Abstract
Purpose of Review
Myeloproliferative neoplasms are traditionally seen in older adults, making them poorly understood in younger patients. Clinical presentation, genetic landscape, outcomes, and best management practices are inadequately described in this group. Over the past decade, more research has focused on younger patients, and this paper seeks to review and describe the current status of the field.
Recent Findings
A recent review analyzed the available pediatric MPN literature and highlighted the paucity of published data. Pediatric patients showed lower rates of the common mutations found in adults, thrombotic events, and disease transformation to myelofibrosis and acute leukemia. A number of centers have recently shared their experience with young adult patients. Better survival outcomes were confirmed for young adult patients compared to older patients.
Summary
There is still much to learn about myeloproliferative neoplasms in pediatric and young adult patients, but currently available data showing better outcomes is reassuring.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Levine RL, Wadleigh M, Cools J, Ebert BL, Wernig G, Huntly BJ, et al. Activating mutation in the tyrosince kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell. 2005;7(4):387–97. https://doi.org/10.1016/j.ccr.2005.03.023.
Pardanani AD, Levine RL, Lasho T, Pikman Y, Mesa RA, Wadleigh M, et al. MPL515 mutations in myeloproliferative and other myeloid disorders: a study of 1182 patients. Blood. 2006;108(10):3472–6.CALR paper. https://doi.org/10.1182/blood-2006-04-018879.
Nangalia J, Massie CE, Baxter EJ, Nice FL, Gundem G, Wedge DC, et al. Somatic CALR mutations in myeloproliferative neoplasms with nonmutated JAK2. N Engl J Med. 2013;369(25):2391–405. https://doi.org/10.1056/NEJMoa1312542.
Nangalia J, Green TR. The evolving genomic landscape of myeloproliferative neoplasms. Hematology Am Soc Hematol Educ Program. 2014;2014(1):287–96. https://doi.org/10.1182/asheducation-2014.1.287.
Barbui T. How to manage children and young adults with myeloproliferative neoplasms. Leukemia. 2012 Jul;26(7):1452–7. https://doi.org/10.1038/leu.2012.12.
•• Ianotto JC, Curto-Garcia N, Lauermannova M, Radia D, Kiladjian JJ, Harrison CN. Characteristics and outcomes of patients with essential thrombocythemia or polycythemia vera diagnosed before 20 years of age, a systematic review. Haematologica. 2019. https://doi.org/10.3324/haematol.2018.200832. Systematic review on pediatric MPNs.
Hofmann I. Myeloproliferative neoplasms in children. J Hematop. 2015;8(3):143–57. https://doi.org/10.1007/s12308-015-0256-1.
• DeLario M, Sheehan AM, Ataya R, Bertuch AA, Vega C 2nd, Webb CR, et al. Clinical, histopathologic, and genetic features of pediatric primary myelofibrosis--an entity different from adults. Am J Hematol. 2012;87(5):461–4. https://doi.org/10.1002/ajh.23140. Case series of pediatric PMF patients.
• An W, Wan Y, Guo Y, Chen X, Ren Y, Zhang J, et al. CALR mutation screening in pediatric primary myelofibrosis. Pediatr Blood Cancer. 2014;61(12):2256–62. https://doi.org/10.1002/pbc.25211. Case series of pediatric PMF patients.
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, LeBeau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405. https://doi.org/10.1182/blood-2016-03-643544.
Putti MC, Pizzi M, Bertozzi I, Sabattini E, Micalizzi C, Farruggia P, et al. Bone marrow histology for the diagnosis of essential thrombocythemia in children: a multicenter Italian study. Blood. 2017 Jun 1;129(22):3040–2. https://doi.org/10.1182/blood-2017-01-761767.
• Kucine N, Al-Kawaaz M, Hajje D, Bussel J, Orazi A. Difficulty distinguishing essential thrombocythaemia from polycythaemia vera in children with JAK2 V617F-positive myeloproliferative neoplasms. Br J Haematol. 2019;185(1):136–9. Paper detailing issues with WHO diagnostic criteria when used in children.
