Abstract
Objective
Rapid deployment surgical aortic valve replacement has emerged as an alternative to the contemporary sutured valve technique. A difference in transvalvular pressure has been observed clinically between RD-SAVR and contemporary SAVR. A mechanistic inquiry into the impact of the rapid deployment valve inflow frame design on the left ventricular outflow tract and valve hemodynamics is needed.
Methods
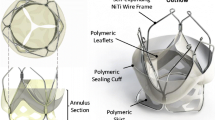
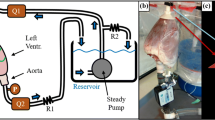
A 23 mm EDWARDS INTUITY Elite rapid deployment valve and a control contemporary, sutured valve, a 23 mm Magna Ease valve, were implanted in an explanted human heart by an experienced cardiac surgeon. Per convention, the rapid deployment valve was implanted with three non-pledgeted, simple guiding sutures, while fifteen pledgeted, mattress sutures were used to implant the contemporary surgical valve. In vitro flow models were created from micro-computed tomography scans of the implanted valves and surrounding cardiac anatomy. Particle image velocimetry and hydrodynamic characterization experiments were conducted in the vicinity of the valves in a validated pulsatile flow loop system.
Results
The rapid deployment and control valves were found to have mean transvalvular pressure gradients of 7.92 ± 0.37 and 10.13 ± 0.48 mmHg, respectively. The inflow frame of the rapid deployment valve formed a larger, more circular, left ventricular outflow tract compared to the control valve. Furthermore, it was found that the presence of the control valve’s sub-annular pledgets compromised its velocity distribution and consequently its pressure gradient.
Conclusions
The rapid deployment valve’s intra-annular inflow frame provides for a larger, left ventricular outflow tract, thus reducing the transvalvular pressure gradient and improving overall hemodynamic performance.






Similar content being viewed by others
References
Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics—2017 update: a report from the american heart association. Circulation. 2017;135:e146–603.
Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary. J Am Coll Cardiol. 2014;63:2438–88.
Di Eusanio M, Phan K. Sutureless aortic valve replacement. Ann Cardiothorac Surg. 2015;4:123–30.
Liakopoulos OJ, Gerfer S, Weider S, et al. Direct comparison of the Edwards Intuity Elite and Sorin Perceval S rapid deployment aortic valves. Ann Thorac Surg. 2018;105:108–14.
Sohn SH, Jang M, Hwang HY, et al. Rapid deployment or sutureless versus conventional bioprosthetic aortic valve replacement: a meta-analysis. J Thorac Cardiovasc Surg. 2018;155(2402–2412):e5.
Phan K, Tsai Y-C, Niranjan N, et al. Sutureless aortic valve replacement: a systematic review and meta-analysis. Ann Cardiothorac Surg. 2015;4:100–11.
Young C, Laufer G, Kocher A, et al. One-year outcomes after rapid-deployment aortic valve replacement. J Thorac Cardiovasc Surg. 2018;155:575–85.
Rahmanian PB. Invited commentary. Ann Thorac Surg. 2018;106(6):1749–50. https://doi.org/10.1016/j.athoracsur.2018.08.004.
Ferrari E, Roduit C, Salamin P, et al. Rapid-deployment aortic valve replacement versus standard bioprosthesis implantation. J Card Surg. 2017;32:322–7.
Jahren SE, Heinisch PP, Wirz J, et al. Hemodynamic performance of Edwards Intuity valve in a compliant aortic root model. In: 2015 37th annual international conference of the IEEE Engineering in Medicine and Biology Society, vol. 2015, IEEE; 2015. p. 3315–18.
Capelli C, Corsini C, Biscarini D, et al. Pledget-armed sutures affect the haemodynamic performance of biologic aortic valve substitutes: a preliminary experimental and computational study. Cardiovasc Eng Technol. 2017;8:17–29.
Bloodworth CH, Pierce EL, Easley TF, et al. Ex vivo methods for informing computational models of the mitral valve. Ann Biomed Eng. 2017;45:496–507.
