Abstract
Over the last decade research on cancer stem cells (CSC) significantly contributed to a better understanding of tumor biology. Given their similarity to normal stem cells, i.e. self-renewal and pluripotency the need arises to develop robust protocols for the isolation and characterization of CSCs. As with other malignancies, hepatic tumors are composed of a heterogeneous population of cells including liver cancer stem cells (LCSC). Yet, a precise understanding of why stem cells become cancerous is still lacking. There is unmet need to develop robust protocols for the successful isolation of LCSCs from human tissue resection material as to assist in the development of molecular targeted therapies. Here we review the research progress made in the isolation and characterization of LCSCs by considering a wide range of cell surface markers and sorting methods, as applied to side populations, microsphere cultures and the gradient centrifugation method. We emphasize the different fluorescence activated cell sorting methods and the possibility to enrich LCSCs by immunomagnetic beads. We review the specificity of functional assays by considering ABCG transporter and ALDH1 enzyme activities and evaluate the in vivo tumorigenicity of LCSCs in highly sensitive bioassays. Finally, we evaluate different LCSC markers in association with viral and non-viral liver disease and explore the potential of novel drug delivery systems targeting CD133, EpCAM, CD13 and CD90 for the development of molecular targeted therapies.

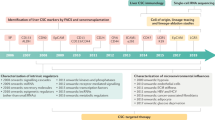
Graphical Abstract





Similar content being viewed by others
Data Availability
All information is given in the manuscript.
Abbreviations
- LCSC:
-
liver cancer stem cells
- IARC:
-
International Agency for Research on Cancer
- CSCs:
-
cancer stem cells
- HCC:
-
hepatocellular carcinoma
- AML:
-
acute myelocytic leukemia
- HPCs:
-
hepatic progenitor cells
- ALDH1:
-
aldehyde Dehydrogenase 1
- OCT-4:
-
octamer-binding transcription factor 4
- PLB:
-
plumbagin
- FGF2:
-
fibroblast growth factor 2
- GEM:
-
gemcitabine
- EGFR:
-
epidermal growth factor receptor
- AFP:
-
alpha-fetoprotein
- SCID:
-
severe combined immunodeficient
- CK19:
-
cytokeratin19
- EpCAM:
-
epithelial cell adhesion molecule
- FACS:
-
fluorescence-activated cell sorting
- MACS:
-
magnetic activated cell sorting
- IMS:
-
immunomagnetic bead sorting
- TMs:
-
thermosensitive magneto liposomes
- 17-AAG:
-
17-allylamino-17-demethoxgeldanamycin
- SFCs:
-
sphere forming cells
- SP:
-
side population
- Rho123:
-
Rhodamine 123
- ABCG2:
-
ATP Binding Cassette Subfamily G Member 2
- UV:
-
ultraviolet
- DCV:
-
Dye Cycle Violet
- LDA:
-
limited dilution method
- HGF:
-
hepatocyte growth factor
- BAAA:
-
BODIPY®-amino acetaldehyde
- PDGC:
-
percoll discontinuous gradient centrifugation method
- MMAF:
-
monomethyl auristatin F
- 5-FU:
-
fluorouracil
- CDDP:
-
cisplatin
- DXR:
-
doxorubicin
- TRAIL:
-
tumor necrosis factor-related apoptosis-inducing ligand
- CAR-T:
-
T cell chimeric antigen receptor
- HBV:
-
hepatitis B virus
- HCV:
-
hepatitis C virus
- RPMI-1640:
-
Gibco Roswell Park Memorial Institute (RPMI) 1640 Medium
- DMEM:
-
Dulbecco’s Modified Eagle’s Medium
- PDX:
-
patient derived xenograft
References
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a Cancer Journal for Clinicians, 68(6), 394–424. https://doi.org/10.3322/caac.21492.
Covey, A. M. (2018). Hepatocellular carcinoma: updates to screening and diagnosis. Journal of the National Comprehensive Cancer Network, 16(5S), 663–665. https://doi.org/10.6004/jnccn.2018.0052.
Chen, J., Jin, R., Zhao, J., Liu, J., Ying, H., Yan, H., Zhou, S., Liang, Y., Huang, D., Liang, X., Yu, H., Lin, H., & Cai, X. (2015). Potential molecular, cellular and microenvironmental mechanism of sorafenib resistance in hepatocellular carcinoma. Cancer Letters, 367(1), 1–11. https://doi.org/10.1016/j.canlet.2015.06.019.
Nguyen, L., Chapel, S., Tran, B. D., & Lacy, S. (2019). Cabozantinib exposure-response analyses of efficacy and safety in patients with advanced hepatocellular carcinoma. Journal of Pharmacokinetics and Pharmacodynamics, 46(6), 577–589. https://doi.org/10.1007/s10928-019-09659-y.
Yu, C. C., Huang, S. Y., Chang, S. F., Liao, K. F., & Chiu, S. C. (2020). The synergistic anti-cancer effects of NVP-BEZ235 and regorafenib in hepatocellular carcinoma. Molecules, 25(10). https://doi.org/10.3390/molecules25102454.
Nassar, D., & Blanpain, C. (2016). Cancer stem cells: basic concepts and therapeutic implications. Annual Review of Pathology, 11, 47–76. https://doi.org/10.1146/annurev-pathol-012615-044438.
Efremov, Y. R., Proskurina, A. S., Potter, E. A., Dolgova, E. V., Efremova, O. V., Taranov, O. S., Ostanin, A. A., Chernykh, E. R., Kolchanov, N. A., & Bogachev, S. S. (2018). Cancer stem cells: emergent nature of tumor emergency. Frontiers in Genetics, 9, 544. https://doi.org/10.3389/fgene.2018.00544.
Wang, X., Wang, R., Bai, S., Xiong, S., Li, Y., Liu, M., Zhao, Z., Wang, Y., Zhao, Y., Chen, W., Billiar, T. R., & Cheng, B. (2019). Musashi2 contributes to the maintenance of CD44v6+ liver cancer stem cells via notch1 signaling pathway. Journal of Experimental & Clinical Cancer Research, 38(1), 505. https://doi.org/10.1186/s13046-019-1508-1.
Chen, L., Wu, M., Ji, C., Yuan, M., Liu, C., & Yin, Q. (2020). Silencing transcription factor FOXM1 represses proliferation, migration, and invasion while inducing apoptosis of liver cancer stem cells by regulating the expression of ALDH2. IUBMB Life, 72(2), 285–295. https://doi.org/10.1002/iub.2166.
Sun, Q., Zhang, Z., Lu, Y., Liu, Q., Xu, X., Xu, J., Liu, Y., Yu, H., Yu, D., & Sun, B. (2019). Loss of xanthine oxidoreductase potentiates propagation of hepatocellular carcinoma stem cells. Hepatology. https://doi.org/10.1002/hep.30978.
Lapidot, T., Sirard, C., Vormoor, J., Murdoch, B., Hoang, T., Caceres-Cortes, J., Minden, M., Paterson, B., Caligiuri, M. A., & Dick, J. E. (1994). A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature, 367(6464), 645–648. https://doi.org/10.1038/367645a0.
Xia, Q., Han, T., Yang, P., Wang, R., Li, H., Zhang, J., & Zhou, X. (2019). MicroRNA-28-5p regulates liver cancer stem cell expansion via IGF-1 pathway. Stem Cells International, 2019, 8734362. https://doi.org/10.1155/2019/8734362.
Si, A., Wang, L., Miao, K., Zhang, R., Ji, H., Lei, Z., Cheng, Z., Fang, X., & Hao, B. (2019). miR-219 regulates liver cancer stem cell expansion via E-cadherin pathway. Cell Cycle, 18(24), 3550–3561. https://doi.org/10.1080/15384101.2019.1691762.
Kahraman, D. C., Kahraman, T., & Cetin-Atalay, R. (2019). Targeting PI3K/Akt/mTOR pathway identifies differential expression and functional role of il8 in liver cancer stem cell enrichment. Molecular Cancer Therapeutics, 18(11), 2146–2157. https://doi.org/10.1158/1535-7163.MCT-19-0004.
Li, X., Strietz, J., Bleilevens, A., Stickeler, E., & Maurer, J. (2020). Chemotherapeutic stress influences epithelial-mesenchymal transition and stemness in cancer stem cells of triple-negative breast cancer. International Journal of Molecular Sciences, 21(2). https://doi.org/10.3390/ijms21020404.
Quaglino, E., Conti, L., & Cavallo, F. (2020). Breast cancer stem cell antigens as targets for immunotherapy. Seminars in Immunology, 101386. https://doi.org/10.1016/j.smim.2020.101386.
Hershey, B. J., Vazzana, R., Joppi, D. L., & Havas, K. M. (2019). Lipid droplets define a sub-population of breast cancer stem cells. Journal of Clinical Medicine, 9(1). https://doi.org/10.3390/jcm9010087.
Acikgoz, E., Tatar, C., & Oktem, G. (2020). Triptolide inhibits CD133(+) /CD44(+) colon cancer stem cell growth and migration through triggering apoptosis and represses epithelial-mesenchymal transition via downregulating expressions of snail, slug, and twist. Journal of Cellular Biochemistry. https://doi.org/10.1002/jcb.29602.
Zhang, L., Niu, H., Ma, J., Yuan, B. Y., Chen, Y. H., Zhuang, Y., Chen, G. W., Zeng, Z. C., & Xiang, Z. L. (2019). The molecular mechanism of LncRNA34a-mediated regulation of bone metastasis in hepatocellular carcinoma. Molecular Cancer, 18(1), 120. https://doi.org/10.1186/s12943-019-1044-9.
Ullmann, P., Nurmik, M., Schmitz, M., Rodriguez, F., Weiler, J., Qureshi-Baig, K., Felten, P., Nazarov, P. V., Nicot, N., Zuegel, N., Haan, S., & Letellier, E. (2019). Tumor suppressor miR-215 counteracts hypoxia-induced colon cancer stem cell activity. Cancer Letters, 450, 32–41. https://doi.org/10.1016/j.canlet.2019.02.030.
