Abstract
Objectives
To examine the associations between four sleep behaviors and the risk of healthspan termination.
Methods
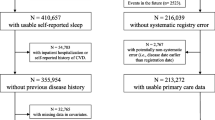
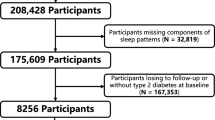
This study included 323,373 participants, free of terminated healthspan at baseline, from the UK-Biobank (UKB). We applied multivariable-adjusted Cox regression models to estimate the risk of terminated healthspan based on four sleep behaviors (insomnia/sleeplessness, napping, daytime sleepiness, and difficulty getting up from bed), which were self-reported and measured on Likert scales from “usually” to “never/rarely” experiences. In this study, healthspan was defined based on eight events that are strongly associated with longevity (congestive heart failure, myocardial infarction, chronic obstructive pulmonary disease, stroke, dementia, diabetes, cancer, and death).
Results
Participants who reported the following unhealthy sleep behaviors had a significantly higher risk of terminated healthspan: “usually experience sleeplessness/insomnia” (HR = 1.05, 95% CI: 1.03–1.07; P < 0.001); “usually nap” (HR = 1.22, 95% CI: 1.18–1.26; P < 0.01); “excessive daytime sleepiness” (HR = 1.25, 95% CI: 1.19–1.32; P < 0.001); and “difficult getting up from bed” (HR = 1.08, 95% CI: 1.05–1.10; P < 0.001). The corresponding population attributable risk percentage (PAR%) indicated that about 7% of healthspan termination in this cohort would have been eliminated if all participants had healthy sleep behaviors.
Conclusion
Participants who reported “usually experience sleeplessness/insomnia,” “usually nap,” “excessive daytime sleepiness,” and “difficult getting up from bed” had increased risk of shortened healthspan. Therefore, adherence to healthy sleep behavior is significant for the extension of healthspan.

Similar content being viewed by others
References
Li Y, Schoufour J, Wang DD, Dhana K, Pan A, Liu X, Song M, Liu G, Shin HJ, Sun Q, Al-Shaar L, Wang M, Rimm EB, Hertzmark E, Stampfer MJ, Willett WC, Franco OH, Hu FB (2020) Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ 368:l6669. https://doi.org/10.1136/bmj.l6669
GBD (2015) Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386(9995):743–800. https://doi.org/10.1016/s0140-6736(15)60692-4
Jagger C, Gillies C, Moscone F, Cambois E, Van Oyen H, Nusselder W, Robine J-M (2008) Inequalities in healthy life years in the 25 countries of the European Union in 2005: a cross-national meta-regression analysis. The Lancet 372(9656):2124–2131. https://doi.org/10.1016/s0140-6736(08)61594-9
Collaborators GM (2017) Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390(10100):1084–1150. https://doi.org/10.1016/s0140-6736(17)31833-0
Collaborators. GDaH, (2016) Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388(10053):1603–1658. https://doi.org/10.1016/s0140-6736(16)31460-x
WHO (2020) World Health Statistics: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2020. World Health Organization
Shadyaba AH, LaCroixc AZ (2015) Review genetic factors associated with longevity: a review of recent findings. Aging Res Rev. https://doi.org/10.1016/j.arr.2014.10.005
Barfield R, Wang H, Liu Y, Brody JA, Swenson B, Li R, Bartz TM, Sotoodehnia N, Chen YI, Cade BE, Chen H, Patel SR, Zhu X, Gharib SA, Johnson WC, Rotter JI, Saxena R, Purcell S, Lin X, Redline S, Sofer T (2019) Epigenome-wide association analysis of daytime sleepiness in the Multi-Ethnic Study of Atherosclerosis reveals African-American-specific associations. Sleep 42(8):zsz101. https://doi.org/10.1093/sleep/zsz101
