Abstract
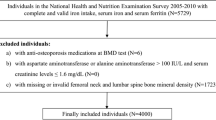
Some studies have suggested an association between serum copper and bone density. Few studies have explored the association between copper intake and osteoporosis and bone mineral density (BMD). Our research aims to assess the associations of copper intake with the risk of osteoporosis in United States adults using the National Health and Nutritional Examination Surveys (NHANES). A total of 8224 individuals were included in our study. Osteoporosis was defined that BMD values surpass 2.5 standard deviations (SD) below the mean of the young adult reference group. Copper intake from diets and supplements was estimated by using two 24-h recall surveys. After adjustment for all the covariates of interest, the odds ratios (ORs) (95% confidence interval (CI)) between the risk of osteoporosis and total copper intake across quartiles 3 and 4 compared with quartile 1 were 0.48 (0.31–0.74) (P < 0.01) and 0.41 (0.26–0.65) (P < 0.01), respectively. The mean total femur BMD and total spine BMD of the highest dietary copper intake quartile (Cu 1.51 mg/d) was 0.03 g/cm2 and 0.02 g/cm2 greater than the lowest quartile. Our results indicate that dietary and total copper intake was positively associated with increasing BMD in US adults and negatively associated with the risk of osteoporosis in US adults.

Similar content being viewed by others
Data Availability
The data of this study will be made available on reasonable request.
Code Availability
The code of this study will be made available on reasonable request.
References
Hendrickx G, Boudin E, Van Hul W (2015) A look behind the scenes: the risk and pathogenesis of primary osteoporosis. Nat Rev Rheumatol 11(8):462–474. https://doi.org/10.1038/nrrheum.2015.48
Wade SW, Strader C, Fitzpatrick LA, Anthony MS, O’Malley CD (2014) Estimating prevalence of osteoporosis: examples from industrialized countries. Arch Osteoporos 9:182. https://doi.org/10.1007/s11657-014-0182-3
Willson T, Nelson SD, Newbold J, Nelson RE, LaFleur J (2015) The clinical epidemiology of male osteoporosis: a review of the recent literature. Clin Epidemiol 7:65–76. https://doi.org/10.2147/clep.S40966
Lunde A, Tell GS, Pedersen AB, Scheike TH, Apalset EM, Ehrenstein V et al (2019) The role of comorbidity in mortality after hip fracture: a nationwide Norwegian study of 38,126 women with hip fracture matched to a general-population comparison cohort. Am J Epidemiol 188(2):398–407. https://doi.org/10.1093/aje/kwy251
Chang J, Yu D, Ji J, Wang N, Yu S, Yu B (2020) The association between the concentration of serum magnesium and postmenopausal osteoporosis. Front Med 7:381. https://doi.org/10.3389/fmed.2020.00381
Zhang H, Wang A, Shen G, Wang X, Liu G, Yang F et al (2021) Hepcidin-induced reduction in iron content and PGC-1β expression negatively regulates osteoclast differentiation to play a protective role in postmenopausal osteoporosis. Aging 13(8):11296–314. https://doi.org/10.18632/aging.202817
Ceylan MN, Akdas S, Yazihan N (2021) Is zinc an important trace element on bone-related diseases and complications? A meta-analysis and systematic review from serum level, dietary intake, and supplementation aspects. Biol Trace Elem Res 199(2):535–549. https://doi.org/10.1007/s12011-020-02193-w
Scheiber I, Dringen R, Mercer JF (2013) Copper: effects of deficiency and overload. Met Ions Life Sci 13:359–387. https://doi.org/10.1007/978-94-007-7500-8_11
Bost M, Houdart S, Oberli M, Kalonji E, Huneau JF, Margaritis I (2016) Dietary copper and human health: current evidence and unresolved issues. J Trace Elem Med Biol 35:107–115. https://doi.org/10.1016/j.jtemb.2016.02.006