Li, X., Ding, J., Li, N., Liu, W., Ding, F., Zheng, H., Ning, Y., Wang, H., Liu, R., & Ren, S. (2019). Synthesis and biological evaluation of celastrol derivatives as anti-ovarian cancer stem cell agents. European Journal of Medicinal Chemistry, 179, 667–679. https://doi.org/10.1016/j.ejmech.2019.06.086.
Fang, Z., Li, T., Chen, W., Wu, D., Qin, Y., Liu, M., Wu, G., He, L., Li, H., & Gu, H. (2019). Gab2 promotes cancer stem cell like properties and metastatic growth of ovarian cancer via downregulation of miR-200c. Experimental Cell Research, 382(1), 111462. https://doi.org/10.1016/j.yexcr.2019.06.007.
Mihanfar, A., Aghazadeh Attari, J., Mohebbi, I., Majidinia, M., Kaviani, M., Yousefi, M., & Yousefi, B. (2019). Ovarian cancer stem cell: a potential therapeutic target for overcoming multidrug resistance. Journal of Cellular Physiology, 234(4), 3238–3253. https://doi.org/10.1002/jcp.26768.
Oishi, N., Yamashita, T., & Kaneko, S. (2014). Molecular biology of liver cancer stem cells. Liver Cancer, 3(2), 71–84. https://doi.org/10.1159/000343863.
Oishi, N., & Wang, X. W. (2011). Novel therapeutic strategies for targeting liver cancer stem cells. International Journal of Biological Sciences, 7(5), 517–535. https://doi.org/10.7150/ijbs.7.517.
Lee, K. D., Kuo, T. K., Whang-Peng, J., Chung, Y. F., Lin, C. T., Chou, S. H., Chen, J. R., Chen, Y. P., & Lee, O. K. (2004). In vitro hepatic differentiation of human mesenchymal stem cells. Hepatology, 40(6), 1275–1284. https://doi.org/10.1002/hep.20469.
Yin, Z., Jiang, K., Li, R., Dong, C., & Wang, L. (2018). Multipotent mesenchymal stromal cells play critical roles in hepatocellular carcinoma initiation, progression and therapy. Molecular Cancer, 17(1), 178. https://doi.org/10.1186/s12943-018-0926-6.
Karakasiliotis, I., & Mavromara, P. (2015). Hepatocellular carcinoma: from hepatocyte to liver cancer stem cell. Frontiers in Physiology, 6, 154. https://doi.org/10.3389/fphys.2015.00154.
Hsiao, P. J., Jao, J. C., Tsai, J. L., Chang, W. T., Jeng, K. S., & Kuo, K. K. (2014). Inorganic arsenic trioxide induces gap junction loss in association with the downregulation of connexin43 and E-cadherin in rat hepatic “stem-like” cells. The Kaohsiung Journal of Medical Sciences, 30(2), 57–67. https://doi.org/10.1016/j.kjms.2013.10.002.
Wang, B., & Jacob, S. T. (2011). Role of cancer stem cells in hepatocarcinogenesis. Genome Medicine, 3(2), 11. https://doi.org/10.1186/gm225.
Fabian, A., Stegner, S., Miarka, L., Zimmermann, J., Lenk, L., Rahn, S., Buttlar, J., Viol, F., Knaack, H., Esser, D., Schauble, S., Grossmann, P., Marinos, G., Hasler, R., Mikulits, W., Saur, D., Kaleta, C., Schafer, H., & Sebens, S. (2019). Metastasis of pancreatic cancer: an uninflamed liver micromilieu controls cell growth and cancer stem cell properties by oxidative phosphorylation in pancreatic ductal epithelial cells. Cancer Letters, 453, 95–106. https://doi.org/10.1016/j.canlet.2019.03.039.
Lee, S. Y., Jeong, E. K., Ju, M. K., Jeon, H. M., Kim, M. Y., Kim, C. H., Park, H. G., Han, S. I., & Kang, H. S. (2017). Induction of metastasis, cancer stem cell phenotype, and oncogenic metabolism in cancer cells by ionizing radiation. Molecular Cancer, 16(1), 10. https://doi.org/10.1186/s12943-016-0577-4.
Lin, S. H., Liu, T., Ming, X., Tang, Z., Fu, L., Schmitt-Kopplin, P., Kanawati, B., Guan, X. Y., & Cai, Z. (2016). Regulatory role of hexosamine biosynthetic pathway on hepatic cancer stem cell marker CD133 under low glucose conditions. Scientific Reports, 6, 21184. https://doi.org/10.1038/srep21184.
Wu, X., Qu, D., Weygant, N., Peng, J., & Houchen, C. W. (2020). Cancer stem cell marker DCLK1 correlates with tumorigenic immune infiltrates in the colon and gastric adenocarcinoma microenvironments. Cancers (Basel), 12(2). https://doi.org/10.3390/cancers12020274.
Ghanei, Z., Jamshidizad, A., Joupari, M. D., & Shamsara, M. (2020). Isolation and characterization of breast cancer stem cell-like phenotype by Oct4 promoter-mediated activity. Journal of Cellular Physiology. https://doi.org/10.1002/jcp.29437.
Bhaduri, A., Di Lullo, E., Jung, D., Muller, S., Crouch, E. E., Espinosa, C. S., Ozawa, T., Alvarado, B., Spatazza, J., Cadwell, C. R., Wilkins, G., Velmeshev, D., Liu, S. J., Malatesta, M., Andrews, M. G., Mostajo-Radji, M. A., Huang, E. J., Nowakowski, T. J., Lim, D. A., Diaz, A., Raleigh, D. R., & Kriegstein, A. R. (2020). Outer radial glia-like cancer stem cells contribute to heterogeneity of glioblastoma. Cell Stem Cell, 26(1), 48–63 e46. https://doi.org/10.1016/j.stem.2019.11.015.
Fathi, F., Rahbarghazi, R., Movassaghpour, A. A., & Rashidi, M. R. (2019). Detection of CD133-marked cancer stem cells by surface plasmon resonance: its application in leukemia patients. Biochimica et Biophysica Acta - General Subjects, 1863(10), 1575–1582. https://doi.org/10.1016/j.bbagen.2019.06.009.
Fu, J. J., Zhou, Y., Shi, X. X., Kang, Y. J., Lu, Z. S., Li, Y., Li, C. M., & Yu, L. (2019). Spontaneous formation of tumor spheroid on a hydrophilic filter paper for cancer stem cell enrichment. Colloids and Surfaces, B: Biointerfaces, 174, 426–434. https://doi.org/10.1016/j.colsurfb.2018.11.038.
Hou, Y. C., Chao, Y. J., Hsieh, M. H., Tung, H. L., Wang, H. C., & Shan, Y. S. (2019). Low CD8(+) T cell infiltration and high PD-L1 expression are associated with level of CD44(+)/CD133(+) cancer stem cells and predict an unfavorable prognosis in pancreatic cancer. Cancers (Basel), 11(4). https://doi.org/10.3390/cancers11040541.
Lin, L., Jou, D., Wang, Y., Ma, H., Liu, T., Fuchs, J., Li, P. K., Lu, J., Li, C., & Lin, J. (2016). STAT3 as a potential therapeutic target in ALDH+ and CD44+/CD24+ stem cell-like pancreatic cancer cells. International Journal of Oncology, 49(6), 2265–2274. https://doi.org/10.3892/ijo.2016.3728.
Chen, J., Li, J., Wu, L., Geng, Y., Yu, J., Chong, C., Wang, M., Gao, Y., Bai, C., Ding, Y., Chen, Y., & Zhang, Q. (2018). Syntheses and anti-pancreatic cancer activities of rakicidin A analogues. European Journal of Medicinal Chemistry, 151, 601–627. https://doi.org/10.1016/j.ejmech.2018.03.078.
Ma, X., Liu, J., Li, J., Li, Y., Le, V. M., Li, S., Liang, X., Liu, L., & Liu, J. (2019). miR-139-5p reverses stemness maintenance and metastasis of colon cancer stem-like cells by targeting E2-2. J Cell Physiol, 234(12), 22703–22718. https://doi.org/10.1002/jcp.28836.
Ke, J., Wu, X., Wu, X., He, X., Lian, L., Zou, Y., He, X., Wang, H., Luo, Y., Wang, L., & Lan, P. (2012). A subpopulation of CD24(+) cells in colon cancer cell lines possess stem cell characteristics. Neoplasma, 59(3), 282–288. https://doi.org/10.4149/neo_2012_036.
atel, S., Waghela, B., Shah, K., Vaidya, F., Mirza, S., Patel, S., Pathak, C., & Rawal, R. (2018). Silibinin, a natural blend in polytherapy formulation for targeting Cd44v6 expressing colon cancer stem cells. Scientific Reports, 8(1), 16985. https://doi.org/10.1038/s41598-018-35069-0.
Zhang, H. (2020). CCND1 silencing suppresses liver cancer stem cell differentiation through inhibiting autophagy. Human Cell, 33(1), 140–147. https://doi.org/10.1007/s13577-019-00295-9.
Wu, D. M., Zheng, Z. H., Zhang, Y. B., Fan, S. H., Zhang, Z. F., Wang, Y. J., Zheng, Y. L., & Lu, J. (2019). Down-regulated lncRNA DLX6-AS1 inhibits tumorigenesis through STAT3 signaling pathway by suppressing CADM1 promoter methylation in liver cancer stem cells. Journal of Experimental & Clinical Cancer Research, 38(1), 237. https://doi.org/10.1186/s13046-019-1239-3.