Martin K. Risk factors for and management of MPN-associated bleeding and thrombosis. Curr Hematol Malig Rep. 2017 Oct;12(5):389–96. https://doi.org/10.1007/s11899-017-0400-3.
Ishida H, Sarashina T, Matsumara R, Umeda K, Mitsui T, Fujita N, et al. Clinical features of children with polycythemia vera, essential thrombocythemia, and primary myelofibrosis in Japan: retrospective nationwide survey. Blood. 2019;134(Supplement_1):2958. https://doi.org/10.1182/blood-2019-123429.
Rampal R, Ahn J, Abdel-Wahab O, Nahas M, Wang K, Lipson D, et al. Genomic and functional analysis of leukemic transformation of myeloproliferative neoplasms. Proc Natl Acad Sci U S A. 2014;111(50):E5401–10. https://doi.org/10.1073/pnas.1407792111.
Yogarajah M, Teffer A. Leukemic transformation in myeloproliferative neoplasms: a literature review on risk, characteristics, and outcome. Mayo Clin Proc. 2017;92(7):1118–28.
• Giona F, Teofili L, Moleti ML, Martini M, Palumbo G, Amendola A. Thrombocythemia and polycythemia in patients younger than 20 years at diagnosis: clinical and biologic features, treatment, and long-term outcome. Blood. 2012;119(10):2219–27. https://doi.org/10.1182/blood-2011-08-371328. Case series of pediatric ET and PV with management recommendations.
Kucine N, Chastain KM, Mahler MB, Bussel JB. Primary thrombocytosis in children. Haematologica. 2014;99(4):620–8.
Randi ML, Bertozzi I, Putti MC. Contemporary management of essential thrombocythemia in children. Expert Rev Hematol. 2019;12(5):367–73.
Mesa RA, Jamieson C, Bhatia R, Deininger MW, Fletcher CD, Gerds AT, et al. NCCN guidelines insights: myeloproliferative neoplasms, version 2.2018. J Natl Compr Cancer Netw. 2017;15(10):1193–207.
Barbui T, Tefferi A, Vannucchi AM, et al. Philadelphia chromosome-negative classical myeloproliferative neoplasms: revised management recommendations from European LeukemiaNet. Leukemia. 2018;32(5):1057–69 Hans IFN.
Pizzi M, Silver RT, Barel A, Orazi A. Recombinant interferon-α in myelofibrosis reduces bone marrow fibrosis, improves its morphology and is associated with clinical response. Mod Pathol. 2015 Oct;28(10):1315–23. https://doi.org/10.1038/modpathol.2015.93.
Ianotto JC, Chauveau A, Boyer-Perrard F, Gyan E, Laribi K, Cony-Makhoul P, et al. Benefits and pitfalls of pegylated interferon-α2a therapy in patients with myeloproliferative neoplasm-associated myelofibrosis: a French Intergroup of Myeloproliferative neoplasms (FIM) study. Haematologica. 2018;103(3):438–46. https://doi.org/10.3324/haematol.2017.181297.
Liberek A, Łuczak G, Korzon M, Szlagatys-Sidorkiewicz A, Bako W, Góra-Gębka M, et al. Tolerance of interferon-alpha therapy in children with chronic hepatitis B. J Paediatr Child Health. 2004;40(5–6):265–9. https://doi.org/10.1111/j.1440-1754.2004.00361.x.
Navid F, Herzog CE, Sandoval J, Daryani VM, Stewart CF, Gattuso J, et al. Feasibility of pegylated interferon in children and young adults with resected high-risk melanoma. Pediatr Blood Cancer. 2016;63(7):1207–13. Published online 2016 Apr 1. https://doi.org/10.1002/pbc.25983.
Kucine N, Bergmann S, Krichevsky S, Jones D, Rytting ME, Resar L. Use of pegylated interferon in six pediatric patients with myeloproliferative neoplasms. Blood. 2019;134(Supplement_1):4194. https://doi.org/10.1182/blood-2019-124023.
Loh ML, Tasian SK, Rabin KR, Brown P, Magoon D, Reid JM, et al. A phase 1 dosing study of ruxolitinib in children with relapsed or refractory solid tumors, leukemias, or myeloproliferative neoplasms: a children’s oncology group phase 1 consortium study (ADVL1011). Pediatr Blood Cancer. 2015;62(10):1717–24. https://doi.org/10.1002/pbc.25575.
