Abstract
Background
Bariatric surgery has proven a successful approach in the treatment of morbid obesity and its concomitant diseases such as diabetes mellitus and arterial hypertension. Aiming for optimal management of this challenging patient cohort, tailored concepts directly guided by individual patient physiology may outperform standardized care. Implying esophageal pressure measurement and electrical impedance tomography—increasingly applied monitoring approaches to individually adjust mechanical ventilation in challenging circumstances like acute respiratory distress syndrome (ARDS) and intraabdominal hypertension—we compared our institutions standard ventilator regimen with an individually adjusted positive end expiratory pressure (PEEP) level aiming for a positive transpulmonary pressure (P L) throughout the respiratory cycle.
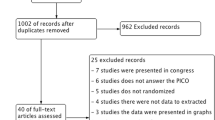
Methods
After obtaining written informed consent, 37 patients scheduled for elective bariatric surgery were studied during mechanical ventilation in reverse Trendelenburg position. Before and after installation of capnoperitoneum, PEEP levels were gradually raised from a standard value of 10 cm H2O until a P L of 0 +/− 1 cm H2O was reached. Changes in ventilation were monitored by electrical impedance tomography (EIT) and arterial blood gases (ABGs) were obtained at the end of surgery and 5 and 60 min after extubation, respectively.
Results
To achieve the goal of a transpulmonary pressure (P L) of 0 cm H2O at end expiration, PEEP levels of 16.7 cm H2O (95% KI 15.6–18.1) before and 23.8 cm H2O (95% KI 19.6–40.4) during capnoperitoneum were necessary. EIT measurements confirmed an optimal PEEP level between 10 and 15 cm H2O before and 20 and 25 cm H2O during capnoperitoneum, respectively. Intra- and postoperative oxygenation did not change significantly.
Conclusion
Patients during laparoscopic bariatric surgery require high levels of PEEP to maintain a positive transpulmonary pressure throughout the respiratory cycle. EIT monitoring allows for non-invasive monitoring of increasing PEEP demand during capnoperitoneum. Individually adjusted PEEP levels did not result in improved postoperative oxygenation.





Similar content being viewed by others
References
Arterburn DE, Maciejewski ML, Tsevat J. Impact of morbid obesity on medical expenditures in adults. Int J Obes. 2005;29:334–9.
Grieve E, Fenwick E, Yang HC, et al. The disproportionate economic burden associated with severe and complicated obesity: a systematic review. Obes Rev. 2013;14:883–94.
Puzziferri N, Roshek 3rd TB, Mayo HG, et al. Long-term follow-up after bariatric surgery: a systematic review. JAMA. 2014;312:934–42.
Dixon JB, Schachter LM, O'Brien PE, et al. Surgical vs conventional therapy for weight loss treatment of obstructive sleep apnea: a randomized controlled trial. JAMA. 308:1142–9.
Reoch J, Mottillo S, Shimony A, et al. Safety of laparoscopic vs open bariatric surgery: a systematic review and meta-analysis. Arch Surg. 2011;146:1314–22.
Pelosi P, Croci M, Ravagnan I, et al. Total respiratory system, lung, and chest wall mechanics in sedated-paralyzed postoperative morbidly obese patients. Chest. 1996;109:144–51.
Behazin N, Jones SB, Cohen RI, et al. Respiratory restriction and elevated pleural and esophageal pressures in morbid obesity. J Appl Physiol. 1985;108:212–8.
El-Dawlatly AA, Al-Dohayan A, Abdel-Meguid ME, et al. The effects of pneumoperitoneum on respiratory mechanics during general anesthesia for bariatric surgery. Obes Surg. 2004;14:212–5.
Dumont L, Mattys M, Mardirosoff C, et al. Changes in pulmonary mechanics during laparoscopic gastroplasty in morbidly obese patients. Acta Anaesthesiol Scand. 1997;41:408–13.
Futier E, Constantin JM, Pelosi P, et al. Noninvasive ventilation and alveolar recruitment maneuver improve respiratory function during and after intubation of morbidly obese patients: a randomized controlled study. Anesthesiology. 114:1354–63.
Perilli V, Sollazzi L, Modesti C, et al. Comparison of positive end-expiratory pressure with reverse Trendelenburg position in morbidly obese patients undergoing bariatric surgery: effects on hemodynamics and pulmonary gas exchange. Obes Surg. 2003;13:605–9.
Futier E, Constantin JM, Petit A, et al. Positive end-expiratory pressure improves end-expiratory lung volume but not oxygenation after induction of anaesthesia. Eur J Anaesthesiol. 2010;27:508–13.
Futier E, Constantin JM, Pelosi P, et al. Intraoperative recruitment maneuver reverses detrimental pneumoperitoneum-induced respiratory effects in healthy weight and obese patients undergoing laparoscopy. Anesthesiology. 2010;113:1310–9.
Neligan PJ, Malhotra G, Fraser M, et al. Noninvasive ventilation immediately after extubation improves lung function in morbidly obese patients with obstructive sleep apnea undergoing laparoscopic bariatric surgery. Anesth Analg. 2010;110:1360–5.
Bardoczky GI, Yernault JC, Houben JJ, et al. Large tidal volume ventilation does not improve oxygenation in morbidly obese patients during anesthesia. Anesth Analg. 1995;81:385–8.