Ran, R. Z., Chen, J., Cui, L. J., Lin, X. L., Fan, M. M., Cong, Z. Z., Zhang, H., Tan, W. F., Zhang, G. Q., & Zhang, Y. J. (2019). miR-194 inhibits liver cancer stem cell expansion by regulating RAC1 pathway. Experimental Cell Research, 378(1), 66–75. https://doi.org/10.1016/j.yexcr.2019.03.007.
Yang, C., Cai, W. C., Dong, Z. T., Guo, J. W., Zhao, Y. J., Sui, C. J., & Yang, J. M. (2019). lncARSR promotes liver cancer stem cells expansion via STAT3 pathway. Gene, 687, 73–81. https://doi.org/10.1016/j.gene.2018.10.087.
Wang, R., Li, Y., Tsung, A., Huang, H., Du, Q., Yang, M., Deng, M., Xiong, S., Wang, X., Zhang, L., Geller, D. A., Cheng, B., & Billiar, T. R. (2018). iNOS promotes CD24(+)CD133(+) liver cancer stem cell phenotype through a TACE/ADAM17-dependent Notch signaling pathway. Proceedings of the National Academy of Sciences of the United States of America, 115(43), E10127–E10136. https://doi.org/10.1073/pnas.1722100115.
Liu, F., Kong, X., Lv, L., & Gao, J. (2015). MiR-155 targets TP53INP1 to regulate liver cancer stem cell acquisition and self-renewal. FEBS Letters, 589(4), 500–506. https://doi.org/10.1016/j.febslet.2015.01.009.
Ding, W., You, H., Dang, H., LeBlanc, F., Galicia, V., Lu, S. C., Stiles, B., & Rountree, C. B. (2010). Epithelial-to-mesenchymal transition of murine liver tumor cells promotes invasion. Hepatology, 52(3), 945–953. https://doi.org/10.1002/hep.23748.
Ding, W., Mouzaki, M., You, H., Laird, J. C., Mato, J., Lu, S. C., & Rountree, C. B. (2009). CD133+ liver cancer stem cells from methionine adenosyl transferase 1A-deficient mice demonstrate resistance to transforming growth factor (TGF)-beta-induced apoptosis. Hepatology, 49(4), 1277–1286. https://doi.org/10.1002/hep.22743.
Zhang, K., Che, S., Pan, C., Su, Z., Zheng, S., Yang, S., Zhang, H., Li, W., Wang, W., & Liu, J. (2018). The SHH/Gli axis regulates CD90-mediated liver cancer stem cell function by activating the IL6/JAK2 pathway. Journal of Cellular and Molecular Medicine, 22(7), 3679–3690. https://doi.org/10.1111/jcmm.13651.
Xia, W., Lo, C. M., Poon, R. Y. C., Cheung, T. T., Chan, A. C. Y., Chen, L., Yang, S., Tsao, G. S. W., & Wang, X. Q. (2017). Smad inhibitor induces CSC differentiation for effective chemosensitization in cyclin D1- and TGF-beta/Smad-regulated liver cancer stem cell-like cells. Oncotarget, 8(24), 38811–38824. https://doi.org/10.18632/oncotarget.16402.
Jung, J. W., Yoon, S. M., Kim, S., Jeon, Y. H., Yoon, B. H., Yang, S. G., Kim, M. K., Choe, S., & Kuo, M. M. (2016). Bone morphogenetic protein-9 is a potent growth inhibitor of hepatocellular carcinoma and reduces the liver cancer stem cells population. Oncotarget, 7(45), 73754–73768. https://doi.org/10.18632/oncotarget.12062.
Su, R., Nan, H., Guo, H., Ruan, Z., Jiang, L., Song, Y., & Nan, K. (2016). Associations of components of PTEN/AKT/mTOR pathway with cancer stem cell markers and prognostic value of these biomarkers in hepatocellular carcinoma. Hepatology Research, 46(13), 1380–1391. https://doi.org/10.1111/hepr.12687.
ang, L., Zhang, H. B., Li, H., Fu, Y., & Yang, G. S. (2012). miR-548c-5p inhibits proliferation and migration and promotes apoptosis in CD90(+) HepG2 cells. Radiology and Oncology, 46(3), 233–241. https://doi.org/10.2478/v10019-012-0025-z.
Wu, J., Zhu, P., Lu, T., Du, Y., Wang, Y., He, L., Ye, B., Liu, B., Yang, L., Wang, J., Gu, Y., Lan, J., Hao, Y., He, L., & Fan, Z. (2019). The long non-coding RNA LncHDAC2 drives the self-renewal of liver cancer stem cells via activation of Hedgehog signaling. Journal of Hepatology, 70(5), 918–929. https://doi.org/10.1016/j.jhep.2018.12.015.
Zhang, J., Fang, C., Qu, M., Wu, H., Wang, X., Zhang, H., Ma, H., Zhang, Z., Huang, Y., Shi, L., Liang, S., Gao, Z., Song, W., & Wang, X. (2018). CD13 inhibition enhances cytotoxic effect of chemotherapy agents. Frontiers in Pharmacology, 9, 1042. https://doi.org/10.3389/fphar.2018.01042.
Dou, C., Fang, C., Zhao, Y., Fu, X., Zhang, Y., Zhu, D., Wu, H., Liu, H., Zhang, J., Xu, W., Liu, Z., Wang, H., Li, D., & Wang, X. (2017). BC-02 eradicates liver cancer stem cells by upregulating the ROS-dependent DNA damage. International Journal of Oncology, 51(6), 1775–1784. https://doi.org/10.3892/ijo.2017.4159.
Zheng, Y. B., Gong, J. H., Liu, X. J., Li, Y., & Zhen, Y. S. (2017). A CD13-targeting peptide integrated protein inhibits human liver cancer growth by killing cancer stem cells and suppressing angiogenesis. Molecular Carcinogenesis, 56(5), 1395–1404. https://doi.org/10.1002/mc.22600.
Sun, Z. P., Zhang, J., Shi, L. H., Zhang, X. R., Duan, Y., Xu, W. F., Dai, G., & Wang, X. J. (2015). Aminopeptidase N inhibitor 4cc synergizes antitumor effects of 5-fluorouracil on human liver cancer cells through ROS-dependent CD13 inhibition. Biomedicine & Pharmacotherapy, 76, 65–72. https://doi.org/10.1016/j.biopha.2015.10.023.
Kim, H. M., Haraguchi, N., Ishii, H., Ohkuma, M., Okano, M., Mimori, K., Eguchi, H., Yamamoto, H., Nagano, H., Sekimoto, M., Doki, Y., & Mori, M. (2012). Increased CD13 expression reduces reactive oxygen species, promoting survival of liver cancer stem cells via an epithelial-mesenchymal transition-like phenomenon. Annals of Surgical Oncology, 19(Suppl 3), S539–S548. https://doi.org/10.1245/s10434-011-2040-5.
i, B., Liu, D., Yang, P., Li, H. Y., & Wang, D. (2019). miR-613 inhibits liver cancer stem cell expansion by regulating SOX9 pathway. Gene, 707, 78–85. https://doi.org/10.1016/j.gene.2019.05.015.
Wang, X., Sun, W., Shen, W., Xia, M., Chen, C., Xiang, D., Ning, B., Cui, X., Li, H., Li, X., Ding, J., & Wang, H. (2016). Long non-coding RNA DILC regulates liver cancer stem cells via IL-6/STAT3 axis. Journal of Hepatology, 64(6), 1283–1294. https://doi.org/10.1016/j.jhep.2016.01.019.
Wang, R., Sun, Q., Wang, P., Liu, M., Xiong, S., Luo, J., Huang, H., Du, Q., Geller, D. A., & Cheng, B. (2016). Notch and Wnt/beta-catenin signaling pathway play important roles in activating liver cancer stem cells. Oncotarget, 7(5), 5754–5768. https://doi.org/10.18632/oncotarget.6805.
Gedaly, R., Galuppo, R., Musgrave, Y., Angulo, P., Hundley, J., Shah, M., Daily, M. F., Chen, C., Cohen, D. A., Spear, B. T., & Evers, B. M. (2013). PKI-587 and sorafenib alone and in combination on inhibition of liver cancer stem cell proliferation. The Journal of Surgical Research, 185(1), 225–230. https://doi.org/10.1016/j.jss.2013.05.016.
Zhu, K., Li, J., Li, J., Sun, J., Guo, Y., Tian, H., Li, L., Zhang, C., Shi, M., Kong, G., & Li, Z. (2019). Ring1 promotes the transformation of hepatic progenitor cells into cancer stem cells through the Wnt/beta-catenin signaling pathway. Journal of Cellular Biochemistry. https://doi.org/10.1002/jcb.29496.
Li, T. Y., & Chiang, B. H. (2019). 4-Acetylantroquinonol B from antrodia cinnamomea enhances immune function of dendritic cells against liver cancer stem cells. Biomedicine & Pharmacotherapy, 109, 2262–2269. https://doi.org/10.1016/j.biopha.2018.11.101.
Jiang, Z. B., Ma, B. Q., Liu, S. G., Li, J., Yang, G. M., Hou, Y. B., Si, R. H., Gao, P., & Yan, H. T. (2019). miR-365 regulates liver cancer stem cells via RAC1 pathway. Molecular Carcinogenesis, 58(1), 55–65. https://doi.org/10.1002/mc.22906.
Qin, X. Y., Suzuki, H., Honda, M., Okada, H., Kaneko, S., Inoue, I., Ebisui, E., Hashimoto, K., Carninci, P., Kanki, K., Tatsukawa, H., Ishibashi, N., Masaki, T., Matsuura, T., Kagechika, H., Toriguchi, K., Hatano, E., Shirakami, Y., Shiota, G., Shimizu, M., Moriwaki, H., & Kojima, S. (2018). Prevention of hepatocellular carcinoma by targeting MYCN-positive liver cancer stem cells with acyclic retinoid. Proceedings of the National Academy of Sciences of the United States of America, 115(19), 4969–4974. https://doi.org/10.1073/pnas.1802279115.