Chaudhri MA, Kemmler W, Harsch I, Watling RJ (2009) Plasma copper and bone mineral density in osteopenia: an indicator of bone mineral density in osteopenic females. Biol Trace Elem Res 129(1–3):94–98. https://doi.org/10.1007/s12011-008-8299-0
Mahdavi-Roshan M, Ebrahimi M, Ebrahimi A (2015) Copper, magnesium, zinc and calcium status in osteopenic and osteoporotic post-menopausal women. Clin Cases Miner Bone Metab 12(1):18–21. https://doi.org/10.11138/ccmbm/2015.12.1.01
Qu X, He Z, Qiao H, Zhai Z, Mao Z, Yu Z et al (2018) Serum copper levels are associated with bone mineral density and total fracture. J Orthop Translat 14:34–44. https://doi.org/10.1016/j.jot.2018.05.001
Sadeghi N, Oveisi MR, Jannat B, Hajimahmoodi M, Behzad M, Behfar A et al (2014) The relationship between bone health and plasma zinc, copper lead and cadmium concentration in osteoporotic women. J Environ Health Sci Eng 12(1):125. https://doi.org/10.1186/s40201-014-0125-3
Roughead ZK, Lukaski HC (2003) Inadequate copper intake reduces serum insulin-like growth factor-I and bone strength in growing rats fed graded amounts of copper and zinc. J Nutr 133(2):442–448. https://doi.org/10.1093/jn/133.2.442
Looker AC, Orwoll ES, Johnston CC Jr, Lindsay RL, Wahner HW, Dunn WL et al (1997) Prevalence of low femoral bone density in older U S adults from NHANES III. J Bone Min Res 12(11):1761–8. https://doi.org/10.1359/jbmr.1997.12.11.1761
Cai S, Fan J, Zhu L, Ye J, Rao X, Fan C et al (2020) Bone mineral density and osteoporosis in relation to all-cause and cause-specific mortality in NHANES: a population-based cohort study. Bone 141:115597. https://doi.org/10.1016/j.bone.2020.115597
Arikan DC, Coskun A, Ozer A, Kilinc M, Atalay F, Arikan T (2011) Plasma selenium, zinc, copper and lipid levels in postmenopausal Turkish women and their relation with osteoporosis. Biol Trace Elem Res 144(1–3):407–417. https://doi.org/10.1007/s12011-011-9109-7
Opsahl W, Zeronian H, Ellison M, Lewis D, Rucker RB, Riggins RS (1982) Role of copper in collagen cross-linking and its influence on selected mechanical properties of chick bone and tendon. J Nutr 112(4):708–716. https://doi.org/10.1093/jn/112.4.708
Rucker RB, Kosonen T, Clegg MS, Mitchell AE, Rucker BR, Uriu-Hare JY et al (1998) Copper, lysyl oxidase, and extracellular matrix protein cross-linking. Am J Clin Nutr 67(5 Suppl):996s–1002s. https://doi.org/10.1093/ajcn/67.5.996S
Dahl SL, Rucker RB, Niklason LE (2005) Effects of copper and cross-linking on the extracellular matrix of tissue-engineered arteries. Cell Transplant 14(6):367–374. https://doi.org/10.3727/000000005783982936
Li S, Wang M, Chen X, Li SF, Li-Ling J, Xie HQ (2014) Inhibition of osteogenic differentiation of mesenchymal stem cells by copper supplementation. Cell Prolif 47(1):81–90. https://doi.org/10.1111/cpr.12083
Acknowledgements
The authors thank the National Center for Health Statistics of the Centers for Disease Control and Prevention for sharing the data.
Author information
Authors and Affiliations
Contributions
H.F. Zhang and Y.G. Fan contributed to the conception of the study; S.F. Ni contributed significantly to analysis and manuscript preparation; H.F. Zhang, Y.G. Fan, and S.F. Ni performed the data analyses and wrote the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
NHANES was approved by the National Center for Health Statistics Research Ethics Review Board.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shuangfei Ni and Huafeng Zhang jointly supervised this work.
Rights and permissions
About this article
Cite this article
Fan, Y., Ni, S. & Zhang, H. Associations of Copper Intake with Bone Mineral Density and Osteoporosis in Adults: Data from the National Health and Nutrition Examination Survey . Biol Trace Elem Res 200, 2062–2068 (2022). https://doi.org/10.1007/s12011-021-02845-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-021-02845-5