Irwin MR, Olmstead R, Carroll JE (2016) Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry 80(1):40–52. https://doi.org/10.1016/j.biopsych.2015.05.014
Tobaldini E, Costantino G, Solbiati M, Cogliati C, Kara T, Nobili L, Montano N (2017) Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases. Neurosci Biobehav Rev 74(Pt B):321–329. https://doi.org/10.1016/j.neubiorev.2016.07.004
Carskadon MA, Chappell KR, Barker DH, Hart AC, Dwyer K, Gredvig-Ardito C, Starr C, McGeary JE (2019) A pilot prospective study of sleep patterns and DNA methylation-characterized epigenetic aging in young adults. BMC Res Notes 12(1):583. https://doi.org/10.1186/s13104-019-4633-1
Lo JC, Sim SK, Chee MW (2014) Sleep reduces false memory in healthy older adults. Sleep 37(4):665–671. https://doi.org/10.5665/sleep.3564 (671a)
Wang D, Li W, Cui X, Meng Y, Zhou M, Xiao L, Ma J, Yi G, Chen W (2016) Sleep duration and risk of coronary heart disease: a systematic review and meta-analysis of prospective cohort studies. Int J Cardiol 219:231–239. https://doi.org/10.1016/j.ijcard.2016.06.027
Westerlund A, Bellocco R, Sundstrom J, Adami HO, Akerstedt T, Trolle Lagerros Y (2013) Sleep characteristics and cardiovascular events in a large Swedish cohort. Eur J Epidemiol 28(6):463–473. https://doi.org/10.1007/s10654-013-9802-2
Fan M, Sun D, Zhou T, Heianza Y, Lv J, Li L, Qi L (2020) Sleep patterns, genetic susceptibility, and incident cardiovascular disease: a prospective study of 385 292 UK biobank participants. Eur Heart J 41(11):1182–1189. https://doi.org/10.1093/eurheartj/ehz849
Blachier M, Dauvilliers Y, Jaussent I, Helmer C, Ritchie K, Jouven X, Tzourio C, Amouyel P, Besset A, Ducimetiere P, Empana JP (2012) Excessive daytime sleepiness and vascular events: the three city study. Ann Neurol 71(5):661–667. https://doi.org/10.1002/ana.22656
Boden-Albala B, Roberts ET, Bazil C, Moon Y, Elkind MS, Rundek T, Paik MC, Sacco RL (2012) Daytime sleepiness and risk of stroke and vascular disease: findings from the Northern Manhattan Study (NOMAS). Circ Cardiovasc Qual Outcomes 5(4):500–507. https://doi.org/10.1161/CIRCOUTCOMES.111.963801
Bertisch SM, Pollock BD, Mittleman MA, Buysse DJ, Bazzano LA, Gottlieb DJ, Redline S (2018) Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: Sleep Heart Health Study. Sleep 41(6):zsy047. https://doi.org/10.1093/sleep/zsy047
Laugsand LE, Vatten LJ, Platou C, Janszky I (2011) Insomnia and the risk of acute myocardial infarction: a population study. Circulation 124(19):2073–2081. https://doi.org/10.1161/CIRCULATIONAHA.111.025858
Hsu CY, Chen YT, Chen MH, Huang CC, Chiang CH, Huang PH, Chen JW, Chen TJ, Lin SJ, Leu HB, Chan WL (2015) The association between insomnia and increased future cardiovascular events: a nationwide population-based study. Psychosom Med 77(7):743–751. https://doi.org/10.1097/PSY.0000000000000199
Geiger-Brown J, Sagherian K, Zhu S, Wieroniey MA, Blair L, Warren J, Hinds PS, Szeles R (2016) Napping on the night shift: a two-hospital implementation project. Am J Nurs 116(5):26–33
Li H, Shao Y, Xing Z, Li Y, Wang S, Zhang M, Ying J, Shi Y, Sun J (2019) Napping on night-shifts among nursing staff: a mixed-methods systematic review. J Adv Nurs 75(2):291–312. https://doi.org/10.1111/jan.13859
Tumiran MA, Rahman NNA, Saat RM, Kabir N, Zulkifli MY, Adli DSH (2018) The concept of Qailulah (midday napping) from neuroscientific and Islamic perspectives. J Relig Health 57(4):1363–1375. https://doi.org/10.1007/s10943-015-0093-7
