Abstract
Background
Eliminating health disparities among different segments of the US population is an overarching goal of the US Healthy People 2020 objectives.
Objective
Examine changes in educational, rural-urban, and racial disparities in premature mortality during the past 10 years.
Design and Participants
Descriptive analysis of US mortality data from 2007 to 2017.
Main Measures
Relative and absolute rural-urban, educational attainment, and Black-White disparities in premature mortality for all-cause and top 10 causes of death among persons ages 25–74 years, estimated as rate ratios and rate differences between ≤12 and ≥16 years of education, rural versus urban, and non-Hispanic Black (Black) versus non-Hispanic White (White), respectively, in 2007 and 2017.
Key Results
During 2007–2017, mortality rates in persons aged 25–74 years in the USA increased for several leading causes of death, especially in persons with <16 years of education, rural residents, and White people. As a result, disparity in mortality between 2007 and 2017 widened on both relative and absolute scales for all-cause and for 6 of the top 10 causes of death by education and for all-cause and for 9 of the top 10 causes by rural/urban residence. In contrast, Black-White disparities narrowed for all-cause and for all 7 causes that Black people had a higher rate than White people. For all-cause mortality for example, absolute disparities in the number of deaths per 100,000 person-years between 2007 and 2017 increased from 454.0 (95%CI, 446.0–462.1) to 542.7 (535.6–549.7) for educational attainment and from 85.8 (82.8–88.8) to 140.5 (137.6–143.4) for rural versus urban; in contrast, absolute Black-White disparity decreased from 315.3 (311.0–319.7) to 221.7 (218.1–225.3).
Conclusions
Educational and rural-urban disparities in premature mortality widened, whereas Black-White disparities narrowed in the USA between 2007 and 2017, though overall rates remained considerably higher in Black people.
Similar content being viewed by others
INTRODUCTION
In December 2010, the U.S. Department of Health and Human Services (HHS) launched the Healthy People 2020 initiative as it has done every 10 years during the past few decades.1 One of the Healthy People 2020 initiative’s four overarching goals was to achieve health equity and to eliminate health disparities among different segments of the US population defined by dimensions such as socioeconomic status (SES), rural/urban residence, and race/ethnicity.2,3
Over the past 10 years, many major national and local efforts have addressed this goal, including the Affordable Care Act (ACA) to expand healthcare coverage to broad group of low-income adults, HHS Action Plan to Reduce Racial and Ethnic Health Disparities,4 the National Stakeholder Strategy for Achieving Health Equity,5 and the National Partnership for Action to End Health Disparities.6 For example, over 20 million adults have gained insurance coverage through the ACA.7
Previous studies examined progress in reducing disparities over the past decade by race/ethnicity,8 SES,9 or rural/urban.10 Few studies, however, examined progress by all these three dimensions concurrently. Herein, we assessed progress in eliminating educational, rural-urban, and Black-White disparities in premature mortality in men and women ages 25–74 years from all-cause (all causes combined) and the 10 leading causes of death during 2007–2017. Findings from this study can inform future interventions to reduce health disparities.
METHODS
Data Source
Deaths occurring in ages 25–74 years by sex, race/ethnicity, and educational attainment from 2007 to 2017 in the USA (the 50 states and the District of Colombia) which served as the numerator for calculating death rates, were obtained from the National Centers for Health Statistics 11. Underlying causes of death were coded based on the selection and coding rules of the tenth revision of International Classification of Disease (ICD-10) codes 12 (see eTable1 for the ICD codes for all-cause and 10 leading causes of death). In 2017, these 10 leading causes accounted for about 78% of total deaths among persons ages 25–74 years.13
Population data, which served as the denominator of rates, for the corresponding age group, sex, race/ethnicity, educational attainment, and calendar year were obtained from the public-use microdata sample files of the American Community Survey (ACS).14 However, information on educational attainment from ACS was measured by the highest level of education completed, while from NCHS it was measured by the number of years of schooling. To make the two measures comparable, we broadly categorized educational attainment from NCHS to ≤12 years education comparable to ≤ high school, 13–15 years of education comparable to some college, and ≥16 years of education comparable to Bachelor’s degree or above.