Wang, C., Fu, S. Y., Wang, M. D., Yu, W. B., Cui, Q. S., Wang, H. R., Huang, H., Dong, W., Zhang, W. W., Li, P. P., Lin, C., Pan, Z. Y., Yang, Y., Wu, M. C., & Zhou, W. P. (2017). Zinc finger protein X-linked promotes expansion of EpCAM(+) cancer stem-like cells in hepatocellular carcinoma. Molecular Oncology, 11(5), 455–469. https://doi.org/10.1002/1878-0261.12036.
Zhu, M., Li, W., Lu, Y., Dong, X., Lin, B., Chen, Y., Zhang, X., Guo, J., & Li, M. (2017). HBx drives alpha fetoprotein expression to promote initiation of liver cancer stem cells through activating PI3K/AKT signal pathway. International Journal of Cancer, 140(6), 1346–1355. https://doi.org/10.1002/ijc.30553.
io, K., Yamashita, T., Okada, H., Kondo, M., Hayashi, T., Hara, Y., Nomura, Y., Zeng, S. S., Yoshida, M., Hayashi, T., Sunagozaka, H., Oishi, N., Honda, M., & Kaneko, S. (2015). Defeating EpCAM(+) liver cancer stem cells by targeting chromatin remodeling enzyme CHD4 in human hepatocellular carcinoma. Journal of Hepatology, 63(5), 1164–1172. https://doi.org/10.1016/j.jhep.2015.06.009.
Tyms, A. S. (1986). Polyamine inhibitors. The Journal of Antimicrobial Chemotherapy, 17(2), 131–135. https://doi.org/10.1093/jac/17.2.131.
Yamashita, T., Honda, M., Nio, K., Nakamoto, Y., Yamashita, T., Takamura, H., Tani, T., Zen, Y., & Kaneko, S. (2010). Oncostatin m renders epithelial cell adhesion molecule-positive liver cancer stem cells sensitive to 5-Fluorouracil by inducing hepatocytic differentiation. Cancer Research, 70(11), 4687–4697. https://doi.org/10.1158/0008-5472.CAN-09-4210.
Su, M., Wang, P., Wang, X., Zhang, M., Wei, S., Liu, K., Han, S., Han, X., Deng, Y., & Shen, L. (2019). Nuclear CD44 mediated by importin beta participated in naive genes transcriptional regulation in C3A-iCSCs. International Journal of Biological Sciences, 15(6), 1252–1260. https://doi.org/10.7150/ijbs.28235.
Kim, S., Cho, C. Y., Lee, D., Song, D. G., Kim, H. J., Jung, J. W., Kim, J. E., Park, D., Lee, H., Um, H., Park, J., Choi, Y., Kim, Y., Nam, S. H., & Lee, J. W. (2018). CD133-induced TM4SF5 expression promotes sphere growth via recruitment and blocking of protein tyrosine phosphatase receptor type F (PTPRF). Cancer Letters, 438, 219–231. https://doi.org/10.1016/j.canlet.2018.09.009.
Lee, J. H., Hur, W., Hong, S. W., Kim, J. H., Kim, S. M., Lee, E. B., & Yoon, S. K. (2017). ELK3 promotes the migration and invasion of liver cancer stem cells by targeting HIF-1alpha. Oncology Reports, 37(2), 813–822. https://doi.org/10.3892/or.2016.5293.
Zou, H., Cao, X., Xiao, Q., Sheng, X., Ren, K., Quan, M., Song, Z., Li, D., Zheng, Y., Zeng, W., Cao, J., & Peng, Y. (2016). Synergistic inhibition of characteristics of liver cancer stem-like cells with a combination of sorafenib and 8-bromo-7-methoxychrysin in SMMC-7721 cell line. Oncology Reports, 36(3), 1731–1738. https://doi.org/10.3892/or.2016.4973.
Vilchez, V., Turcios, L., Zaytseva, Y., Stewart, R., Lee, E. Y., Maynard, E., Shah, M. B., Daily, M. F., Tzeng, C. W., Davenport, D., Castellanos, A. L., Krohmer, S., Hosein, P. J., Evers, B. M., & Gedaly, R. (2016). Cancer stem cell marker expression alone and in combination with microvascular invasion predicts poor prognosis in patients undergoing transplantation for hepatocellular carcinoma. American Journal of Surgery, 212(2), 238–245. https://doi.org/10.1016/j.amjsurg.2015.12.019.
Yan, H., Dong, X., Zhong, X., Ye, J., Zhou, Y., Yang, X., Shen, J., & Zhang, J. (2014). Inhibitions of epithelial to mesenchymal transition and cancer stem cells-like properties are involved in miR-148a-mediated anti-metastasis of hepatocellular carcinoma. Molecular Carcinogenesis, 53(12), 960–969. https://doi.org/10.1002/mc.22064.
Cheng, Z., Lei, Z., Yang, P., Si, A., Xiang, D., Zhou, J., & Huser, N. (2019). Long non-coding RNA THOR promotes liver cancer stem cells expansion via beta-catenin pathway. Gene, 684, 95–103. https://doi.org/10.1016/j.gene.2018.10.051.
Zeng, C., Zhang, Y., Park, S. C., Eun, J. R., Nguyen, N. T., Tschudy-Seney, B., Jung, Y. J., Theise, N. D., Zern, M. A., & Duan, Y. (2015). CD34(+) liver cancer stem cells were formed by fusion of hepatobiliary stem/progenitor cells with hematopoietic precursor-derived myeloid intermediates. Stem Cells and Development, 24(21), 2467–2478. https://doi.org/10.1089/scd.2015.0202.
Park, S. C., Zeng, C., Tschudy-Seney, B., Nguyen, N. T., Eun, J. R., Zhang, Y., Ramsamooj, R., Zhang, Y., Zhao, M., Theise, N. D., Zhou, H., Zern, M. A., & Duan, Y. (2015). Clonogenically culturing and expanding CD34+ liver cancer stem cells in vitro. Stem Cells and Development, 24(13), 1506–1514. https://doi.org/10.1089/scd.2015.0022.
Park, S. C., Nguyen, N. T., Eun, J. R., Zhang, Y., Jung, Y. J., Tschudy-Seney, B., Trotsyuk, A., Lam, A., Ramsamooj, R., Zhang, Y., Theise, N. D., Zern, M. A., & Duan, Y. (2015). Identification of cancer stem cell subpopulations of CD34(+) PLC/PRF/5 that result in three types of human liver carcinomas. Stem Cells and Development, 24(8), 1008–1021. https://doi.org/10.1089/scd.2014.0405.
Jiang, X., Liu, F., Wang, Y., & Gao, J. (2019). Secreted protein acidic and rich in cysteine promotes epithelial-mesenchymal transition of hepatocellular carcinoma cells and acquisition of cancerstem cell phenotypes. Journal of Gastroenterology and Hepatology, 34(10), 1860–1868. https://doi.org/10.1111/jgh.14692.
Zhang, J., Pei, Y., Yang, W., Yang, W., Chen, B., Zhao, X., & Long, S. (2019). Cytoglobin ameliorates the stemness of hepatocellular carcinoma via coupling oxidative-nitrosative stress signals. Molecular Carcinogenesis, 58(3), 334–343. https://doi.org/10.1002/mc.22931.
Chen, X., Huan, H., Liu, C., Luo, Y., Shen, J., Zhuo, Y., Zhang, Z., & Qian, C. (2019). Deacetylation of beta-catenin by SIRT1 regulates self-renewal and oncogenesis of liver cancer stem cells. Cancer Letters, 463, 1–10. https://doi.org/10.1016/j.canlet.2019.07.021.
Wang, Y., Zhu, P., Luo, J., Wang, J., Liu, Z., Wu, W., Du, Y., Ye, B., Wang, D., He, L., Ren, W., Wang, J., Sun, X., Chen, R., Tian, Y., & Fan, Z. (2019). LncRNA HAND2-AS1 promotes liver cancer stem cell self-renewal via BMP signaling. EMBO J, 38(17), e101110. https://doi.org/10.15252/embj.2018101110.
Huang, Y., Zhou, B., Luo, H., Mao, J., Huang, Y., Zhang, K., Mei, C., Yan, Y., Jin, H., Gao, J., Su, Z., Pang, P., Li, D., & Shan, H. (2019). ZnAs@SiO2 nanoparticles as a potential anti-tumor drug for targeting stemness and epithelial-mesenchymal transition in hepatocellular carcinoma via SHP-1/JAK2/STAT3 signaling. Theranostics, 9(15), 4391–4408. https://doi.org/10.7150/thno.32462.
Qureshi-Baig, K., Kuhn, D., Viry, E., Pozdeev, V. I., Schmitz, M., Rodriguez, F., Ullmann, P., Koncina, E., Nurmik, M., Frasquilho, S., Nazarov, P. V., Zuegel, N., Boulmont, M., Karapetyan, Y., Antunes, L., Val, D., Mittelbronn, M., Janji, B., Haan, S., & Letellier, E. (2019). Hypoxia-induced autophagy drives colorectal cancer initiation and progression by activating the PRKC/PKC-EZR (ezrin) pathway. Autophagy, 1–17. https://doi.org/10.1080/15548627.2019.1687213.
Chaudhary, A. K., Mondal, G., Kumar, V., Kattel, K., & Mahato, R. I. (2017). Chemosensitization and inhibition of pancreatic cancer stem cell proliferation by overexpression of microRNA-205. Cancer Letters, 402, 1–8. https://doi.org/10.1016/j.canlet.2017.05.007.
Suetsugu, A., Nagaki, M., Aoki, H., Motohashi, T., Kunisada, T., & Moriwaki, H. (2006). Characterization of CD133+ hepatocellular carcinoma cells as cancer stem/progenitor cells. Biochemical and Biophysical Research Communications, 351(4), 820–824. https://doi.org/10.1016/j.bbrc.2006.10.128.
