Abstract
Purpose
This study was undertaken to clinically validate the accuracy of a semiautomated software tool for analysing the enhancement curve in focal malignant bone lesions.
Materials and methods
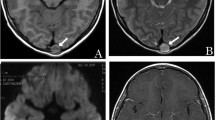
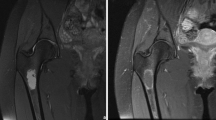
Twenty-three patients affected by cancer with malignant focal bone lesions underwent dynamic gadolinium-enhanced magnetic resonance (MR) imaging using the following protocol: T1-weighted turbo spin-echo sequences (time to repeat [TR] 600 ms, time to echo [TE] 8.6 ms, field of view [FOV] 40×40 cm) before and after intravenous injection of gadolinium-containing contrast agent. Image postprocessing was performed using the software DyCoH. Each region of interest (5×5 pixels), drawn to include the area of the lesion with the highest values of the area under the curve map, was analysed to obtain time-intensity curves and relative perfusion parameters: time to peak (TTP), peak intensity (PI), slope (60-s slope), intensity at 60 s after contrast agent injection (60-s I) and final intensity (FI).
Results
Data were obtained by analysing 86 malignant lesions and 86 apparently normal bone regions. PI, 60-s slope, 60-s I and FI were significantly different between neoplastic and apparently normal (p<0.001) samples. Sensitivity, specificity and accuracy were, respectively, 94%, 93% and 94% at a PI threshold of 100 (signal-to-noise ratio), with positive and negative predictive values of 93% and 94%. At a threshold value of 0.85 for 60-s slope, sensitivity and specificity values were both 91%.
Conclusions
The semiautomated technique we report appears to be accurate for identifying neoplastic tissue and for mapping perfusion parameters, with the added value of a consistent measurement of perfusion parameters on colour-coded maps.
Riassunto
Obiettivo
Scopo del presente lavoro è stato valutare l’accuratezza di un software di analisi semiautomatica nell’analisi delle curve di potenziamento post-contrastografico delle lesioni ossee focali maligne.
Materiali e metodi
Ventitre pazienti oncologici con lesioni ossee focali maligne sono stati sottoposti ad esame di risonanza magnetica dinamica utilizzando sequenze turbo spin echo T1-pesate (tempo di ripetizione [TR] 600 ms, tempo di eco [TE] 8,6 ms, campo di vista [FOV] 40×40 cm) prima e dopo somministrazione endovenosa di mezzo di contrasto paramagnetico. L’analisi delle immagini è stata poi effettuata utilizzando il software DyCoH. Ciascuna regione di interesse (ROI, 5×5 pixel), posizionata nella zona della lesione che presentava i più alti valori di area sotto la curva (AUC) sulla mappa, è stata analizzata per ottenere le curve intensità/tempo ed i relativi parametri perfusionali: tempo di picco (TTP), intensità di picco (PI), pendenza (60”Slope) ed intensità (60”I) al primo minuto dopo la somministrazione di mezzo di contrasto, intensità finale (FI).
Risultati
I risultati sono stati ottenuti dall’analisi di 86 lesioni maligne ed 86 regioni di tessuto osseo apparentemente normale. I parametri PI, 60”Slope, 60”I e FI hanno mostrato valori con differenza statisticamente significativa tra lesioni neoplastiche e tessuto osseo apparentemente normale (p<0,001). La sensibilità, la specificità e l’accuratezza calcolate si sono mostrate rispettivamente del 94%, 93% e 94% ad un valore soglia di PI di 100 (signal to noise ratio, SNR), con valori predittivi positivi e negativi rispettivamente del 93% e 94%. Ad un valore soglia di 0,85 per il parametro 60”Slope, la sensibilità, la specificità, l’accuratezza ed i valori predittivi positivi e negativi erano del 91%.
Conclusioni
La tecnica di analisi semiautomatica utilizzata appare accurata nell’identificazione di tessuto neoplastico e nell’elaborazione di mappe parametriche perfusionali, con il valore aggiunto di una valida misura dei parametri perfusionali sulle mappe colorimetriche stesse.