We obtained age-standardized death rates for all-cause and the 10 leading causes of death from 2007 to 2017 for ages 25–74 years by sex and urbanicity (residence in metropolitan counties [urban] or in non-metropolitan counties[rural]) from the SEER*Stat database.15 We restricted analyses to ages 25–74 years to emphasize disparities in premature mortality among adults and to account for some people not completing their highest education until age 25 years.16 For racial/ethnic disparities, we limited analysis to non-Hispanic Black (Black) versus non-Hispanic White (White) because Hispanic and Asian American, Native Hawaiian, or Pacific Islander have a lower mortality rate than White population17 and because accuracy of race/ethnicity information on death certificates is considerably lower for American Indian/Alaskan Natives.18
Statistical Analysis
Annual direct age-standardized death rates were calculated by sex, educational attainment (≤12, 13–15, and ≥16 years of education), rural/urban residence, and race/ethnicity (all races combined, White, and Black) based on the 2000 US standard population. Annual percent changes (APCs) and average APCs (AAPCs) in age-standardized death rates from 2007 to 2017 along with their 95% confidence intervals (CIs) were estimated by grid search of joinpoints by permutation test with a maximum of 1 joinpoint allowed, using Joinpoint Regression Program, Version 4.7.0. Trends were considered increasing or decreasing when the 95%CIs of corresponding APCs or AAPCs did not include 0; otherwise, they were considered stable. Relative and absolute educational, residential, and racial disparities in morality, comparing rates between persons with ≤12 and with ≥16 years of education, between rural and urban residents, and between Black and White were estimated as rate ratios (RRs) and rate differences (RDs), respectively, in 2007 and 2017. The resulting absolute and relative disparities between 2007 and 2017 were considered statistically significantly different if their 95%CIs did not overlap. In additional analysis, we also examined if trends were different by sex and different rural/urban designations.
KEY RESULTS
From 2007 to 2017, a total of 11,851,982 all-cause deaths (59.6% in men and 40.4% in women) occurred in ages 25–74 years in the USA (eTable2). By race, White and Black persons accounted for 73.8% and 15.8% of the deaths, respectively. By educational attainment, persons with ≤12 years of education accounted for 63.8% of the deaths, followed by persons with 13–15 years of education (20.9%) and persons with ≥16 years of education (15.2%). About 80.5% of the deaths occurred in urban residents and 19.5% of the deaths in rural residents. Cancer was the leading cause of premature death (30.2%) followed by heart disease (20.4%) and accidents (7.7%).
Figure 1 and eTable3 show mortality trends by educational attainment for all-cause and the 10 leading causes of death for both sexes combined. Overall, the all-cause mortality rate decreased by 1.50% (95%CI, 0.98–2.02%) per year during 2007–2012. But it increased by 0.73% (95%CI, 0.22–1.24%) per year from 2012 to 2017. This increase, however, was confined to those with ≤15 years of education, among whom rates increased by close to 2% per year, and was in a stark contrast with a declining trend (0.93% [95%CI, 0.5–1.36%] per year) among those with ≥16 years of education.
Trends in death rates by cause of death and educational attainment, ages 25–74 years, 2007–2017. Note: Rates were age-standardized to the 2000 US standard population and expressed per 100,000 person-years. Dots in graphs are observed rates and lines are fitted rates based on joinpoint analysis. CLRD denotes chronic lower respiratory diseases. Chronic liver disease denotes chronic liver disease and cirrhosis. Nephritis denotes nephritis, nephrotic syndrome, and nephrosis.