Midha PA, Raghav V, Okafor I, et al. The effect of valve-in-valve implantation height on sinus flow. Ann Biomed Eng. 2017;45:405–12.
International Organization for Standardization (ISO 5840-3). Cardiovascular implants—cardiac valve prostheses—Part 3: heart valve substitutes implanted by transcatheter techniques. Switzerland, Geneva; 2013.
Gunning PS, Saikrishnan N, McNamara LM, et al. An in vitro evaluation of the impact of eccentric deployment on transcatheter aortic valve hemodynamics. Ann Biomed Eng. 2014;42:1195–206.
Gibson PH, Becher H, Choy JB. Classification of left ventricular size: diameter or volume with contrast echocardiography? Open Hear. 2014;1:e000147.
Borger MA, Moustafine V, Conradi L, et al. A randomized multicenter trial of minimally invasive rapid deployment versus conventional full sternotomy aortic valve replacement. Ann Thorac Surg. 2015;99:17–24.
Bobiarski J, Newcomb AE, Elhenawy AM, et al. One-year hemodynamic comparison of perimount magna with st jude epic aortic bioprostheses. Arch Med Sci. 2013;3:445–51.
Barnhart GR, Accola KD, Grossi EA, et al. TRANSFORM (Multicenter experience with rapid deployment Edwards INTUITY valve system for aortic valve replacement) US clinical trial: performance of a rapid deployment aortic valve. J Thorac Cardiovasc Surg. 2017;153(241–251):e2.
Kocher AA, Laufer G, Haverich A, et al. One-year outcomes of the surgical treatment of aortic stenosis with a next generation surgical aortic valve (TRITON) trial: a prospective multicenter study of rapid-deployment aortic valve replacement with the EDWARDS INTUITY valve system. J Thorac Cardiovasc Surg. 2013;145:110–6.
Andreas M, Wallner S, Habertheuer A, et al. Conventional versus rapid-deployment aortic valve replacement: a single-centre comparison between the Edwards Magna valve and its rapid-deployment successor. Interact Cardiovasc Thorac Surg. 2016;22:799–805.
Wahlers TCW, Andreas M, Rahmanian P, et al. Outcomes of a rapid deployment aortic valve versus its conventional counterpart: a propensity-matched analysis. Innovations. 2018;13(3):177–83. https://doi.org/10.1097/imi.0000000000000509.
Dayan V, Vignolo G, Soca G, et al. Predictors and outcomes of prosthesis-patient mismatch after aortic valve replacement. JACC Cardiovasc Imaging. 2016;9:924–33.
Mannacio V, Mannacio L, Mango E, et al. Severe prosthesis-patient mismatch after aortic valve replacement for aortic stenosis: analysis of risk factors for early and long-term mortality. J Cardiol. 2017;69:333–9.
Theron A, Gariboldi V, Grisoli D, et al. Rapid deployment of aortic bioprosthesis in elderly patients with small aortic annulus. Ann Thorac Surg. 2016;101:1434–41.
Botzenhardt F, Eichinger WB, Guenzinger R, et al. Hemodynamic performance and incidence of patient-prosthesis mismatch of the complete supraannular perimount magna bioprosthesis in the aortic position. Thorac Cardiovasc Surg. 2005;53:226–30.
Rahmanian PB, Kaya S, Eghbalzadeh K, et al. Rapid deployment aortic valve replacement: excellent results and increased effective orifice areas. Ann Thorac Surg. 2018;105:24–30.
Laufer G, Haverich A, Andreas M, et al. Long-term outcomes of a rapid deployment aortic valve: data up to 5 years. Eur J Cardio-Thorac Surg. 2017;52:281–7.
Funding
This study was funded by a research grant from Edwards Lifesciences.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Georgia Tech Research Corporation received a grant from Edwards Lifesciences to carry out this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sadri, V., Bloodworth, C.H., Madukauwa-David, I.D. et al. A mechanistic investigation of the EDWARDS INTUITY Elite valve’s hemodynamic performance. Gen Thorac Cardiovasc Surg 68, 9–17 (2020). https://doi.org/10.1007/s11748-019-01154-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-019-01154-y