Similar content being viewed by others
References/Bibliografia
Padhani AR (2002) Dynamic contrast-enhanced MRI in clinical oncology: current status and future directions. J Magn Reson Imaging 16:407–422
Choyke PL, Dwyer AJ, Knopp MV (2003) Functional tumor imaging with dynamic contrast-enhanced magnetic resonance imaging J Magn Reson Imaging 17:509–520
Padhani AR (1999) Dynamic contrast enhanced MRI studies in human tumors. Br J Radiol 72:427–431
Carmeliet P, Jain RK (2000) Angiogenesis in cancer and other diseases. Nature 407:249–257
Jackson A, Buckley DL, Parker GJM (2005) Dynamic contrast-enhanced magnetic resonance imaging in oncology. Springer-Verlag, Berlin
Verstraete KL, Van der Woude HJ, Hogendoorn PC et al (1996) Dynamic contrast-enhanced MR imaging of musculoskeletal tumors: basic principles and clinical applications. J Magn Reson Imaging 6:311–321
Daniel BL, Yen YF, Glover GH et al (1998) Breast disease: dynamic spiral MR imaging. Radiology 209:499–509
Russo V, Setola R, Del Vescovo R et al (2007) DyCoH: an innovative tool to dynamic contrast enhancement analysis. Conf Proc IEEE Eng Med Biol Soc 1:63–66
Quattrocchi CC, Santini D, Dell’aia P et al (2007) A prospective analysis of CT density measurements of bone metastases after treatment with zoledronic acid. Skeletal Radiol 36:1121–1127
Padhani AR, Leach M (2005) Antivascular cancer treatments: functional assessments by dynamic contrast-enhanced magnetic resonance imaging. Abdom Imaging 30:324–341
Zahra MA, Hollingsworth KG, Sala E et al (2007) Dynamic contrast-enhanced MRI as a predictor of tumor response to radiotherapy. Lancet Oncol 8:63–74
Jeong KK, Seong SH, Young JC et al (2005) Wash-in rate on the basis of dynamic contrast-enhanced MRI: usefulness for prostate cancer detection and localization. J Magn Reson Imaging 22:639–646
Schaefer JF, Vollmar J, Schick F et al (2004) Solitary pulmonary nodules: dynamic contrast-enhanced MR imaging-perfusion differences in malignant and benign lesions. Radiology 232:544–553
Jackson A (2004) Analysis of dynamic contrast enhanced MRI. Br J Radiol 77:S154–S166
Jackson A, O’Connor JP, Parker GJ et al (2007) Imaging tumor vascular heterogeneity and angiogenesis using dynamic contrast-enhanced magnetic resonance imaging. Clin Cancer Res 13:3449–3459
Evelhoch JL (1999) Key factors in the acquisition of contrast kinetic data for oncology. J Magn Reson Imaging;10:254–259
Lavini C, de Jonge MC, van de Sande MG et al (2007) Pixel-by-pixel analysis of DCE-MRI curve patterns and an illustration of its applications to the imaging of the musculoskeletal system. Magn Reson Imaging;25:604–612
Verstraete KL, De Deene Y, Roels H et al (1994) Benign and malignant musculoskeletal lesions: dynamic contrast-enhanced MR imaging - parametric “first-pass” images depict tissue vascularization and perfusion. Radiology;192:835–843
Rijpkema M, Kaanders JH, Joosten FB et al (2001) A method for quantitative mapping of dynamic MRI contrast agent uptake in human tumors. J Magn Reson Imaging 14:457–463
Gribbestad IS, Nilsen G, Fjøsne HE et al (1994) Comparative signal intensity measurements in dynamic gadolinium-enhanced MR mammography. J Magn Reson Imaging 4:477–480
Aronen HJ, Gazit IE, Louis DN et al (1994) Cerebral blood volume maps of gliomas: comparison with tumor grade and histologic findings. Radiology 191:41–51
Barile A, Regis G, Masi R et al (2007) Musculoskeletal tumours: preliminary experience with perfusion MRI. Radiol Med 112:550–561
Griffith JF, Yeung DK, Antonio GE et al (2006) Vertebral marrow fat content and diffusion and perfusion indexes in women with varying bone density: MR evaluation. Radiology 241:831–838
Griffith JF, Yeung DK, Antonio GE et al (2005) Vertebral bone mineral density, marrow perfusion, and fat content in healthy men and men with osteoporosis: dynamic contrast-enhanced MR imaging and MR spectroscopy. Radiology 236:945–951
Lauenstein TC, Goehde SC, Herborn CU et al (2004) Whole-body MR imaging: evaluation of patients for metastases. Radiology 233:139–148
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
D’Agostino, F., Dell’Aia, P., Quattrocchi, C. et al. Differentiation of normal and neoplastic bone tissue in dynamic gadolinium-enhanced magnetic resonance imaging: validation of a semiautomated technique. Radiol med 115, 804–814 (2010). https://doi.org/10.1007/s11547-010-0572-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-010-0572-6