Similarly, the mortality trends for the 10 leading causes of death were most favorable for most educated persons (Fig. 1 and eTable3). For causes with an overall decreasing trend (cancer, heart disease, chronic lower respiratory diseases, and cerebrovascular diseases), decreases were either confined to or steeper in persons with ≥16 years of education. Among causes of death with an overall increasing trend (accidents, suicide, and chronic liver disease and cirrhosis), increases were confined to or steeper in persons with ≤15 years of education. For example, during 2007–2017, cancer death rate decreased by 2.36% (95%CI, 2.02–2.69%) per year among those with ≥16 years of education, compared to 1.35% (95%CI, 1.16–1.54%) per year among those with ≤12 years of education. Notably, the death rate for accidents increased from 2013 to 2017 for all levels of education, ranging from 3% per year for those with ≥16 years of education to 10.6% per year for those with ≤12 years of education. Generally similar patterns were observed in both men and women for all-cause and the 10 leading causes of death (eTable4 and eTable5).
Figure 2 and eTable6 show mortality trends for urban and rural residents for both sexes combined. During 2007–2017, all-cause mortality rate decreased (AAPC, 0.42% [95%CI, 0.20–0.64%]) among urban residents but increased (AAPC, 0.55% [95%CI, 0.24–0.86%]) among rural residents, although rates ticked up among urban residents 2012–2017. Cause-specific mortality trends were more favorable for urban areas than rural areas for 9 of the 10 leading causes of death. For example, heart disease mortality rate from 2011 to 2017 increased by 0.91% (95%CI, 0.48–1.34%) per year in rural areas but remained stable in urban areas, after declining by 1.52% and 2.96% per year, respectively, during 2007–2011. In additional analysis, we found that mortality trends were more favorable for large metropolitan areas than small metropolitan areas within urban area groups but were generally similar within rural area groups by population size and distance to the metropolitan areas (eTable7).
Trends in death rates by cause of death among urban and rural residents, ages 25–74 years, 2007–2017. Notes: Rates were age-standardized to the 2000 US standard population and expressed per 100,000 person-years. Dots in graphs are observed rates and lines are fitted rates based on joinpoint analysis. CLRD denotes chronic lower respiratory diseases. Chronic liver disease denotes chronic liver disease and cirrhosis. Nephritis denotes Nephritis, nephrotic syndrome, and nephrosis.
Figure 3 and eTable8 show both sexes combined mortality trends for White and Black populations. All-cause mortality in White people declined slightly from 2007 to 2012 but increased from 2012 to 2017, resulting in an overall stable trend (AAPC=0.04%; 95%CI, −0.24–0.32%) during 2007–2017. In contrast, the rate in Black people declined steeply then stabilized, resulting in an overall decrease of 1.11% (95%CI, 0.65–1.58%) per year from 2007 to 2017. In general, trends were more favorable in Black than in White for each of the 10 leading causes of death. For example, cancer death rates from 2007 to 2017 declined by 2.31% (95%CI, 2.17–2.45%) per year in Black people compared to by 1.78% (95%CI, 1.72–1.85%) in White people. Diabetes mellitus death rates from 2011 to 2017 increased by 1.69% (95%CI, 1.16–2.23%) per years in White but stabilized in Black, after declining in both White and Black people from 2007 to 2011. Generally similar patterns were observed in both men and women (eTable9 and eTable10).
Trends in death rates by cause of death among non-Hispanic White (White) and non-Hispanic Black (Black) aged 25–74 years, 2007–2017. Notes: Rates were age-standardized to the 2000 US standard population and expressed per 100,000 person-years. Dots in graphs are observed rates and lines are fitted rates based on joinpoint analysis. CLRD denotes chronic lower respiratory diseases. Chronic liver disease denotes chronic liver disease and cirrhosis. Nephritis denotes nephritis, nephrotic syndrome, and nephrosis.