Cheungpasitporn W, Thongprayoon C, Srivali N, Vijayvargiya P, Andersen CA, Kittanamongkolchai W, Sathick IJ, Caples SM, Erickson SB (2016) The effects of napping on the risk of hypertension: a systematic review and meta-analysis. J Evid Based Med 9(4):205–212. https://doi.org/10.1111/jebm.12211
Institute of Medicine Committee on Sleep M, Research (2006) The national academies collection: reports funded by National Institutes of Health. In: Colten HR, Altevogt BM (eds) Sleep disorders and sleep deprivation: an unmet public health problem. National Academies Press (US). Copyright © 2006, National Academy of Sciences., Washington (DC)
Ackermann K, Plomp R, Lao O, Middleton B, Revell VL, Skene DJ, Kayser M (2013) Effect of sleep deprivation on rhythms of clock gene expression and melatonin in humans. Chronobiol Int 30(7):901–909. https://doi.org/10.3109/07420528.2013.784773
Faraut B, Andrillon T, Vecchierini MF, Leger D (2017) Napping: A public health issue. From epidemiological to laboratory studies. Sleep Med Rev 35:85–100. https://doi.org/10.1016/j.smrv.2016.09.002
Yin J, Jin X, Shan Z, Li S, Huang H, Li P, Peng X, Peng Z, Yu K, Bao W, Yang W, Chen X, Liu L (2017) Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc 6(9):e005947. https://doi.org/10.1161/JAHA.117.005947
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P, Elliott P, Green J, Landray M, Liu B, Matthews P, Ong G, Pell J, Silman A, Young A, Sprosen T, Peakman T, Collins R (2015) UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 12(3):e1001779. https://doi.org/10.1371/journal.pmed.1001779
Johansson A, Rask-Andersen M, Karlsson T, Ek WE (2019) Genome-wide association analysis of 350 000 Caucasians from the UK Biobank identifies novel loci for asthma, hay fever and eczema. Hum Mol Genet 28(23):4022–4041. https://doi.org/10.1093/hmg/ddz175
Zenin A, Tsepilov Y, Sharapov S, Getmantsev E, Menshikov LI, Fedichev PO, Aulchenko Y (2019) Identification of 12 genetic loci associated with human healthspan. Commun Biol 2:41. https://doi.org/10.1038/s42003-019-0290-0
Leng Y, Wainwright NWJ, Cappuccio FP, Surtees PG, Hayat S, Luben R, Brayne C, Khaw KT (2014) Daytime napping and the risk of all-cause and cause-specific mortality: a 13-year follow-up of a British population. Am J Epidemiol 179(9):1115–1124. https://doi.org/10.1093/aje/kwu036
Bonsall SYaA (2017) UK Townsend Deprivation Scores from 2011 census data.pdf
Weisberg JFS (2010) Cox proportional-hazards regression for survival data in R: an appendix to an R companion to applied regression, third edition
Javaheri S, Redline S (2017) Insomnia and risk of cardiovascular disease. Chest 152(2):435–444. https://doi.org/10.1016/j.chest.2017.01.026
Depner CM, Stothard ER, Wright KP Jr (2014) Metabolic consequences of sleep and circadian disorders. Curr Diab Rep 14(7):507. https://doi.org/10.1007/s11892-014-0507-z
Erren TC, Morfeld P, Foster RG, Reiter RJ, Groß JV, Westermann IK (2016) Sleep and cancer: synthesis of experimental data and meta-analyses of cancer incidence among some 1,500,000 study individuals in 13 countries. Chronobiol Int 33(4):325–350. https://doi.org/10.3109/07420528.2016.1149486
Ruggiero JS, Redeker NS (2014) Effects of napping on sleepiness and sleep-related performance deficits in night-shift workers: a systematic review. Biol Res Nurs 16(2):134–42. https://doi.org/10.1177/1099800413476571
Leng Y, Ahmadi-Abhari S, Wainwright NWJ, Cappuccio FP, Surtees PG, Luben R, Brayne C, Khaw K-T (2014) Daytime napping, sleep duration and serum C reactive protein: a population-based cohort study. BMJ Open 4(11):e006071. https://doi.org/10.1136/bmjopen-2014-006071