Song, Y., Park, I. S., Kim, J., & Seo, H. R. (2019). Actinomycin D inhibits the expression of the cystine/glutamate transporter xCT via attenuation of CD133 synthesis in CD133(+) HCC. Chemico-Biological Interactions, 309, 108713. https://doi.org/10.1016/j.cbi.2019.06.026.
Zhang, K., Che, S., Su, Z., Zheng, S., Zhang, H., Yang, S., Li, W., & Liu, J. (2018). CD90 promotes cell migration, viability and sphereforming ability of hepatocellular carcinoma cells. International Journal of Molecular Medicine, 41(2), 946–954. https://doi.org/10.3892/ijmm.2017.3314.
Liu, Z., Dai, X., Wang, T., Zhang, C., Zhang, W., Zhang, W., Zhang, Q., Wu, K., Liu, F., Liu, Y., & Wu, J. (2017). Hepatitis B virus PreS1 facilitates hepatocellular carcinoma development by promoting appearance and self-renewal of liver cancer stem cells. Cancer Letters, 400, 149–160. https://doi.org/10.1016/j.canlet.2017.04.017.
Fausto, N., & Campbell, J. S. (2003). The role of hepatocytes and oval cells in liver regeneration and repopulation. Mechanisms of Development, 120(1), 117–130. https://doi.org/10.1016/s0925-4773(02)00338-6.
Hashimoto, O., Shimizu, K., Semba, S., Chiba, S., Ku, Y., Yokozaki, H., & Hori, Y. (2011). Hypoxia induces tumor aggressiveness and the expansion of CD133-positive cells in a hypoxia-inducible factor-1alpha-dependent manner in pancreatic cancer cells. Pathobiology, 78(4), 181–192. https://doi.org/10.1159/000325538.
mmervoll, H., Hoem, D., Sakariassen, P. O., Steffensen, O. J., & Molven, A. (2008). Expression of the “stem cell marker” CD133 in pancreas and pancreatic ductal adenocarcinomas. BMC Cancer, 8, 48. https://doi.org/10.1186/1471-2407-8-48.
Osmond, T. L., Broadley, K. W., & McConnell, M. J. (2010). Glioblastoma cells negative for the anti-CD133 antibody AC133 express a truncated variant of the CD133 protein. International Journal of Molecular Medicine, 25(6), 883–888. https://doi.org/10.3892/ijmm_00000418.
Lv, D., Ma, Q. H., Duan, J. J., Wu, H. B., Zhao, X. L., Yu, S. C., & Bian, X. W. (2016). Optimized dissociation protocol for isolating human glioma stem cells from tumorspheres via fluorescence-activated cell sorting. Cancer Letters, 377(1), 105–115. https://doi.org/10.1016/j.canlet.2016.04.022.
Sakariassen, P. O., Immervoll, H., & Chekenya, M. (2007). Cancer stem cells as mediators of treatment resistance in brain tumors: status and controversies. Neoplasia, 9(11), 882–892. https://doi.org/10.1593/neo.07658.
Miraglia, S., Godfrey, W., Yin, A. H., Atkins, K., Warnke, R., Holden, J. T., Bray, R. A., Waller, E. K., & Buck, D. W. (1997). A novel five-transmembrane hematopoietic stem cell antigen: isolation, characterization, and molecular cloning. Blood, 90(12), 5013-5021. https://www.ncbi.nlm.nih.gov/pubmed/9389721
Annabi, B., Lachambre, M. P., Plouffe, K., Sartelet, H., & Beliveau, R. (2009). Modulation of invasive properties of CD133+ glioblastoma stem cells: a role for MT1-MMP in bioactive lysophospholipid signaling. Molecular Carcinogenesis, 48(10), 910–919. https://doi.org/10.1002/mc.20541.
Yang, Y., Hao, E., Pan, X., Tan, D., Du, Z., Xie, J., Hou, X., Deng, J., & Wei, K. (2019). Gomisin M2 from Baizuan suppresses breast cancer stem cell proliferation in a zebrafish xenograft model. Aging (Albany NY), 11(19), 8347–8361. https://doi.org/10.18632/aging.102323.
Zhou, X., Chen, L., Wang, A., Ma, Y., Zhang, H., & Zhu, Y. (2015). Multifunctional fluorescent magnetic nanoparticles for lung cancer stem cells research. Colloids and Surfaces, B: Biointerfaces, 134, 431–439. https://doi.org/10.1016/j.colsurfb.2015.07.030.
Simbulan-Rosenthal, C. M., Dougherty, R., Vakili, S., Ferraro, A. M., Kuo, L. W., Alobaidi, R., Aljehane, L., Gaur, A., Sykora, P., Glasgow, E., Agarwal, S., & Rosenthal, D. S. (2019). CRISPR-Cas9 knockdown and induced expression of CD133 reveal essential roles in melanoma invasion and metastasis. Cancers (Basel), 11(10). https://doi.org/10.3390/cancers11101490.
Lin, X., Chen, W., Wei, F., Zhou, B. P., Hung, M. C., & Xie, X. (2017). Nanoparticle delivery of miR-34a eradicates long-term-cultured breast cancer stem cells via targeting C22ORF28 directly. Theranostics, 7(19), 4805–4824. https://doi.org/10.7150/thno.20771.
Yang, R., An, L. Y., Miao, Q. F., Li, F. M., Han, Y., Wang, H. X., Liu, D. P., Chen, R., & Tang, S. Q. (2016). Effective elimination of liver cancer stem-like cells by CD90 antibody targeted thermosensitive magnetoliposomes. Oncotarget, 7(24), 35894–35916. https://doi.org/10.18632/oncotarget.9116.
ang, R., Tang, Q., Miao, F., An, Y., Li, M., Han, Y., Wang, X., Wang, J., Liu, P., & Chen, R. (2015). Inhibition of heat-shock protein 90 sensitizes liver cancer stem-like cells to magnetic hyperthermia and enhances anti-tumor effect on hepatocellular carcinoma-burdened nude mice. International Journal of Nanomedicine, 10, 7345–7358. https://doi.org/10.2147/IJN.S93758.
Quan, M. F., Xiao, L. H., Liu, Z. H., Guo, H., Ren, K. Q., Liu, F., Cao, J. G., & Deng, X. Y. (2013). 8-bromo-7-methoxychrysin inhibits properties of liver cancer stem cells via downregulation of beta-catenin. World Journal of Gastroenterology, 19(43), 7680–7695. https://doi.org/10.3748/wjg.v19.i43.7680.
Boulter, L., Guest, R. V., Kendall, T. J., Wilson, D. H., Wojtacha, D., Robson, A. J., Ridgway, R. A., Samuel, K., Van Rooijen, N., Barry, S. T., Wigmore, S. J., Sansom, O. J., & Forbes, S. J. (2015). WNT signaling drives cholangiocarcinoma growth and can be pharmacologically inhibited. The Journal of Clinical Investigation, 125(3), 1269–1285. https://doi.org/10.1172/JCI76452.
Dezso, K., Paku, S., Papp, V., Turanyi, E., & Nagy, P. (2009). Architectural and immunohistochemical characterization of biliary ductules in normal human liver. Stem Cells and Development, 18(10), 1417–1422. https://doi.org/10.1089/scd.2009.0110.
Yin, S., Li, J., Hu, C., Chen, X., Yao, M., Yan, M., Jiang, G., Ge, C., Xie, H., Wan, D., Yang, S., Zheng, S., & Gu, J. (2007). CD133 positive hepatocellular carcinoma cells possess high capacity for tumorigenicity. International Journal of Cancer, 120(7), 1444–1450. https://doi.org/10.1002/ijc.22476.
Hur, W., Ryu, J. Y., Kim, H. U., Hong, S. W., Lee, E. B., Lee, S. Y., & Yoon, S. K. (2017). Systems approach to characterize the metabolism of liver cancer stem cells expressing CD133. Scientific Reports, 7, 45557. https://doi.org/10.1038/srep45557.
Lee, S. H., Hyun, S. K., Kim, H. B., Kang, C. D., & Kim, S. H. (2016). Potential role of CD133 expression in the susceptibility of human liver cancer stem-like cells to TRAIL. Oncology Research, 24(6), 495–509. https://doi.org/10.3727/096504016X14685034103950.
Yoshikawa, S., Zen, Y., Fujii, T., Sato, Y., Ohta, T., Aoyagi, Y., & Nakanuma, Y. (2009). Characterization of CD133+ parenchymal cells in the liver: histology and culture. World Journal of Gastroenterology, 15(39), 4896–4906. https://doi.org/10.3748/wjg.15.4896.
amashita, M., Wada, H., Eguchi, H., Ogawa, H., Yamada, D., Noda, T., Asaoka, T., Kawamoto, K., Gotoh, K., Umeshita, K., Doki, Y., & Mori, M. (2016). A CD13 inhibitor, ubenimex, synergistically enhances the effects of anticancer drugs in hepatocellular carcinoma. International Journal of Oncology, 49(1), 89–98. https://doi.org/10.3892/ijo.2016.3496.
Haraguchi, N., Ishii, H., Mimori, K., Tanaka, F., Ohkuma, M., Kim, H. M., Akita, H., Takiuchi, D., Hatano, H., Nagano, H., Barnard, G. F., Doki, Y., & Mori, M. (2010). CD13 is a therapeutic target in human liver cancer stem cells. The Journal of Clinical Investigation, 120(9), 3326–3339. https://doi.org/10.1172/JCI42550.
Yamashita, T., Honda, M., Nakamoto, Y., Baba, M., Nio, K., Hara, Y., Zeng, S. S., Hayashi, T., Kondo, M., Takatori, H., Yamashita, T., Mizukoshi, E., Ikeda, H., Zen, Y., Takamura, H., Wang, X. W., & Kaneko, S. (2013). Discrete nature of EpCAM+ and CD90+ cancer stem cells in human hepatocellular carcinoma. Hepatology, 57(4), 1484–1497. https://doi.org/10.1002/hep.26168.
