van Cauter E, Mokhlesi B (2014) Association of obstructive sleep apnea in rapid eye movement sleep with reduced glycemic control in type 2 diabetes: therapeutic implications. Diabetes Care 37(2):355–363. https://doi.org/10.2337/dc13-0933
Mokhlesi B, Grimaldi D, Beccuti G, Abraham V, Whitmore H, Delebecque F, Van Cauter E (2016) Effect of one week of 8-hour nightly continuous positive airway pressure treatment of obstructive sleep apnea on glycemic control in type 2 diabetes: a proof-of-concept study. Am J Respir Crit Care Med 194(4):516–519. https://doi.org/10.1164/rccm.201602-0396LE
Amin A, Ali A, Altaf QA, Piya MK, Barnett AH, Raymond NT, Tahrani AA (2017) Prevalence and associations of obstructive sleep apnea in south Asians and white Europeans with type 2 diabetes: a cross-sectional study. J Clin Sleep Med 13(4):583–589. https://doi.org/10.5664/jcsm.6548
Wen CP, David Cheng TY, Tsai SP, Chan HT, Hsu HL, Hsu CC, Eriksen MP (2009) Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr 12(4):497–506. https://doi.org/10.1017/S1368980008002802
Low S, Chin MC, Ma S, Heng D, Deurenberg-Yap M (2009) Rationale for redefining obesity in Asians. Ann Acad Med Singap 38(1):66–69
Funding
This research was supported by the Grant from the Seoul National University Hospital Research Fund (16-2014-85).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict(s) of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Additional information
Comment
This study finds an association between the metabolic syndrome and OSA during REM sleep, with an adjusted OR of 7.08, but no significant association with non-REM OSA. This study adds to the growing body of literature finding REM OSA to be associated with cardiometabolic outcomes. A study in a Caucasian population (HypnoLaus cohort) also found an association between REM OSA and metabolic syndrome. The lower OR in that study may have been due to the different ethnicity of participants but also to the population-based rather than clinical-based study design. Several particularities of REM OSA may account for greater impact on outcomes as discussed by authors, notably, often more marked hypoxemia.
Although analyses were adjusted for body mass index, BMI is a poor predictor of metabolic and cardiovascular complications. Rather, waist circumference, which reflects visceral fat, is much more predictive but was not adjusted for and remains a possible confounder in this study. Further studies in different populations will need to more clearly delineate the role of OSA itself, including related intermittent hypoxemia, sleep fragmentation and deprivation, autonomic activation, etc., on metabolic dysregulation. Could an interaction exist between increased visceral fat and intermittent hypoxemia? Treatment studies will be particularly important to help guide clinical practice. Should we be more aggressive in treating patients with lower overall AHI if REM AHI is ≥ 15/h?
Marta Kaminska
Montreal, Canada
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Koo, D., Kim, HR. & Nam, H. Moderate to severe obstructive sleep apnea during REM sleep as a predictor of metabolic syndrome in a Korean population. Sleep Breath 24, 1751–1758 (2020). https://doi.org/10.1007/s11325-019-02005-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-019-02005-z