Sutherasan Y, D’Antini D, Pelosi P. Advances in ventilator-associated lung injury: prevention is the target. Expert Rev Respir Med. 8:233–48.
Futier E, Pereira B, Jaber S. Intraoperative low-tidal-volume ventilation. N Engl J Med. 369:1862–3.
Stahl DL, North CM, Lewis A, et al. Case scenario: power of positive end-expiratory pressure: use of esophageal manometry to illustrate pulmonary physiology in an obese patient. Anesthesiology. 2014;121:1320–6.
Talmor D, Sarge T, Malhotra A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med. 2008;359:2095–104.
Grasso S, Terragni P, Birocco A, et al. ECMO criteria for influenza A (H1N1)-associated ARDS: role of transpulmonary pressure. Intensive Care Med. 2012;38:395–403.
Pelosi P, Luecke T, Rocco PR. Chest wall mechanics and abdominal pressure during general anaesthesia in normal and obese individuals and in acute lung injury. Curr Opin Crit Care. 2011;17:72–9.
Sindi A, Piraino T, Alhazzani W, et al. The correlation between esophageal and abdominal pressures in mechanically ventilated patients undergoing laparoscopic surgery. Respir Care. 2013;59:491–6.
Cinnella G, Grasso S, Spadaro S, et al. Effects of recruitment maneuver and positive end-expiratory pressure on respiratory mechanics and transpulmonary pressure during laparoscopic surgery. Anesthesiology. 2012;118:114–22.
Erlandsson K, Odenstedt H, Lundin S, et al. Positive end-expiratory pressure optimization using electric impedance tomography in morbidly obese patients during laparoscopic gastric bypass surgery. Acta Anaesthesiol Scand. 2006;50:833–9.
Maracaja-Neto LF, Vercosa N, Roncally AC, et al. Beneficial effects of high positive end-expiratory pressure in lung respiratory mechanics during laparoscopic surgery. Acta Anaesthesiol Scand. 2009;53:210–7.
Valenza F, Vagginelli F, Tiby A, et al. Effects of the beach chair position, positive end-expiratory pressure, and pneumoperitoneum on respiratory function in morbidly obese patients during anesthesia and paralysis. Anesthesiology. 2007;107:725–32.
Talab HF, Zabani IA, Abdelrahman HS, et al. Intraoperative ventilatory strategies for prevention of pulmonary atelectasis in obese patients undergoing laparoscopic bariatric surgery. Anesth Analg. 2009;109:1511–6.
Schumann R. Anaesthesia for bariatric surgery. Best Pract Res Clin Anaesthesiol. 2011;25:83–93.
Reinius H, Jonsson L, Gustafsson S, et al. Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology. 2009;111:979–87.
Almarakbi WA, Fawzi HM, Alhashemi JA. Effects of four intraoperative ventilatory strategies on respiratory compliance and gas exchange during laparoscopic gastric banding in obese patients. Br J Anaesth. 2009;102:862–8.
Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 369:428–37.
Grasso S, Stripoli T, De Michele M, et al. ARDSnet ventilatory protocol and alveolar hyperinflation: role of positive end-expiratory pressure. Am J Respir Crit Care Med. 2007;176:761–7.
Rodriguez PO, Bonelli I, Setten M, et al. Transpulmonary pressure and gas exchange during decremental PEEP titration in pulmonary ARDS patients. Respir Care. 2012;58:754–63.
Chiumello D, Carlesso E, Cadringher P, et al. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med. 2008;178:346–55.
Washko GR, O'Donnell CR, Loring SH. Volume-related and volume-independent effects of posture on esophageal and transpulmonary pressures in healthy subjects. J Appl Physiol. 2006;100:753–8.
Pelosi P, Goldner M, McKibben A, et al. Recruitment and derecruitment during acute respiratory failure: an experimental study. Am J Respir Crit Care Med. 2001;164:122–30.
Defresne AA, Hans GA, Goffin PJ, et al. Recruitment of lung volume during surgery neither affects the postoperative spirometry nor the risk of hypoxaemia after laparoscopic gastric bypass in morbidly obese patients: a randomized controlled study. Br J Anaesth. 2014;113(3):501–7.
Lumb AB, Greenhill SJ, Simpson MP, et al. Lung recruitment and positive airway pressure before extubation does not improve oxygenation in the post-anaesthesia care unit: a randomized clinical trial. Br J Anaesth. 2010;104:643–7.
Pok EH, Lee WJ. Gastrointestinal metabolic surgery for the treatment of type 2 diabetes mellitus. World J Gastroenterol. 2014;20:14315–28.
Adams ST, Salhab M, Hussain ZI, et al. Obesity-related hypertension and its remission following gastric bypass surgery—a review of the mechanisms and predictive factors. Blood Press. 2012;22:131–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Lars Eichler, Katarzyna Truskowska, Alwin E. Goetz, and Christian Zöllner report support by Carefusion, Höchberg, Germany, who provided the respirator (Avea™) and esophageal pressure probes and Dräger, Lübeck, Germany, who provided the EIT monitor (Pulmovista 500™).
Anna Dupree and Philipp Busch report no conflict of interest.
Rights and permissions
About this article
Cite this article
Eichler, L., Truskowska, K., Dupree, A. et al. Intraoperative Ventilation of Morbidly Obese Patients Guided by Transpulmonary Pressure. OBES SURG 28, 122–129 (2018). https://doi.org/10.1007/s11695-017-2794-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2794-3