Abstract
Purpose of Review
To review findings from empirical studies assessing the role of psychosocial factors in bladder pain syndrome and interstitial cystitis (BPS/IC).
Recent Findings
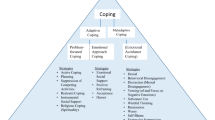
There is a high rate of psychosocial comorbidity in BPS/IC, including elevated levels of anxiety and depression. Recent studies assessing the role of illness perceptions in BPS/IC relate poorer illness perceptions to more unhelpful illness coping patterns. Conversely, positive illness perceptions including self-efficacy in illness management are associated with more adaptive coping behaviors such as exercising and acceptance. New research is investigating the role of trauma in BPS/IC and the impact of suicidality. There is a paucity of psychosocial interventions for BPS/IC over the last 5 years. The three small-scale studies reviewed included a mindfulness-based stress reduction (MBSR) intervention tailored for BPS/IC, a brief self-management intervention designed to increase patient knowledge and symptom management techniques and a 90-min interview aimed at increasing awareness about physiological affective relationship in IC.
Summary
Illness-related cognitions impact illness-related coping behavior, distress, symptom severity, and QoL in BPS/IC. Positive illness perceptions can positively impact behavioral responses to illness and illness outcomes. Trauma, emotion regulation, and suicidality in BPS/IC are important factors for psychosocial interventions and multidisciplinary treatments to address. Insight from the existing evidence base and other functional illness areas such as IBS can be used to inform the design and assessment of interventions aimed to understand and treat BPS/IC as a biopsychosocial illness. The role of healthcare practitioners is fundamental to informing patient perceptions of their illness and providing adequate support for their own self-management approaches.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Doggweiler R, Whitmore KE, Meijlink JM, Drake MJ, Frawley H, Nordling J, et al. A standard for terminology in chronic pelvic pain syndromes: a report from the chronic pelvic pain working group of the international continence society. Neurourol Urodyn. 2017;36(4):984–1008.
Berry SH, Elliott MN, Suttorp M, Bogart LM, Stoto MA, Eggers P, et al. Prevalence of symptoms of bladder pain syndrome/interstitial cystitis among adult females in the United States. J Urol. 2011;186(2):540–4.
Malde S, Palmisani S, Al-Kaisy A, Sahai A. Guideline of guidelines: bladder pain syndrome. BJU Int. 2018;122(5):729–43.
Kanter G, Volpe KA, Dunivan GC, Cichowski SB, Jeppson PC, Rogers RG, et al. Important role of physicians in addressing psychological aspects of interstitial cystitis/bladder pain syndrome (IC/BPS): a qualitative analysis. Int Urogynecol J. 2017;28(2):249–56.
Payne CK, Joyce GF, Wise M, Clemens JQ, Project UD in A. Interstitial cystitis and painful bladder syndrome. J Urol. 2007;177(6):2042–9.
Nickel JC, Tripp DA, Beiko D, Tolls V, Herschorn S, Carr LK, et al. The interstitial cystitis/bladder pain syndrome clinical picture: a perspective from patient life experience. Urol Pract. 2018;5(4):286–92.
Hanno PM, Erickson D, Moldwin R, Faraday MM. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015;193(5):1545–53.
Cashman S, Biers S. Chronic pelvic pain in benign and functional urological conditions: a review and comparison of the UK and European guidelines. J Clin Urol. 2018;11(2):115–21.
Dellis AE, Kostakopoulos N, Papatsoris AG. Is there an effective therapy of interstitial cystitis/bladder pain syndrome? Expert Opin Pharmacother. 2019:1–3.
Tripp DA. Managing psychosocial correlates of urologic chronic pelvic pain syndromes: advice from a urology pain psychologist. Can Urol Assoc J. 2018;12(6 Suppl 3):S175–7.
Clemens JQ, Mullins C, Kusek JW, Kirkali Z, Mayer EA, Rodríguez LV, et al. The MAPP research network: a novel study of urologic chronic pelvic pain syndromes. BMC Urol. 2014;14:57.
Kinsey D, Pretorius S, Glover L, Alexander T. The psychological impact of overactive bladder: a systematic review. J Health Psychol. 2016;21(1):69–81.
•• McKernan LC, Walsh CG, Reynolds WS, Crofford LJ, Dmochowski RR, Williams DA. Psychosocial co-morbidities in interstitial cystitis/bladder pain syndrome (IC/BPS): a systematic review. Neurourol Urodynam. 2018;37(3):926–41 This review comprehensively collates studies assessing the role of psychosocial factors in IC/BPS.
McKernan LC, Nash M, Carr ER. An integrative trauma-based approach toward chronic pain: specific applications to interstitial cystitis/bladder pain syndrome. J Psychother Integr. 2016;26(4):378.