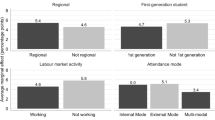
Figure 4 and supplemental eTable11 show relative and absolute educational, urban-rural, and Black-White disparities in mortality in 2007 versus 2017 for all-cause and 10 leading causes of death. In 2007, death rates were higher in persons with ≤12 years of education than in persons with ≥16 years of education for all-cause (RR=2.53, RD=454.0/100,000 persons) and for all ten leading causes of death, ranging from 1.9 times as high for cancer to 4.7 times as high for chronic lower respiratory disease. Between 2007 and 2017, such educational disparities widened on both relative and absolute scales for all-cause (RR=3.10, RD=542.7/100,000 persons) and for six (heart disease, accidents, chronic lower respiratory diseases, diabetes mellitus, suicide, and septicemia) of the 10 leading causes of death, with accidents showing the largest increase in absolute disparity. Generally similar patterns were observed among men and women (eTable11).
Educational, rural-urban, and black-white disparities in death rates by cause of death, ages 25–74 years, 2007 and 2017. CLRD denotes chronic lower respiratory diseases. Cerebrovasc Dis. denotes cerebrovascular diseases. Liver disease denotes chronic liver disease and cirrhosis. Nephritis denotes nephritis, nephrotic syndrome, and nephrosis.
Rural residents had higher death rates than urban residents for all-cause and for all leading causes of death (Fig. 4, eTable11). From 2007 to 2017, rural-urban disparities widened on both relative and absolute scales for all-cause mortality (from RR=1.17, RD=85.8/100,000 persons to RR=1.29, RD=140.5/100,000 persons) and for 9 of the 10 leading causes, with heart disease and cancer showing the largest increase in the absolute disparity. Generally similar patterns were observed among men and women (eTable11).
In contrast to increasing educational and rural-urban disparities, Black-White disparity in all-cause mortality narrowed from 2007 to 2017 (from RR=1.60, RD=315.3/100,000 persons to RR=1.42, RD=221.7/100,000 persons), largely driven by cancer and heart disease (eTable11). Generally similar patterns were observed among men and women (eTable11).
DISCUSSION
Based on US national mortality data, mortality rates in persons aged 25–74 years during 2007–2017 increased for all-cause and several leading causes of death, especially in persons with <16 years of education, rural residents, and White people. As a result, educational and rural-urban disparities in premature mortality widened between 2007 and 2017 on both relative and absolute scales for all causes combined and most leading causes of death, whereas Black-White disparities narrowed slightly. Notably, educational disparities dwarfed those of other demographic measures, with the disparity in the overall mortality more than twice as high in both absolute and relative scales.
Widened educational and rural-urban disparities reflect the differential mortality trends that favored most educated persons and urban residents than their counterparts for nearly all the 10 leading causes of death. For example, for accidents— the major driver of increasing educational disparity in all-cause mortality—the death rates increased 3 times faster during 2013–2017 among those with ≤12 years of education than those with ≥16 years of education. For heart disease—the major driver of increasing rural-urban disparity in all-cause mortality—the death rates decreased by 1.2% per year during 2007–2017 among urban residents while the rates remained stable among rural residents.
Underlying these differential trends are a broad array of individual, societal, and environmental shared risk factors (social determinants of health) across conditions that contribute to educational and rural-urban disparities in the USA.19,20 Persons with less educational attainment and those residing in rural areas are more likely to have lower SES, live in poverty, be uninsured, lack health literacy, and if employed, be unable to take time off from work for receipt of preventive services as well as care for acute and chronic conditions.20,21,22 They are also more likely to live in neighborhoods that lack grocery stores for fresh fruits and vegetables 23,24; parks or other safe places for recreational and leisure-time activities 25,26; and health care facilities or providers for high-quality emergent and preventive services.27,28 Impoverished neighborhoods are also more likely to be targeted for advertising by the tobacco, fast food, beverage, and alcohol industries.29,30,31
Lower education and rural residence are also associated with higher levels of risk behaviors.32,33,34 During the past decade, progress in reducing tobacco use has been slower among less educated persons and smoking prevalence has remained higher.35 Similarly, the prevalence of obesity, high blood pressure, diabetes, high blood cholesterol, and physical inactivity has remained much higher in persons of lower SES.36,37 Recent data showed that prevalence of chronic HCV infection, a major risk factor of chronic liver disease, liver cancer, and cirrhosis, was twice as high in those with <12 years of education as in those with ≥12 years of education.38,39 The opioid epidemic, a major driver for increasing deaths from accidents and for flatting or falling US life expectancy over the past decade,40 has disproportionately impacted persons with lower SES.41,42 Widespread implementation and dissemination of effective interventions to reduce risk behaviors, such as enhancing access to care and increasing excise tax on tobacco, are essential for reducing educational and rural-urban health disparities. However, it is noteworthy that even in egalitarian countries with universal healthcare coverage there is substantial disparity in mortality by educational attainment43 although considerably lower than that found in the USA.