Inada, M., Benten, D., Cheng, K., Joseph, B., Berishvili, E., Badve, S., Logdberg, L., Dabeva, M., & Gupta, S. (2008). Stage-specific regulation of adhesion molecule expression segregates epithelial stem/progenitor cells in fetal and adult human livers. Hepatology International, 2(1), 50–62. https://doi.org/10.1007/s12072-007-9023-4.
Bae, J. S., Noh, S. J., Jang, K. Y., Park, H. S., Chung, M. J., Park, C. K., & Moon, W. S. (2012). Expression and role of epithelial cell adhesion molecule in dysplastic nodule and hepatocellular carcinoma. International Journal of Oncology, 41(6), 2150–2158. https://doi.org/10.3892/ijo.2012.1631.
Schmelzer, E., & Reid, L. M. (2008). EpCAM expression in normal, non-pathological tissues. Frontiers in Bioscience, 13, 3096–3100. https://doi.org/10.2741/2911.
Schmelzer, E., Zhang, L., Bruce, A., Wauthier, E., Ludlow, J., Yao, H. L., Moss, N., Melhem, A., McClelland, R., Turner, W., Kulik, M., Sherwood, S., Tallheden, T., Cheng, N., Furth, M. E., & Reid, L. M. (2007). Human hepatic stem cells from fetal and postnatal donors. The Journal of Experimental Medicine, 204(8), 1973–1987. https://doi.org/10.1084/jem.20061603.
Tsuchiya, A., Suda, T., Oda, C., Kimura, A., Hosaka, K., Kimura, N., Tominaga, K., Hayashi, K., Takamura, M., & Terai, S. (2019). EpCAM- and/or NCAM-expressing hepatocellular carcinoma in which behavior of hepatic progenitor cell marker-positive cells are followed. Case Reports in Gastroenterology, 13(1), 118–124. https://doi.org/10.1159/000498913.
Zhang, R. R., Zheng, Y. W., Li, B., Nie, Y. Z., Ueno, Y., Tsuchida, T., & Taniguchi, H. (2018). Hepatic stem cells with self-renewal and liver repopulation potential are harbored in CDCP1-positive subpopulations of human fetal liver cells. Stem Cell Research & Therapy, 9(1), 29. https://doi.org/10.1186/s13287-017-0747-3.
Thakolwiboon, S., Zhu, J., Liang, Q., Welling, T. H., Zhang, M., & Lubman, D. M. (2014). Heterogeneity of the CD90(+) population in different stages of hepatocarcinogenesis. The Journal of Proteomics & Bioinformatics, 7(10), 296–302. https://doi.org/10.4172/jpb.1000332.
Weiss, T. S., & Dayoub, R. (2017). Thy-1 (CD90)-Positive Hepatic Progenitor Cells, hepatoctyes, and non-parenchymal liver cells isolated from human livers. Methods in Molecular Biology, 1506, 75–89. https://doi.org/10.1007/978-1-4939-6506-9_5.
Conigliaro, A., Costa, V., Lo Dico, A., Saieva, L., Buccheri, S., Dieli, F., Manno, M., Raccosta, S., Mancone, C., Tripodi, M., De Leo, G., & Alessandro, R. (2015). CD90+ liver cancer cells modulate endothelial cell phenotype through the release of exosomes containing H19 lncRNA. Molecular Cancer, 14, 155. https://doi.org/10.1186/s12943-015-0426-x.
Lu, J. W., Chang, J. G., Yeh, K. T., Chen, R. M., Tsai, J. J., & Hu, R. M. (2011). Overexpression of Thy1/CD90 in human hepatocellular carcinoma is associated with HBV infection and poor prognosis. Acta Histochemica, 113(8), 833–838. https://doi.org/10.1016/j.acthis.2011.01.001.
Ho, C. M., Ho, S. L., Shun, C. T., Lee, P. H., Chen, Y. H., Chien, C. S., Chen, H. L., & Hu, R. H. (2017). Histopathological evidence for the existence of primary liver progenitor cell cancer: insight from cancer stem cell pathobiology. Discovery Medicine, 23(124), 41-50. https://www.ncbi.nlm.nih.gov/pubmed/28245426
Yang, Z. F., Ho, D. W., Ng, M. N., Lau, C. K., Yu, W. C., Ngai, P., Chu, P. W., Lam, C. T., Poon, R. T., & Fan, S. T. (2008). Significance of CD90+ cancer stem cells in human liver cancer. Cancer Cell, 13(2), 153–166. https://doi.org/10.1016/j.ccr.2008.01.013.
Ho, D. W., Tsui, Y. M., Sze, K. M., Chan, L. K., Cheung, T. T., Lee, E., Sham, P. C., Tsui, S. K., Lee, T. K., & Ng, I. O. (2019). Single-cell transcriptomics reveals the landscape of intra-tumoral heterogeneity and stemness-related subpopulations in liver cancer. Cancer Letters, 459, 176–185. https://doi.org/10.1016/j.canlet.2019.06.002.
Qiu, Q., Hernandez, J. C., Dean, A. M., Rao, P. H., & Darlington, G. J. (2011). CD24-positive cells from normal adult mouse liver are hepatocyte progenitor cells. Stem Cells and Development, 20(12), 2177–2188. https://doi.org/10.1089/scd.2010.0352.
Li, L., Chen, J., Ge, C., Zhao, F., Chen, T., Tian, H., Li, J., & Li, H. (2019). CD24 isoform a promotes cell proliferation, migration and invasion and is downregulated by EGR1 in hepatocellular carcinoma. Oncotargets and Therapy, 12, 1705–1716. https://doi.org/10.2147/OTT.S196506.
Lu, S., Yao, Y., Xu, G., Zhou, C., Zhang, Y., Sun, J., Jiang, R., Shao, Q., & Chen, Y. (2018). CD24 regulates sorafenib resistance via activating autophagy in hepatocellular carcinoma. Cell Death & Disease, 9(6), 646. https://doi.org/10.1038/s41419-018-0681-z.
Lee, T. K., Castilho, A., Cheung, V. C., Tang, K. H., Ma, S., & Ng, I. O. (2011). CD24(+) liver tumor-initiating cells drive self-renewal and tumor initiation through STAT3-mediated NANOG regulation. Cell Stem Cell, 9(1), 50–63. https://doi.org/10.1016/j.stem.2011.06.005.
Su, X., Shi, Y., Zou, X., Lu, Z. N., Xie, G., Yang, J. Y. H., Wu, C. C., Cui, X. F., He, K. Y., Luo, Q., Qu, Y. L., Wang, N., Wang, L., & Han, Z. G. (2017). Single-cell RNA-Seq analysis reveals dynamic trajectories during mouse liver development. BMC Genomics, 18(1), 946. https://doi.org/10.1186/s12864-017-4342-x.
Wang, J. H., Gong, C., Guo, F. J., Zhou, X., Zhang, M. S., Qiu, H., Chao, T. F., Liu, Y., Qin, L., & Xiong, H. H. (2020). Knockdown of STIP1 inhibits the invasion of CD133positive cancer stemlike cells of the osteosarcoma MG63 cell line via the PI3K/Akt and ERK1/2 pathways. International Journal of Molecular Medicine, 46(6), 2251–2259. https://doi.org/10.3892/ijmm.2020.4764.
Weng, C. H., Wu, C. S., Wu, J. C., Kung, M. L., Wu, M. H., & Tai, M. H. (2020). Cisplatin-induced giant cells formation is involved in chemoresistance of melanoma cells. International Journal of Molecular Sciences, 21(21). https://doi.org/10.3390/ijms21217892.
Lin, Q., Wu, Z., Yue, X., Yu, X., Wang, Z., Song, X., Xu, L., He, Y., Ge, Y., Tan, S., Wang, T., Song, H., Yuan, D., Gong, Y., Gao, L., Liang, X., & Ma, C. (2020). ZHX2 restricts hepatocellular carcinoma by suppressing stem cell-like traits through KDM2A-mediated H3K36 demethylation. EBioMedicine, 53, 102676. https://doi.org/10.1016/j.ebiom.2020.102676.
hi, R., Liu, L., Wang, F., He, Y., Niu, Y., Wang, C., Zhang, X., Zhang, X., Zhang, H., Chen, M., & Wang, Y. (2020). Downregulation of cytokeratin 18 induces cellular partial EMT and stemness through increasing EpCAM expression in breast cancer. Cellular Signalling, 76, 109810. https://doi.org/10.1016/j.cellsig.2020.109810.
Chen, X., Chen, T., Zhang, L., Wang, Z., Zhou, Q., Huang, T., Ge, C., Xu, H., Zhu, M., Zhao, F., Yao, M., Tian, H., Li, H., Zhu, X., & Li, J. (2020). Cyclodextrin-mediated formation of porous RNA nanospheres and their application in synergistic targeted therapeutics of hepatocellular carcinoma. Biomaterials, 261, 120304. https://doi.org/10.1016/j.biomaterials.2020.120304.
Ferreri, A. J. M., Calimeri, T., Ponzoni, M., Curnis, F., Conte, G. M., Scarano, E., Rrapaj, E., De Lorenzo, D., Cattaneo, D., Fallanca, F., Nonis, A., Foppoli, M., Lopedote, P., Citterio, G., Politi, L. S., Sassone, M., Angelillo, P., Guggiari, E., Steffanoni, S., Tarantino, V., Ciceri, F., Bordignon, C., Anzalone, N., & Corti, A. (2020). Improving the antitumor activity of R-CHOP with NGR-hTNF in primary CNS lymphoma: final results of a phase 2 trial. Blood Advances, 4(15), 3648–3658. https://doi.org/10.1182/bloodadvances.2020002270.
Zhai, M., Yang, Z., Zhang, C., Li, J., Jia, J., Zhou, L., Lu, R., Yao, Z., & Fu, Z. (2020). APN-mediated phosphorylation of BCKDK promotes hepatocellular carcinoma metastasis and proliferation via the ERK signaling pathway. Cell Death & Disease, 11(5), 396. https://doi.org/10.1038/s41419-020-2610-1.