Peters KM, Kalinowski SE, Carrico DJ, Ibrahim IA, Diokno AC. Fact or fiction—is abuse prevalent in patients with interstitial cystitis? Results from a community survey and clinic population. J Urol. 2007;178(3):891–5.
McKernan LC, Johnson BN, Reynolds WS, Williams DA, Cheavens JS, Dmochowski RR, et al. Posttraumatic stress disorder in interstitial cystitis/bladder pain syndrome: relationship to patient phenotype and clinical practice implications. Neurourol Urodynam. 2019b;38(1):353–62.
Chiu C-D, Lee M-H, Chen W-C, Ho HL, Wu H-C. Childhood trauma perpetrated by close others, psychiatric dysfunction, and urological symptoms in patients with interstitial cystitis/bladder pain syndrome. J Psychosom Res. 2017b;93:90–5.
Hepner KA, Watkins KE, Elliott MN, Clemens JQ, Hilton LG, Berry SH. Suicidal ideation among patients with bladder pain syndrome/interstitial cystitis. Urology. 2012;80(2):280–5.
Tripp DA, Nickel JC, Krsmanovic A, Pontari M, Moldwin R, Mayer R, et al. Depression and catastrophizing predict suicidal ideation in tertiary care patients with interstitial cystitis/bladder pain syndrome. Can Urol Assoc J. 2016;10(11–12):383–8.
Vasudevan V, Moldwin R. Addressing quality of life in the patient with interstitial cystitis/bladder pain syndrome. Asian J Urol. 2017;4(1):50–4.
Beckett MK, Elliott MN, Clemens JQ, Ewing B, Berry SH. Consequences of interstitial cystitis/bladder pain symptoms on women’s work participation and income: results from a National Household Sample. J Urol. 2014;191(1):83–8.
Katz L, Tripp DA, Carr LK, Mayer R, Moldwin RM, Nickel JC. Understanding pain and coping in women with interstitial cystitis/bladder pain syndrome. BJU Int. 2017;120(2):286–92.
Muere A, Tripp DA, Nickel JC, Kelly K-L, Mayer R, Pontari M, et al. Depression and coping behaviors are key factors in understanding pain in interstitial cystitis/bladder pain syndrome. Pain Manag Nurs. 2018;19(5):497–505.
Holmes H, Carty J, Lumley M, Tomakowsky J, Pegram S, Dove-Medows E, et al. (508) Self-sacrificing moderates the relationship between emotional distress and pain among women with chronic urogenital pain. J Pain. 2016;17(4):S101–2.
Katz L, Tripp DA, Nickel JC, Krsmanovic A, Muere A, Carr L, et al. What works? Coping and emotion regulation on mental health in women with IC/BPS. Pain Res Manag. 2015;20(3):e28.
Katz L, Tripp DA, Nickel JC, Krsmanovic A, Muere A, Carr LK, et al. P94: illness perceptions mediate the relationship between pain and depression in women with IC/BPS. Pain Res Manag J Can Pain. 2014;19:e31.
Tripp D, Crawford A, Curtis Nickel J, Moldwin R, Carr L, Mayer R, et al. MP39-20 the longitudinal role of catastrophizing and emotion regulation in the relationship between depression and pain in women with interstitial cystitis/bladder pain syndrome. J Urol. 2018;199:e518.
Chiu C-D, Lee M-H, Chen W-C, Ho HL, Wu H-C. Alexithymia and anesthetic bladder capacity in interstitial cystitis/bladder pain syndrome. J Psychosom Res. 2017a;100:15–21.
Leue C, Kruimel J, Vrijens D, Masclee A, Van Os J, Van Koeveringe G. Functional urological disorders: a sensitized defence response in the bladder–gut–brain axis. Nat Rev Urol. 2017;14(3):153–63.
Grundy L, Caldwell A, Brierley S. Mechanisms underlying overactive bladder and interstitial cystitis/bladder pain syndrome. Front Neurosci. 2018;12:931.
Maixner W, Fillingim R, Williams D, Smith S. Overlapping chronic pain conditions: implications for diagnosis and classification. J Pain. 2017;17(9):T93–T107.
McKernan LC, Johnson BN, Crofford LJ, Lumley MA, Bruehl S, Cheavens JS. Posttraumatic stress symptoms mediate the effects of trauma exposure on clinical indicators of central sensitization in patients with chronic pain. Clin J Pain. 2019a;35(5):385–93.
Lai HH, Jemielita T, Sutcliffe S, Bradley CS, Naliboff B, Williams DA, et al. Characterization of whole body pain in urological chronic pelvic pain syndrome at baseline: a MAPP Research Network Study. J Urol. 2017;198(3):622–31.