In contrast to the widening disparities by educational attainment and urban-rural residence, Black-White disparities in mortality narrowed, because of more favorable trends for many of leading causes of death in Black people. For example, for heart disease, one of the two major drivers of decreasing Black-White disparity in all-cause mortality, death rates decreased by 1.6% per year during 2007–2017 among Black people compared to 0.8% per year among White people during same time period. This may, in part, reflect the historic improvements in Black-White disparities in major risk factors, especially cigarette smoking,44 and improved quality and equity of care in US hospitals.45 The narrowing of the disparity may also in part reflect the increase in proportion of persons in the most educated group in Black than White people during the study period (eTable12). Nevertheless, Black people continued to have a much higher mortality rate than White people in 2017, in part because of greater Black representation in lower SES groups and lower educational attainment,46 reflections of life course exposures to structural racism.47 As the most basic component of SES, education not only determines a person’s future earning potentials, occupational opportunities, and social status but also provides health-information-seeking skills.48 In an increasingly diverse US population, however, future disparities evaluation research must continue to assess dimensions of race and ethnicity, SES (e.g., educational attainment), geography, sexual orientation, levels of disability, and more in order to ensure equitable gains in public health.
Recently, many national efforts have begun to address social determinants as the root causes of health disparities.4,5,6 Growing attention to alternative payment models focusing on paying for value, not volume, could also strengthen collaborations between the healthcare sector and communities in addressing disparities. The Affordable Care Act increased insurance coverage options and provided federal incentives for states to expand Medicaid eligibility to low-income adults, which has been associated with improved health insurance coverage and receipt of preventive, screening and treatment services.49,50,51 However, as of July 2021, 12 states have not adopted Medicaid expansion; many non-expansion states are in southern and midwestern states which are disproportionately represented by Black and rural populations and high poverty and uninsured rates.
Our study has several limitations. First, it is restricted to people aged 25–74 years and thus lacks information on disparities in children and adolescents and older seniors. Second, educational attainment recorded on the death certificates tends to be higher than self-reported information,52 which could result in underestimated socioeconomic disparities. We used broad educational categories to minimize this bias, however. Third, SES is a multidimensional construct that includes income, wealth, occupation, and education, among other individual and community-level factors53 that are not reported consistently on death certificates, and thus our findings of educational disparity in mortality may not reflect the whole spectrum of socioeconomic disparities arising from exposures over a life course. Fourth, national-level disparity in mortality patterns may mask substantial variations by state, county, and neighborhood. Fifth, we did not consider the intersectionality of the disparities by educational attainment, race/ethnicity, and urban/rural. This will be an important area for additional research. Sixth, we examined the change in racial/ethnic mortality disparity only between Black and White people. Future studies should examine the disparity for the other racial/ethnic populations.
CONCLUSIONS
All people, regardless of their race, ethnic origin, residence, or socioeconomic circumstance, deserve an equal opportunity to fulfill their full potential for health. Based on national mortality data, however, disparity in premature mortality from all causes and many major causes of death from 2007 to 2017 widened by educational attainment and rural residence but narrowed by race/ethnicity. Disparities not only affect socioeconomically disadvantaged populations, but also limit continued national improvements in health care and overall population health. As the US population becomes more diverse, it is increasingly important to address and mitigate health disparities across many dimensions to ensure equitable improvements in public health.
References
U.S. Department of Health and Human Services. HHS announces the nation’s new health promotion and disease prevention agenda. https://www.healthypeople.gov/sites/default/files/DefaultPressRelease_1.pdf. Accessed March 20, 2020.