Skeldon AC, Derks G, Dijk DJ (2016) Modelling changes in sleep timing and duration across the lifespan: changes in circadian rhythmicity or sleep homeostasis? Sleep Med Rev 28:96–107. https://doi.org/10.1016/j.smrv.2015.05.011
Magnavita N, Garbarino S (2017) Sleep, health and wellness at work: a scoping review. Int J Environ Res Public Health 14(11):1347. https://doi.org/10.3390/ijerph14111347
Gangwisch JE, Rexrode K, Forman JP, Mukamal K, Malaspina D, Feskanich D (2014) Daytime sleepiness and risk of coronary heart disease and stroke: results from the Nurses’ Health Study II. Sleep Med 15(7):782–788. https://doi.org/10.1016/j.sleep.2014.04.001
Ahlberg K, Jahkola A, Savolainen A, Könönen M, Partinen M, Hublin C, Sinisalo J, Lindholm H, Sarna S, Ahlberg J (2008) Associations of reported bruxism with insomnia and insufficient sleep symptoms among media personnel with or without irregular shift work. Head Face Med 4:4. https://doi.org/10.1186/1746-160x-4-4
Chakravorty S, Chaudhary NS, Brower KJ (2016) Alcohol dependence and its relationship with insomnia and other sleep disorders. Alcohol Clin Exp Res 40(11):2271–2282. https://doi.org/10.1111/acer.13217
Owens JA, Dearth-Wesley T, Lewin D, Gioia G, Whitaker RC (2016) Self-regulation and sleep duration, sleepiness, and chronotype in adolescents. Pediatrics 138(6):e20161406. https://doi.org/10.1542/peds.2016-1406
Patterson F, Malone SK, Grandner MA, Lozano A, Perkett M, Hanlon A (2018) Interactive effects of sleep duration and morning/evening preference on cardiovascular risk factors. Eur J Public Health 28(1):155–161. https://doi.org/10.1093/eurpub/ckx029
Redeker NS, Caruso CC, Hashmi SD, Mullington JM, Grandner M, Morgenthaler TI (2019) Workplace interventions to promote sleep health and an alert, healthy workforce. J Clin Sleep Med 15(4):649–657. https://doi.org/10.5664/jcsm.7734
Palermo TA, Rotenberg L, Zeitoune RC, Silva-Costa A, Souto EP, Griep RH (2015) Napping during the night shift and recovery after work among hospital nurses. Rev Lat Am Enfermagem 23(1):114–121. https://doi.org/10.1590/0104-1169.0147.2532
Acknowledgments
We thank the study participants and research staff for their contributions and commitment to this study.
Funding
This study was conducted using the UK-Biobank resource (Application Number 64689). This work was supported by the National Natural Science of China (81941020).
Author information
Authors and Affiliations
Contributions
MLS and XZ conducted the statistical analysis and wrote the first draft. TH, AS, and TBB helped apply for permission to use data and offered technical support during the study. GJ, ELH, and MN critically revised the manuscript for important intellectual content. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Research involving human participants and/or animals
The UKB adhered to ethical guidelines as stated in the Helsinki declaration, and the ethical approval for the study was issued by the North West Multicenter Research Ethical Committee.
Informed consent
We utilized the UKB dataset, and participants gave written informed consent during the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sambou, M.L., Zhao, X., Hong, T. et al. Investigation of the relationships between sleep behaviors and risk of healthspan termination: a prospective cohort study based on 323,373 UK-Biobank participants. Sleep Breath 26, 205–213 (2022). https://doi.org/10.1007/s11325-021-02394-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02394-0