• Ginzburg YZ, Feola M, Zimran E, Varkonyi J, Ganz T, Hoffman R. Dysregulated iron metabolism in polycythemia vera: etiology and consequences. Leukemia. 2018;32(10):2105–16. Excellent review paper describing iron deficiency in PV.
Halterman JS, Kaczorowski JM, Aligne CA, Auinger P, Szilagyi PG. Iron deficiency and cognitive acheivement among school-aged children and adolescents in the United States. Pediatrics. 2001;107(6):1381–6. https://doi.org/10.1542/peds.107.6.1381.
Low M, Farrell A, Biggs BA, Pasricha SR. Effects of daily iron supplementation in primary-school-aged children: systematic review and meta-analysis of randomized controlled trials. CMAJ. 2013 Nov 19;185(17):E791–802. https://doi.org/10.1503/cmaj.130628.
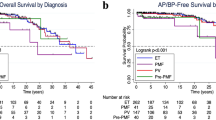
•• Boddu P, Masarova L, Verstovsek S, Strati P, Kantjarian H, Cortes J, et al. Patient characteristics and outcomes in adolescents and young adults with classical Philadelphia chromosome-negative myeloproliferative neoplasms. Ann Hematol. 2018;97(1):109–21. https://doi.org/10.1007/s00277-017-3165-9. Large retrosepctive study of young adult patients with PV, ET, and PMF.
•• Szuber N, Vallapureddy RR, Penna D, Lasho TL, Finke C, Hanson CA, et al. Myeloproliferative neoplasms in the young: Mayo Clinic experience with 361 patients age 40 years or younger. Am J Hematol. 2018 Dec;93(12):1474–84. https://doi.org/10.1002/ajh.25270. Large retrospective study comparing young adults with patients of older ages with PV, ET, and PMF.
• Barzilai M, Kirgner I, Avivi I, Ellis M, Dally N, Rozovski U, et al. Characteristics and outcomes of young adults with Philadelphia-negative myeloproliferative neoplasms. Eur J Haematol. 2019;102(6):504–8. https://doi.org/10.1111/ejh.13232. Retrospective study of young adult MPNs.
• Stein BL, Saraf S, Sobol U, Halpern A, Shammo J, Rondelli D, et al. Age-related differences in disease characteristics and clinical outcomes in polycythemia vera. Leuk Lymphoma. 2013;54(9):1989–95. https://doi.org/10.3109/10428194.2012.759656. Study comparing young adult and older adult patients with PV.
• Palandri F, Latagliata R, Polverelli N, Tieghi A, Crugnola M, Martino B, et al. Mutations and long-term outcome of 217 young patients with essential thrombocythemia or early primary myelofibrosis. Leukemia. 2015;29(6):1344–9. https://doi.org/10.1038/leu.2015.87. Large case series on young adult MPN patients.
Harrison CN, Robinson SE. Myeloproliferative disorders in pregnancy. Hematol Oncol Clin North Am. 2011;25(2):261–75, vii. https://doi.org/10.1016/j.hoc.2011.01.008.
•• Maze D, Kazi S, Gupta V, Malinowski AK, Fazelzad R, Shah PS, et al. Association of treatments for myeloproliferative neoplasms during pregnancy with birth rates and maternal outcomes: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(10):e1912666. https://doi.org/10.1001/jamanetworkopen.2019.12666. Systematic review on pregnancy and MPNs.
Acknowledgements
The author thanks Andrew I. Schafer, MD, and Naveen Pemmaraju, MD, for their input on this paper. NK receives support from the National Heart, Lung, and Blood Institute of the National Institutes of Health (USA), under award #K23HL127223.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Kucine declares that there is no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Myeloproliferative Neoplasms
Rights and permissions
About this article
Cite this article
Kucine, N. Myeloproliferative Neoplasms in Children, Adolescents, and Young Adults. Curr Hematol Malig Rep 15, 141–148 (2020). https://doi.org/10.1007/s11899-020-00571-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11899-020-00571-8