U.S. Department of Health and Human Services. Healthy People 2020 Framework. https://www.healthypeople.gov/sites/default/files/HP2020Framework.pdf. Accessed March 24, 2020.
Koh HK, Blakey CR, Roper AY. Healthy People 2020: a report card on the health of the nation. JAMA. 2014;311(24):2475-2476.
Koh HK, Graham G, Glied SA. Reducing racial and ethnic disparities: the action plan from the department of health and human services. Health Aff (Millwood) 2011;30(10):1822-1829.
U.S. Department of Health and Human Services. National Stakeholder Strategy for Achieving Health Equity. https://minorityhealth.hhs.gov/npa/files/Plans/NSS/CompleteNSS.pdf. Accessed March 24, 2020.
U.S. Department of Health and Human Services. National Partnership for Action to End Health Disparities. https://minorityhealth.hhs.gov/npa/. Accessed March 24, 2020.
Obama B. United States Health Care Reform: Progress to Date and Next Steps. JAMA. 2016;316(5):525-532.
Benjamins MR, Silva A, Saiyed NS, De Maio FG. Comparison of all-cause mortality rates and inequities between Black and White populations across the 30 most populous US cities. JAMA Netw Open 2021;4(1):e2032086.
Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980-2015. Lancet. 2017;389(10077):1475-1490.
Elo IT, Hendi AS, Ho JY, Vierboom YC, Preston SH. Trends in non-Hispanic White mortality in the United States by metropolitan-nonmetropolitan status and region, 1990-2016. Popul Dev Rev 2019;45(3):549-583.
National Center for Health Statistics. Vital Statistics Online Data Portal. https://www.cdc.gov/nchs/data_access/vitalstatsonline.htm. Accessed November, 15, 2020.
World Health Organization. International Statistical Classification of Disease and Related Health Problems: 10th Revision. In. Geneva, Switzerland: World Health Organization; 1992.
Centers for Disease Control and Prevention. National Center for Health Statistics: National Vital Statistics System. https://www.cdc.gov/nchs/nvss/mortality_methods.htm. Accessed December, 10, 2017.
The United States Census Bureau. PUMS data, American Cummnity Survey. Available at:https://www.census.gov/programs-surveys/acs/data/pums.html. Accessed December, 20, 2019.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Mortality - All COD, Aggregated With County, Total U.S. (1990-2017) <Katrina/Rita Population Adjustment>, National Cancer Institute, DCCPS, Surveillance Research Program, released December 2019. Underlying mortality data provided by NCHS (www.cdc.gov/nchs).
Albano JD, Ward E, Jemal A, et al. Cancer mortality in the United States by education level and race. J Natl Cancer Inst 2007;99(18):1384-1394.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin 2021;71(1):7-33.
Arias E, Heron M, Hakes J. The validity of race and Hispanic-origin reporting on death certificates in the United States: an update. Vital Health Stat 2. 2016;(172):1-21.
Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health 2008;29:235-252.
Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep 2014;129 Suppl 2:19-31.
Barnett JC, Vornovitsky MS. Health insurance coverage in the United States: 2015. In. Washington, DC: U.S. Government Printing Office; 2016.
Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health 2011;32(1):381-398.
Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med 2009;36(1):74-81.
Walker RE, Keane CR, Burke JG. Disparities and access to healthy food in the United States: a review of food deserts literature. Health Place 2010;16(5):876-884.
Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev 2009;31:7-20.
Sallis JF, Floyd MF, Rodriguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125(5):729-737.
Bhatt J, Bathija P. Ensuring access to quality health care in vulnerable communities. Acad Med 2018;93(9):1271-1275.
Cyr ME, Etchin AG, Guthrie BJ, Benneyan JC. Access to specialty healthcare in urban versus rural US populations: a systematic literature review. BMC Health Serv Res 2019;19(1):974.
