Abstract
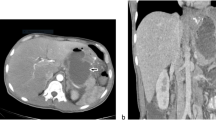
The number of bariatric operations performed each year is increasing. As a result, a rising number of patients in possible need for revisional surgery are referred to bariatric surgeons. But the standard methods of evaluation are often insufficient, and the best strategy remains difficult to choose. In our centre, we have developed 3D gastric computed tomography with air (3D-GCT). The aim of this pilot study was to assess the usefulness of this new image modality as an aid in the decision-making process in patients with failure or complications after bariatric surgery. Twenty patients referred for failure or complications after various bariatric procedures were included in the study. 3D-GCT was performed on a multidetector CT scanner after absorption of effervescent salt diluted in 10 ml of water and IV injection of butylscopolamine. Thin-slice data were transferred to a dedicated 3D workstation creating three-dimensional volume-rendering images of the oesophagus, gastric cavities and anastomoses. The volume of the gastric pouches and the diameter of stoma or anastomoses were measured. No failure or complications were observed. In all patients, 3D-GCT resulted in very impressive precise 3D images of post-surgical anatomy of the stomach. Imaging findings allowed us to identify or to eliminate the common complications of each procedure with a good accuracy, resulting in an aid to choose the best strategy in each patient. In conclusion, our pilot study suggests that 3D-GCT is useful as a decision-making aid in patients with failure or complications after bariatric surgery.








Similar content being viewed by others
References
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19:1605–11.
Spyropoulos C, Kehagias I, Panagiotopoulos S, et al. Revisional bariatric surgery: 13-year experience from a tertiary institution. Arch Surg. 2010;145:173–7.
Gumbs AA, Pomp A, Gagner M. Revisional bariatric surgery for inadequate weight loss. Obes Surg. 2007;17:1137–45.
Lim CS, Liew V, Talbot ML, et al. Revisional bariatric surgery. Obes Surg. 2009;19:827–32.
Dargent J. Lap banding as a redo surgery: “restriction over restriction” may be a relevant bariatric strategy. Obes Surg. 2009;19:1243–9.
Varghese JC, Roy-Choudhury SH. Radiological imaging of the GI tract after bariatric surgery. Gastrointest Endosc. 2009;70:1176–81.
Prosch H, Tscherney R, Kriwanek S, et al. Radiographical imaging of the normal anatomy and complications after gastric banding. Br J Radiol. 2008;81:753–7.
Blachar A, Federle MP, Pealer KM, et al. Radiographic manifestations of normal postoperative anatomy and gastrointestinal complications of bariatric surgery, with emphasis on CT imaging findings. Semin Ultrasound CT MR. 2004;25:239–51.
Trenkner SW. Imaging of morbid obesity procedures and their complications. Abdom Imaging. 2009;34:335–44.
Obstein KL, Thompson CC. Endoscopy after bariatric surgery (with videos). Gastrointest Endosc. 2009;70:1161–6.
Alva S, Eisenberg D, Duffy A, et al. Virtual three-dimensional computed tomography assessment of the gastric pouch following laparoscopic Roux-Y gastric bypass. Obes Surg. 2008;18:364–6.
Alva S, Eisenberg D, Duffy A, et al. A new modality to evaluate the gastric remnant after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2008;4:46–9.
Kawamoto S, Fishman EK. Adjustable laparoscopic gastric banding: demonstrated on multidetector computed tomography with multiplanar reformation and 3-dimensional imaging. J Comput Assist Tomogr. 2009;33:288–90.
Karcz WK, Kuesters S, Marjanovic G, et al. 3D-MSCT gastric pouch volumetry in bariatric surgery-preliminary clinical results. Obes Surg. 2009;19:508–16.
Silecchia G, Catalano C, Gentileschi P, et al. Virtual gastroduodenoscopy: a new look at the bypassed stomach and duodenum after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2002;12:39–48.
Oei TN, Shyn PB, Govindarajulu U, et al. Diagnostic medical radiation dose in patients after laparoscopic bariatric surgery. Obes Surg. 2010;20:569–73.
Gleeson TG, Byrne B, Kenny P, et al. Image quality in low-dose multidetector computed tomography: a pilot study to assess feasibility and dose optimization in whole-body bone imaging. Can Assoc Radiol J 2010 (in press)
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors disclose no commercial interest in the subject of study.
Rights and permissions
About this article
Cite this article
Blanchet, MC., Mesmann, C., Yanes, M. et al. 3D Gastric Computed Tomography as a New Imaging in Patients with Failure or Complication After Bariatric Surgery. OBES SURG 20, 1727–1733 (2010). https://doi.org/10.1007/s11695-010-0256-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0256-2