McKernan L, Cohn J, Bruehl S, Dmochowski R, Reynolds WS. MP29-11 overactive bladder and co-occuring interstitial cystitis/bladder pain syndrome: the role of central sensitization in clinical presentation. J Urol. 2017;4(197):e384.
Tripp DA, Nickel JC, Wong J, Pontari M, Moldwin R, Mayer R, et al. Mapping of pain phenotypes in female patients with bladder pain syndrome/interstitial cystitis and controls. Eur Urol. 2012;62(6):1188–94.
• Naliboff BD, Stephens AJ, Lai HH, Griffith JW, Clemens JQ, Lutgendorf S, et al. Clinical and psychosocial predictors of urological chronic pelvic pain symptom change in 1 year: a prospective study from the MAPP Research Network. J Urol. 2017;198(4):848–57 This study presents the key longitudinal findings from the MAPP network regarding the role of psychosocial factors in IC/BPS.
Lowder JL, Bavendam TG, Berry A, Brady SS, Fitzgerald CM, Fok CS, et al. Terminology for bladder health research in women and girls: prevention of lower urinary tract symptoms transdisciplinary consortium definitions. Neurourol Urodynam. 2019;38(5):1339–52.
Birder LA. Bladder/pelvic pain and neurogenic inflammation. Neurourol. Springer. 2019:433–46.
Jhang J-F, Kuo H-C. Pathomechanism of interstitial cystitis/bladder pain syndrome and mapping the heterogeneity of disease. Int Neurourol J. 2016;20(Suppl 2):S95–104.
Graziottin A, Skaper SD, Fusco M. Mast cells in chronic inflammation, pelvic pain and depression in women. Gynecol Endocrinol. 2014;30(7):472–7.
Nickel JC, Irvine-Bird K, Jianbo L, Shoskes DA. Phenotype-directed management of interstitial cystitis/bladder pain syndrome. Urol. 2014;84(1):175–9.
Wu P, Chen Y, Zhao J, Zhang G, Chen J, Wang J, et al. Urinary microbiome and psychological factors in women with overactive bladder. Front Cell Infect Microbiol. 2017;7:488.
Shoskes DA, Nickel JC, Rackley RR, Pontari MA. Clinical phenotyping in chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: a management strategy for urologic chronic pelvic pain syndromes. Prostate Cancer Prostatic Dis. 2009;12(2):177–83.
Meijlink JM. Bladder pain: the patient perspective. Urologia J. 2017;84(1_suppl):5–7.
O’Hare PG, Hoffmann AR, Allen P, Gordon B, Salin L, Whitmore K. Interstitial cystitis patients’ use and rating of complementary and alternative medicine therapies. Int Urogynecol J. 2013;24(6):977–82.
Epstein RM, Shields CG, Meldrum SC, Fiscella K, Carroll J, Carney PA, et al. Physicians’ responses to patients’ medically unexplained symptoms. Psychosom Med. 2006;68(2):269–76.
Ekman I, Swedberg K, Taft C, Lindseth A, Norberg A, Brink E, et al. Person-centered care — ready for prime time. Eur J Cardiovasc Nurs. 2011;10(4):248–51.
Montori VM, Gafni A, Charles C. A shared treatment decision-making approach between patients with chronic conditions and their clinicians: the case of diabetes. Health Expect. 2006;9(1):25–36.
Kanter G, Komesu YM, Qaedan F, Jeppson PC, Dunivan GC, Cichowski SB, et al. Mindfulness-based stress reduction as a novel treatment for interstitial cystitis/bladder pain syndrome: a randomized controlled trial. Int Urogynecol J. 2016;27(11):1705–11.
Lee M-H, Wu H-C, Tseng C-M, Ko T-L, Weng T-J, Chen Y-F. Health education and symptom flare management using a video-based m-health system for caring women with IC/BPS. Urol. 2018;119:62–9.
Carty J, Lumley M, Holmes H, Tomakowsky J, Schubiner H, Dove-Medows E, et al. (516) The effects of a stress and emotion interview for women with urogenital pain: a randomized trial. J Pain. 2016;17(4):S103.
Funding
This project was conducted with support from the National Institute of Health, National Institute of Diabetes and Digestive and Kidney Diseases award DK118118-01A1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on BPS/Interstitial Cystitis
Rights and permissions
About this article
Cite this article
Windgassen, S., McKernan, L. Cognition, Emotion, and the Bladder: Psychosocial Factors in Bladder Pain Syndrome and Interstitial Cystitis (BPS/IC). Curr Bladder Dysfunct Rep 15, 9–14 (2020). https://doi.org/10.1007/s11884-019-00571-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-019-00571-2