Abstract
Summary
This research aimed to determine the health care cost and utilisation of older Australian women with osteoporosis. A wide range of healthcare services were used and approximately AU$593.9 was spent over a 12-month period for these services. This highlights the significant cost burden of osteoporosis on the healthcare system.
Purpose
Osteoporosis is a common skeletal condition among women that has a considerable impact on quality of life. The purpose of this study is to determine the prevalence of healthcare use and to estimate associated out-of-pocket expenditure for the management of osteoporosis in older Australian women.
Methods
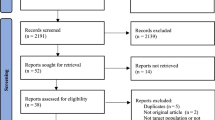
Data was obtained from 393 Australian women from the 45 and Up Study who had osteoporosis. The women were asked about healthcare use for their osteoporosis, including conventional medicine, complementary medicine, and self-care practices or self-care products, and associated out-of-pocket expenditure for that use over 12 months.
Results
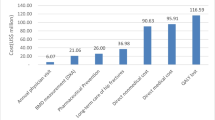
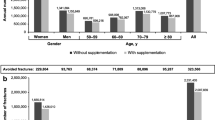
The average age of participants was 72.0 years. Over a 12-month period, the majority of participants (72%) consulted a doctor for their osteoporosis, 24% consulted an allied health practitioner, and 20% consulted a complementary medicine practitioner. Participants had a mean of 6.8 consultations with healthcare practitioners in the previous 12 months for the osteoporosis. In addition, 46% participants used three or more types of complementary medicine products/practices in the previous 12 months. Overall, the participants incurred a (arithmetic) mean ofAU$594 (median = $350; inter-quartile range = $450) in out-of-pocket expenditure for healthcare use over the 12-month period.
Conclusions
Women with osteoporosis use a wide range of healthcare services that are associated with significant annual out-of-pocket expenditure. Preventive strategies can help decrease the cost burden of osteoporosis on the healthcare system.
Similar content being viewed by others
Data availability
The data set and sub-study questionnaire could potentially be made available to other researchers if they obtain the necessary approvals. Further information on this process can be obtained from the 45 and Up Study (45andUp.research@ saxinstitute.org.au).
References
Tu KN, Lie JD, Wan CKV et al (2018) Osteoporosis: a review of treatment options. Pharmacy and Therapeutics 43(2):92
Viswanathan HN, Curtis JR, Yu J et al (2012) Direct healthcare costs of osteoporosis-related fractures in managed care patients receiving pharmacological osteoporosis therapy. Appl Health Econ Health Policy 10(3):163–173
Fujiwara S, Zhao X, Teoh C, Jaffe DH, Taguchi Y (2019) Disease burden of fractures among patients with osteoporosis in Japan: health-related quality of life, work productivity and activity impairment, healthcare resource utilization, and economic costs. J Bone Miner Metab 37(2):307–318
Ha Y-C, Kim H-Y, Jang S, Lee Y-K, Kim T-Y (2017) Economic burden of osteoporosis in South Korea: claim data of the national health insurance service from 2008 to 2011. Calcif Tissue Int 101(6):623–630
Henry MJ, Pasco JA, Nicholson GC, Kotowicz MA (2011) Prevalence of osteoporosis in Australian men and women: Geelong Osteoporosis Study. Med J Aust 195(6):321–322
Johnell O, Kanis J (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733
Kanis JA (2019) Diagnosis and clinical aspects of osteoporosis. Springer, Pocket reference to osteoporosis, pp 11–20
Lewiecki EM, Ortendahl JD, Vanderpuye‐Orgle J, et al. (2019) Healthcare policy changes in osteoporosis can improve outcomes and reduce costs in the United States. JBMR plus. 3(9):e10192.
Wu J, Qu Y, Wang K, Chen Y (2019) Healthcare resource utilization and direct medical costs for patients with osteoporotic fractures in China. Value in health regional issues 18:106–111
Jaleel A, Saag KG, Danila MI (2018) Improving drug adherence in osteoporosis: an update on more recent studies. Therapeutic advances in musculoskeletal disease 10(7):141–149
He J-B, Chen M-H, Lin D-K (2017) New insights into the tonifying kidney-yin herbs and formulas for the treatment of osteoporosis. Arch Osteoporos 12(1):14
Armstrong AR, Thiébaut SP, Brown LJ, Nepal B (2011) Australian adults use complementary and alternative medicine in the treatment of chronic illness: a national study. Aust N Z J Public Health 35(4):384–390
Adams J, Andrews G, Barnes J, Broom A, Magin P (2012) Traditional, complementary and integrative medicine: an international reader: Macmillan International Higher Education.