Hillier A, Chilton M, Zhao QW, Szymkowiak D, Coffman R, Mallya G. Concentration of tobacco advertisements at SNAP and WIC stores, Philadelphia, Pennsylvania, 2012. Prev Chronic Dis 2015;12:E15.
Lucan SC, Maroko AR, Sanon OC, Schechter CB. Unhealthful food-and-beverage advertising in subway stations: targeted marketing, vulnerable groups, dietary intake, and poor health. J Urban Health 2017;94(2):220-232.
Isgor Z, Powell L, Rimkus L, Chaloupka F. Associations between retail food store exterior advertisements and community demographic and socioeconomic composition. Health Place 2016;39:43-50.
Centers for Disease Control and Prevention. CDC Health Disparities and Inequalities Report - United States, 2013. MMWR Suppl. 2013;62(Suppl 3):1-184.
Doogan NJ, Roberts ME, Wewers ME, et al. A growing geographic disparity: Rural and urban cigarette smoking trends in the United States. Prev Med 2017;104:79-85.
Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005-2008). J Rural Health 2012;28(4):392-397.
National Center for Health Statistics. Health, United States, 2018. Hyattsville, MD. 2019.
Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284-2291.
Valero-Elizondo J, Hong JC, Spatz ES, et al. Persistent socioeconomic disparities in cardiovascular risk factors and health in the United States: Medical Expenditure Panel Survey 2002-2013. Atherosclerosis. 2018;269:301-305.
Armstrong GL, Wasley A, Simard EP, McQuillan GM, Kuhnert WL, Alter MJ. The prevalence of hepatitis C virus infection in the United States, 1999 through 2002. Ann Intern Med 2006;144(10):705-714.
Denniston MM, Jiles RB, Drobeniuc J, et al. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med 2014;160(5):293-300.
Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959-2017. JAMA. 2019;322(20):1996-2016.
Jalal H, Buchanich JM, Roberts MS, Balmert LC, Zhang K, Burke DS. Changing dynamics of the drug overdose epidemic in the United States from 1979 through 2016. Science. 2018;361(6408).
Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proc Natl Acad Sci U S A 2015;112(49):15078-15083.
Raghupathi V, Raghupathi W. The influence of education on health: an empirical assessment of OECD countries for the period 1995-2015. Arch Public Health 2020;78:20.
U.S. Department of Health and Human Services. Smoking Cessation: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2020.
Trivedi AN, Nsa W, Hausmann LR, et al. Quality and equity of care in U.S. hospitals. N Engl J Med 2014;371(24):2298-2308.
Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychology. 2016;35(4):407-411.
Bailey ZD, Krieger N, Agenor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453-1463.
Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 2002;21(2):60-76.
Koh HK, Rajkumar R, McDonough JE. Reframing prevention in the era of health reform. JAMA. 2016;316(10):1039-1040.
Koh HK, Sebelius KG. Promoting prevention through the Affordable Care Act. N Engl J Med 2010;363(14):1296-1299.
Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after medicaid expansion or expanded private insurance. JAMA Intern Med 2016;176(10):1501-1509.
Rostron BL, Boies JL, Arias E. Education reporting and classification on death certificates in the United States. Washington, DC: U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention; 2010.
Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51 Suppl:S28-40.
Acknowledgements
We acknowledge the Intramural Research Department of the American Cancer Society for supporting this study.
Funding
Supported by the Intramural Research Department of the American Cancer Society (Ma, Yabroff, Siegel, Cance, and Jemal).
Author information
Authors and Affiliations
Contributions
Concept and design: Ma, Jemal
Acquisition, analysis, or interpretation of data: all authors
Drafting of the manuscript: Ma, Jemal
Critical revision of the manuscript for important intellectual content: all authors
Statistical analysis: Ma
Ma had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Role of the Funder/Sponsor
The funders of the study had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ma, J., Yabroff, K.R., Siegel, R.L. et al. Progress in Reducing Disparities in Premature Mortality in the USA: a Descriptive Study. J GEN INTERN MED 37, 2923–2930 (2022). https://doi.org/10.1007/s11606-021-07268-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07268-5