Cao, J., Zang, J., Kong, X., Zhao, C., Chen, T., Ran, Y., Dong, H., Xu, W., & Zhang, Y. (2019). Leucine ureido derivatives as aminopeptidase N inhibitors using click chemistry. Part II. Bioorganic & Medicinal Chemistry, 27(6), 978–990. https://doi.org/10.1016/j.bmc.2019.01.041.
Lei, J. H., Yan, W., Luo, C. H., Guo, Y. M., Zhang, Y. Y., Wang, X. H., & Su, X. J. (2020). Cytotoxicity of nonylphenol on spermatogonial stem cells via phosphatidylinositol-3-kinase/protein kinase B/mammalian target of rapamycin pathway. World Journal of Stem Cells, 12(6), 500–513. https://doi.org/10.4252/wjsc.v12.i6.500.
Yang, C. C., Chen, Y. T., Wallace, C. G., Chen, K. H., Cheng, B. C., Sung, P. H., Li, Y. C., Ko, S. F., Chang, H. W., & Yip, H. K. (2019). Early administration of empagliflozin preserved heart function in cardiorenal syndrome in rat. Biomedicine & Pharmacotherapy, 109, 658–670. https://doi.org/10.1016/j.biopha.2018.10.095.
Sulaiman, A., McGarry, S., Chambers, J., Al-Kadi, E., Phan, A., Li, L., Mediratta, K., Dimitroulakos, J., Addison, C., Li, X., & Wang, L. (2020). Targeting hypoxia sensitizes TNBC to cisplatin and promotes inhibition of both bulk and cancer stem cells. International Journal of Molecular Sciences, 21(16). https://doi.org/10.3390/ijms21165788.
hou, J., Wang, H., Che, J., Xu, L., Yang, W., Li, Y., & Zhou, W. (2020). Silencing of microRNA-135b inhibits invasion, migration, and stemness of CD24(+)CD44(+) pancreatic cancer stem cells through JADE-1-dependent AKT/mTOR pathway. Cancer Cell International, 20, 134. https://doi.org/10.1186/s12935-020-01210-1.
Zhao, Y., Lu, Q., Li, C., Wang, X., Jiang, L., Huang, L., Wang, C., & Chen, H. (2019). PRMT1 regulates the tumour-initiating properties of esophageal squamous cell carcinoma through histone H4 arginine methylation coupled with transcriptional activation. Cell Death & Disease, 10(5), 359. https://doi.org/10.1038/s41419-019-1595-0.
Wang, K. J., Wang, C., Dai, L. H., Yang, J., Huang, H., Ma, X. J., Zhou, Z., Yang, Z. Y., Xu, W. D., Hua, M. M., Lu, X., Zeng, S. X., Wang, H. Q., Zhang, Z. S., Cheng, Y. Q., Liu, D., Tian, Q. Q., Sun, Y. H., & Xu, C. L. (2019). Targeting an autocrine regulatory loop in cancer stem-like cells impairs the progression and chemotherapy resistance of bladder cancer. Clinical Cancer Research, 25(3), 1070–1086. https://doi.org/10.1158/1078-0432.CCR-18-0586.
Barzegar Behrooz, A., Syahir, A., & Ahmad, S. (2019). CD133: beyond a cancer stem cell biomarker. Journal of Drug Targeting, 27(3), 257–269. https://doi.org/10.1080/1061186X.2018.1479756.
Li, A., Dubey, S., Varney, M. L., Dave, B. J., & Singh, R. K. (2003). IL-8 directly enhanced endothelial cell survival, proliferation, and matrix metalloproteinases production and regulated angiogenesis. Journal of Immunology, 170(6), 3369–3376. https://doi.org/10.4049/jimmunol.170.6.3369.
Aghajani, M., Mansoori, B., Mohammadi, A., Asadzadeh, Z., & Baradaran, B. (2019). New emerging roles of CD133 in cancer stem cell: Signaling pathway and miRNA regulation. Journal of Cellular Physiology, 234(12), 21642–21661. https://doi.org/10.1002/jcp.28824.
Huang, L., Yang, Y., Yang, F., Liu, S., Zhu, Z., Lei, Z., & Guo, J. (2018). Functions of EpCAM in physiological processes and diseases (Review). International Journal of Molecular Medicine, 42(4), 1771–1785. https://doi.org/10.3892/ijmm.2018.3764.
Munz, M., Baeuerle, P. A., & Gires, O. (2009). The emerging role of EpCAM in cancer and stem cell signaling. Cancer Research, 69(14), 5627–5629. https://doi.org/10.1158/0008-5472.CAN-09-0654.
Munz, M., Kieu, C., Mack, B., Schmitt, B., Zeidler, R., & Gires, O. (2004). The carcinoma-associated antigen EpCAM upregulates c-myc and induces cell proliferation. Oncogene, 23(34), 5748–5758. https://doi.org/10.1038/sj.onc.1207610.
Chaves-Perez, A., Mack, B., Maetzel, D., Kremling, H., Eggert, C., Harreus, U., & Gires, O. (2013). EpCAM regulates cell cycle progression via control of cyclin D1 expression. Oncogene, 32(5), 641–650. https://doi.org/10.1038/onc.2012.75.
Maaser, K., & Borlak, J. (2008). A genome-wide expression analysis identifies a network of EpCAM-induced cell cycle regulators. British Journal of Cancer, 99(10), 1635–1643. https://doi.org/10.1038/sj.bjc.6604725.
Mina-Osorio, P. (2008). The moonlighting enzyme CD13: old and new functions to target. Trends in Molecular Medicine, 14(8), 361–371. https://doi.org/10.1016/j.molmed.2008.06.003.
Wickstrom, M., Larsson, R., Nygren, P., & Gullbo, J. (2011). Aminopeptidase N (CD13) as a target for cancer chemotherapy. Cancer Science, 102(3), 501–508. https://doi.org/10.1111/j.1349-7006.2010.01826.x.
Kumar, A., Bhanja, A., Bhattacharyya, J., & Jaganathan, B. G. (2016). Multiple roles of CD90 in cancer. Tumour Biology, 37(9), 11611–11622. https://doi.org/10.1007/s13277-016-5112-0.
Chen, W. C., Chang, Y. S., Hsu, H. P., Yen, M. C., Huang, H. L., Cho, C. Y., Wang, C. Y., Weng, T. Y., Lai, P. T., Chen, C. S., Lin, Y. J., & Lai, M. D. (2015). Therapeutics targeting CD90-integrin-AMPK-CD133 signal axis in liver cancer. Oncotarget, 6(40), 42923–42937. https://doi.org/10.18632/oncotarget.5976.
Altevogt, P., Sammar, M., Huser, L., & Kristiansen, G. (2020). Novel insights into the function of CD24: A driving force in cancer. International Journal of Cancer. 10.1002/ijc.33249
Jaggupilli, A., & Elkord, E. (2012). Significance of CD44 and CD24 as cancer stem cell markers: an enduring ambiguity. Clinical & Developmental Immunology, 2012, 708036. https://doi.org/10.1155/2012/708036.
Ayre, D. C., & Christian, S. L. (2016). CD24: a rheostat that modulates cell surface receptor signaling of diverse receptors. Frontiers in Cell and Development Biology, 4, 146. https://doi.org/10.3389/fcell.2016.00146.
Wang, C., Wang, M. D., Cheng, P., Huang, H., Dong, W., Zhang, W. W., Li, P. P., Lin, C., Pan, Z. Y., Wu, M. C., & Zhou, W. P. (2017). Hepatitis B virus X protein promotes the stem-like properties of OV6(+) cancer cells in hepatocellular carcinoma. Cell Death & Disease, 8(1), e2560. https://doi.org/10.1038/cddis.2016.493.
Haraguchi, N., Utsunomiya, T., Inoue, H., Tanaka, F., Mimori, K., Barnard, G. F., & Mori, M. (2006). Characterization of a side population of cancer cells from human gastrointestinal system. Stem Cells, 24(3), 506–513. https://doi.org/10.1634/stemcells.2005-0282.
Chiba, T., Kita, K., Zheng, Y. W., Yokosuka, O., Saisho, H., Iwama, A., Nakauchi, H., & Taniguchi, H. (2006). Side population purified from hepatocellular carcinoma cells harbors cancer stem cell-like properties. Hepatology, 44(1), 240–251. https://doi.org/10.1002/hep.21227.
Shi, G. M., Xu, Y., Fan, J., Zhou, J., Yang, X. R., Qiu, S. J., Liao, Y., Wu, W. Z., Ji, Y., Ke, A. W., Ding, Z. B., He, Y. Z., Wu, B., Yang, G. H., Qin, W. Z., Zhang, W., Zhu, J., Min, Z. H., & Wu, Z. Q. (2008). Identification of side population cells in human hepatocellular carcinoma cell lines with stepwise metastatic potentials. Journal of Cancer Research and Clinical Oncology, 134(11), 1155–1163. https://doi.org/10.1007/s00432-008-0407-1.
Marquardt, J. U., Raggi, C., Andersen, J. B., Seo, D., Avital, I., Geller, D., Lee, Y. H., Kitade, M., Holczbauer, A., Gillen, M. C., Conner, E. A., Factor, V. M., & Thorgeirsson, S. S. (2011). Human hepatic cancer stem cells are characterized by common stemness traits and diverse oncogenic pathways. Hepatology, 54(3), 1031–1042. https://doi.org/10.1002/hep.24454.
Jeng, K. S., Sheen, I. S., Jeng, W. J., Yu, M. C., Hsiau, H. I., Chang, F. Y., & Tsai, H. H. (2013). Activation of the sonic hedgehog signaling pathway occurs in the CD133 positive cells of mouse liver cancer Hepa 1-6 cells. Oncotargets and Therapy, 6, 1047–1055. https://doi.org/10.2147/OTT.S44828.