Banu J, Varela E, Fernandes G (2012) Alternative therapies for the prevention and treatment of osteoporosis. Nutr Rev 70(1):22–40
Habibi Ghahfarrokhi S, Reisi R (2019) Effects of medicinal herbs on osteoporosis: a systematic review based on clinical trials. Journal of Shahrekord University of Medical Sciences
Lips P, Van Schoor NM (2011) The effect of vitamin D on bone and osteoporosis. Best Pract Res Clin Endocrinol Metab 25(4):585–591
Taku K, Melby MK, Nishi N, Omori T, Kurzer MS (2011) Soy isoflavones for osteoporosis: an evidence-based approach. Maturitas 70(4):333–338
Pan H, Jin R, Li M, Liu Z, Xie Q, Wang P (2018) The effectiveness of acupuncture for osteoporosis: a systematic review and meta-analysis. Am J Chin Med 46(03):489–513
Zhang Y, Chai Y, Pan X, Shen H, Wei X, Xie Y (2019) Tai chi for treating osteopenia and primary osteoporosis: a meta-analysis and trial sequential analysis. Clin Interv Aging 14:91
Mughal N, Inderjeeth AJ, Inderjeeth CA (2019) Osteoporosis in patients with dementia is associated with high morbidity and mortality: ‘findings from a single orthogeriatric unit.’ Australian journal of general practice 48(1/2):53–58
Duckett S, Willcox S (2015) The Australian health care system: Oxford University Press
Carpenter A, Islam MM, Yen L, Mcrae I (2015) Affordability of out-of-pocket health care expenses among older Australians. Health Policy 119(7):907–914
Chong C, Diaz-Granados N, Hawker G, Jamal S, Josse R, Cheung A (2007) Complementary and alternative medicine use by osteoporosis clinic patients. Osteoporos Int 18(11):1547–1556
Mak JC, Faux S (2010) Complementary and alternative medicine use by osteoporotic patients in Australia (CAMEO-A): a prospective study. The Journal Of Alternative and Complementary Medicine 16(5):579–584
Collaborators US (2008) Cohort profile: the 45 and up study. Int J Epidemiol 37(5):941–947
Rural A (2004) Regional and remote health: a guide to remoteness classifications. Canberra: Australian Institute of Health and Welfare AIHW Cat. No. PHE. 53
NSW Government (2019) HealthStats NSW. http://www.healthstats.nsw.gov.au/indicator/dem_pop_age. Accessed 19 July 2021
Australian Bureau of Statistics (2016) Australian Demographic Statistics, Population by age and sex. Canberra: Australian Bureau of Statistics; June 2016
Statistics ABo (2018) 4364.0. 55.001‐National Health Survey First Results, Australia 2017–2018
Steel A, McIntyre E, Harnett J et al (2018) Complementary medicine use in the Australian population: results of a nationally-representative cross-sectional survey. Sci Rep 8(1):1–7
Lefevre A, Hopper I, McNeil JJ, Owen A (2021) Complementary medicine use by community-dwelling older Australians. Med J Aust 214(3):140–141
von Conrady DM, Bonney A (2017) Patterns of complementary and alternative medicine use and health literacy in general practice patients in urban and regional Australia. Aust Fam Physician 46(5):315–324
Ercan E, Ibci S (2018) Use of complementary and alternative medicine by osteoporosis and osteopenia patients. Int J Caring Sci 11(3):1546–1556
McLaughlin D, Lui C-W, Adams J (2012) Complementary and alternative medicine use among older Australian women-a qualitative analysis. BMC Complement Altern Med 12(1):1–8
Vestergaard P, Hermann P, Jensen J-E, Eiken P, Mosekilde L (2012) Effects of paracetamol, non-steroidal anti-inflammatory drugs, acetylsalicylic acid, and opioids on bone mineral density and risk of fracture: results of the Danish Osteoporosis Prevention Study (DOPS). Osteoporos Int 23(4):1255–1265
Gosch M, Jeske M, Kammerlander C, Roth T (2012) Osteoporosis and polypharmacy. Z Gerontol Geriatr 45(6):450–454
Kirby ER, Broom AF, Sibbritt DW, Refshauge KM, Adams J (2013) Health care utilisation and out-of-pocket expenditure associated with back pain: a nationally representative survey of Australian women. PloS one. 8(12):e83559
Navin Cristina TJ, Stewart Williams JA, Parkinson L, Sibbritt DW, Byles JE (2016) Identification of diabetes, heart disease, hypertension and stroke in mid-and older-aged women: comparing self-report and administrative hospital data records. Geriatr Gerontol Int 16(1):95–102
Acknowledgements
This research was completed using data collected through the 45 and Up Study (www.saxinstitute.org.au). The 45 and Up Study is managed by the Sax Institute in collaboration with major partner Cancer Council NSW; and partners: the Heart Foundation; NSW Ministry of Health; NSW Department of Communities and Justice; and the Australian Red Cross Blood Service. We thank the many thousands of people participating in the 45 and Up Study.
Funding
The Australian Research Council (DP140100238) funded this sub-study of women with osteoarthritis upon which this research paper is based.
Author information
Authors and Affiliations
Contributions
DS and JA conceptualised and designed the study; MH analysed the data and performed the statistical analysis. MH and JB drafted the original manuscript. All authors contributed to the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics statements
Ethical approval for the use of the sub-study dataset from the 45 and Up Study was gained from the Human Research Ethics Committees at the University of Technology Sydney on 7th October 2015 (UTS HREC REF NO. 2015000683).
Competing interests
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Adams, J., Bayes, J., Hosseini, M. et al. Annual out-of-pocket expenditure associated with healthcare use among Australian older women with osteoporosis: a cross-sectional study. Arch Osteoporos 16, 148 (2021). https://doi.org/10.1007/s11657-021-01021-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-021-01021-5