Abstract
Background/objectives
Sleep disorders are highly prevalent in primary care. Obstructive sleep apnea (OSA) is one of the most common sleep disorders in the world, and it is estimated that only 10 to 20% of OSA cases are diagnosed. Primary care physicians (PCP) play an important role in screening for OSA. Knowledge of sleep disorders among PCP varies widely and has been generally reported as low. In this study, we aimed to assess the knowledge and attitudes towards OSA among primary care physicians in the Middle East and North Africa regions.
Methods
A cross-sectional study using the Obstructive Sleep Apnea Knowledge and Attitudes (OSAKA) self-administered questionnaire was distributed to PCP attending the Lebanese Society of Family Medicine annual conference, the Lebanese Society of Internal Medicine annual conference, and World Organization of Family Doctors (WONCA) East Mediterranean region conference.
Results
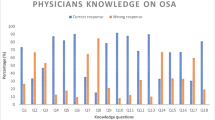
Of 300 physicians approached, 256 (85%) completed the questionnaires. The range of possible scores was 0 to 18. The mean total knowledge score with standard deviation (SD) was 12.6 (2.5). Internal medicine specialists showed a higher mean knowledge score of 14.1 (2.3) compared to general/family medicine specialists 12.4 (2.4) and other specialties 11.9 (2.8), p = 0.001. Though 78% of all physicians felt confident in identifying patients with OSA, only 26% felt confident in managing patients with continuous positive airway pressure. Overall, there was a weak positive correlation between knowledge and attitude.
Conclusion
There were gaps in knowledge and attitudes regarding managing patients with OSA. Training in managing patients with OSA is needed.
Similar content being viewed by others
References
Bielicki P, Pryć A, Witkowska A, Trojnar A, Wąsik M (2019) Disease characteristics and adherence to treatment with continous positive airway pressure in men and women severe obstructive sleep apnea (OSA). Eur Respiratory Soc 54:PA4161
WHO Chronic Disease Epidemics. World Health Organization website
Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, Hla KM (2009) Burden of sleep apnea: rationale, design, and major findings of the Wisconsin sleep cohort study. WMJ: official publication of the State Medical Society of Wisconsin 108(5):246–249
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, Hamilton GS, Dharmage SC (2017) Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev 34:70–81
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014
Al-Jahdali H (2012) Prevalence of sleep apnea and excessive day time sleepiness in patients with end-stage renal disease on dialysis. Saudi J Kidney Diseases Transplant 23(2):251
Mahboub B, Afzal S, Alhariri H, Alzaabi A, Vats M, Soans A (2013) Prevalence of symptoms and risk of sleep apnea in Dubai, UAE. Int J Gen Med 6:109
Khassawneh B, Ghazzawi M, Khader Y, Alomari M, Amarin Z, Shahrour B, Hammouda M (2009) Symptoms and risk of obstructive sleep apnea in primary care patients in Jordan. Sleep Breath 13(3):227–232
Stansbury RC, Strollo PJ (2015) Clinical manifestations of sleep apnea. J Thor Disease 7(9):E298
Bradley TD, Floras JS (2009) Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373(9657):82–93
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342(19):1378–1384
Redline S, Yenokyan G, Gottlieb DJ, Shahar E, O'Connor GT, Resnick HE, Diener-West M, Sanders MH, Wolf PA, Geraghty EM (2010) Obstructive sleep apnea–hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med 182(2):269–277
Reichmuth KJ, Austin D, Skatrud JB, Young T (2005) Association of sleep apnea and type II diabetes: a population-based study. Am J Respir Crit Care Med 172(12):1590–1595
McArdle N, Riha RL, Vennelle M, Coleman EL, Dennis MS, Warlow CP, Douglas NJ (2003) Sleep-disordered breathing as a risk factor for cerebrovascular disease: a case-control study in patients with transient ischemic attacks. Stroke 34(12):2916–2921
George CF (2007) Sleep apnea, alertness, and motor vehicle crashes. Am J Respir Crit Care Med 176(10):954–956
Miller JN, Berger AM (2016) Screening and assessment for obstructive sleep apnea in primary care. Sleep Med Rev 29:41–51
Billiart I, Ingrand P, Paquereau J, Neau J, Meurice J (2002) The sleep apnea syndrome: diagnosis and management in general practice. A descriptive survey of 579 French general practitioners. Rev Mal Respir 19(6):741–746
Chung SA, Jairam S, Hussain MR, Shapiro CM (2001) Knowledge of sleep apnea in a sample grouping of primary care physicians. Sleep Breath 5(03):115–122
Marran NM, Bahri AA, Kariri KI, Daghriri HM, Abiri JM, Kariri AM, Madkhali JM (2019) Recent medical graduates’ knowledge and attitude toward obstructive sleep apnea in the southern region of Saudi Arabia: a cross-sectional study. Egypt J Int Med 31(1):86
Chang J-WR, Akemokwe FM, Marangu DM, Chisunkha B, Irekpita E, Obasikene G, Kagima JW, Obonyo CO (2020) Obstructive sleep apnea awareness among primary care physicians in Africa. Ann Am Thor Soc 17(1):98–106
Gelir E, Ardiç S, İzci B (2004) A questionnaire survey among Turkish physicians about sleep disorders. Tuberk Toraks 52:348–355
Butt M, Dwivedi G, Khair O, Lip GY (2010) Obstructive sleep apnea and cardiovascular disease. Int J Cardiol 139(1):7–16
Kendzerska T, Mollayeva T, Gershon AS, Leung RS, Hawker G, Tomlinson G (2014) Untreated obstructive sleep apnea and the risk for serious long-term adverse outcomes: a systematic review. Sleep Med Rev 18(1):49–59
Schotland HM, Jeffe DB (2003) Development of the obstructive sleep apnea knowledge and attitudes (OSAKA) questionnaire. Sleep Med 4(5):443–450
Ojeda IC, Jeffe DB, Guerrero T, Mantilla R, Santoro I, Gabino G, Calderon JC, Caballero F, Mori J, Cherrez A (2013) Attitudes and knowledge about obstructive sleep apnea among Latin American primary care physicians. Sleep Med 14(10):973–977
Devaraj NK (2020) Knowledge, attitude, and practice regarding obstructive sleep apnea among primary care physicians. Sleep Breathing 1–10
Southwell C, Moallem M, Auckley D (2008) Cardiologist’s knowledge and attitudes about obstructive sleep apnea: a survey study. Sleep Breath 12(4):295–302
Corso RM, Sorbello M, Buccioli M, Carretta E, Nanni O, Piraccini E, Merli G, Petrini F, Guarino A, Frova G (2017) Survey of knowledge and attitudes about obstructive sleep apnoea among italian anaesthetists. Turk J Anesth Reanim 45(3):146–152
Author information
Authors and Affiliations
Contributions
HK and GA contributed to the study conception and design. HK performed the literature review and initial manuscript write-up. GA contributed to the literature review and initial manuscript write up. Data collection, analysis, and results write-up were performed by HK, HT, and RH. All the authors contributed to the discussion, critically reviewed, and advised on each draft. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the American University of Beirut Review Board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Al-Khafaji, H., Bilgay, I.B., Tamim, H. et al. Knowledge and attitude of primary care physicians towards obstructive sleep apnea in the Middle East and North Africa region. Sleep Breath 25, 579–585 (2021). https://doi.org/10.1007/s11325-020-02137-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02137-7