Li, R., Qian, N., Tao, K., You, N., Wang, X., & Dou, K. (2010). MicroRNAs involved in neoplastic transformation of liver cancer stem cells. Journal of Experimental & Clinical Cancer Research, 29, 169. https://doi.org/10.1186/1756-9966-29-169.
Moreira, H., Szyjka, A., Paliszkiewicz, K., & Barg, E. (2019). Prooxidative activity of celastrol induces apoptosis, DNA damage, and cell cycle arrest in drug-resistant human colon cancer cells. Oxidative Medicine and Cellular Longevity, 2019(6793957). https://doi.org/10.1155/2019/6793957.
Kohara, H., Watanabe, K., Shintou, T., Nomoto, T., Okano, M., Shirai, T., Miyazaki, T., & Tabata, Y. (2013). The use of fluorescent indoline dyes for side population analysis. Biomaterials, 34(4), 1024–1032. https://doi.org/10.1016/j.biomaterials.2012.10.059.
Mathew, G., Timm Jr., E. A., Sotomayor, P., Godoy, A., Montecinos, V. P., Smith, G. J., & Huss, W. J. (2009). ABCG2-mediated DyeCycle Violet efflux defined side population in benign and malignant prostate. Cell Cycle, 8(7), 1053–1061. https://doi.org/10.4161/cc.8.7.8043.
Dotse, E., & Bian, Y. (2016). Isolation of colorectal cancer stem-like cells. Cytotechnology, 68(4), 609–619. https://doi.org/10.1007/s10616-014-9806-0.
Wang, L., Li, X., Zhang, W., Yang, Y., Meng, Q., Wang, C., Xin, X., Jiang, X., Song, S., Lu, Y., Pu, H., Gui, X., Li, T., Xu, J., Li, J., Jia, S., & Lu, D. (2019). miR24-2 promotes malignant progression of human liver cancer stem cells by enhancing tyrosine kinase src epigenetically. Molecular Therapy. https://doi.org/10.1016/j.ymthe.2019.10.015.
Yan, X., Liu, X., Wang, Z., Cheng, Q., Ji, G., Yang, H., Wan, L., Ge, C., Zeng, Q., Huang, H., Xi, J., He, L., Nan, X., Yue, W., & Pei, X. (2019). MicroRNA4865p functions as a tumor suppressor of proliferation and cancer stemlike cell properties by targeting Sirt1 in liver cancer. Oncology Reports, 41(3) 1938-1948. https://doi.org/10.3892/or.2018.6930.
Zhu, Y. T., Zhao, Z., Fu, X. Y., Luo, Y., Lei, C. Y., Chen, W., Li, F., Pang, S. Y., Chen, S. S., & Tan, W. L. (2014). The granulocyte macrophage-colony stimulating factor surface modified MB49 bladder cancer stem cells vaccine against metastatic bladder cancer. Stem Cell Research, 13(1), 111–122. https://doi.org/10.1016/j.scr.2014.04.006.
Zhu, Y. T., Lei, C. Y., Luo, Y., Liu, N., He, C. W., Chen, W., Li, F., Deng, Y. J., & Tan, W. L. (2013). A modified method for isolation of bladder cancer stem cells from a MB49 murine cell line. BMC Urology, 13, 57. https://doi.org/10.1186/1471-2490-13-57.
Xu, R., Yu, M., & Li, Y. L. (2018). Isolation, identification and biological characteristics of the stem cells from mucoepidermoid carcinoma of the salivary gland. Shanghai Kou Qiang Yi Xue, 27(1), 39-42. https://www.ncbi.nlm.nih.gov/pubmed/29946639
Wang, N., Li, M. Y., Liu, Y., Yu, J., Ren, J., Zheng, Z., Wang, S., Yang, S., Yang, S. L., Liu, L. P., Hu, B. G., Chong, C. C., Merchant, J. L., Lai, P. B., & Chen, G. G. (2020). ZBP-89 negatively regulates self-renewal of liver cancer stem cells via suppression of Notch1 signaling pathway. Cancer Letters, 472, 70–80. https://doi.org/10.1016/j.canlet.2019.12.026.
Han, S., Shin, H., Lee, J. K., Liu, Z., Rabadan, R., Lee, J., Shin, J., Lee, C., Yang, H., Kim, D., Kim, S. H., Kim, J., Oh, J. W., Kong, D. S., Lee, J. I., Seol, H. J., Choi, J. W., Kang, H. J., & Nam, D. H. (2019). Secretome analysis of patient-derived GBM tumor spheres identifies midkine as a potent therapeutic target. Experimental & Molecular Medicine, 51(12), 147. https://doi.org/10.1038/s12276-019-0351-y.
Wang, C. H., Qi, S. T., Fan, J., Pan, J., Peng, J. X., Nie, J., Bao, Y., Liu, Y. W., Zhang, X., & Liu, Y. (2019). Identification of tumor stem-like cells in admanatimomatous craniopharyngioma and determination of these cells’ pathological significance. Journal of Neurosurgery, 1–11. https://doi.org/10.3171/2019.5.JNS19565.
Wang, H., Paczulla, A. M., Konantz, M., & Lengerke, C. (2018). In vitro tumorigenic assay: the tumor spheres assay. Methods in Molecular Biology, 1692, 77–87. https://doi.org/10.1007/978-1-4939-7401-6_7.
Zheng, B. N., Ding, C. H., Chen, S. J., Zhu, K., Shao, J., Feng, J., Xu, W. P., Cai, L. Y., Zhu, C. P., Duan, W., Ding, J., Zhang, X., Luo, C., & Xie, W. F. (2019). Targeting PRMT5 activity inhibits the malignancy of hepatocellular carcinoma by promoting the transcription of HNF4alpha. Theranostics, 9(9), 2606–2617. https://doi.org/10.7150/thno.32344.
Ma, Y. S., Lv, Z. W., Yu, F., Chang, Z. Y., Cong, X. L., Zhong, X. M., Lu, G. X., Zhu, J., & Fu, D. (2018). MicroRNA-302a/d inhibits the self-renewal capability and cell cycle entry of liver cancer stem cells by targeting the E2F7/AKT axis. Journal of Experimental & Clinical Cancer Research, 37(1), 252. https://doi.org/10.1186/s13046-018-0927-8.
Wen, Q., Xu, C., Zhou, J., Liu, N. M., Cui, Y. H., Quan, M. F., Cao, J. G., & Ren, K. Q. (2019). 8-bromo-7-methoxychrysin suppress stemness of SMMC-7721 cells induced by co-culture of liver cancer stem-like cells with hepatic stellate cells. BMC Cancer, 19(1), 224. https://doi.org/10.1186/s12885-019-5419-5.
Prasetyanti, P. R., Zimberlin, C., De Sousa, E. M. F., & Medema, J. P. (2013). Isolation and propagation of colon cancer stem cells. Methods in Molecular Biology, 1035, 247–259. https://doi.org/10.1007/978-1-62703-508-8_21.
Phillips, T. M., McBride, W. H., & Pajonk, F. (2006). The response of CD24(-/low)/CD44+ breast cancer-initiating cells to radiation. Journal of the National Cancer Institute, 98(24), 1777–1785. https://doi.org/10.1093/jnci/djj495.
Ponti, D., Costa, A., Zaffaroni, N., Pratesi, G., Petrangolini, G., Coradini, D., Pilotti, S., Pierotti, M. A., & Daidone, M. G. (2005). Isolation and in vitro propagation of tumorigenic breast cancer cells with stem/progenitor cell properties. Cancer Research, 65(13), 5506–5511. https://doi.org/10.1158/0008-5472.CAN-05-0626.
Koenders, S. T. A., Wijaya, L. S., Erkelens, M. N., Bakker, A. T., van der Noord, V. E., van Rooden, E. J., Burggraaff, L., Putter, P. C., Botter, E., Wals, K., van den Elst, H., den Dulk, H., Florea, B. I., van de Water, B., van Westen, G. J. P., Mebius, R. E., Overkleeft, H. S., Le Devedec, S. E., & van der Stelt, M. (2019). Development of a retinal-based probe for the profiling of retinaldehyde dehydrogenases in cancer cells. ACS Central Science, 5(12), 1965–1974. https://doi.org/10.1021/acscentsci.9b01022.
Lokman, N. A., Price, Z. K., Hawkins, E. K., Macpherson, A. M., Oehler, M. K., & Ricciardelli, C. (2019). 4-Methylumbelliferone inhibits cancer stem cell activation and overcomes chemoresistance in ovarian cancer. Cancers (Basel), 11(8). https://doi.org/10.3390/cancers11081187.
Raved, D., Tokatly-Latzer, I., Anafi, L., Harari-Steinberg, O., Barshack, I., Dekel, B., & Pode-Shakked, N. (2019). Blastemal NCAM(+)ALDH1(+) Wilms' tumor cancer stem cells correlate with disease progression and poor clinical outcome: A pilot study. Pathology, Research and Practice, 215(8), 152491. https://doi.org/10.1016/j.prp.2019.152491.
Cao, H., Chu, X., Wang, Z., Guo, C., Shao, S., Xiao, J., Zheng, J., & Zhang, D. (2019). High FOXK1 expression correlates with poor outcomes in hepatocellular carcinoma and regulates stemness of hepatocellular carcinoma cells. Life Sciences, 228, 128–134. https://doi.org/10.1016/j.lfs.2019.04.068.
Upadhyaya, B., Liu, Y., & Dey, M. (2019). Phenethyl isothiocyanate exposure promotes oxidative stress and suppresses Sp1 transcription factor in cancer stem cells. International Journal of Molecular Sciences, 20(5). https://doi.org/10.3390/ijms20051027.
Rodman, S. N., Spence, J. M., Ronnfeldt, T. J., Zhu, Y., Solst, S. R., O'Neill, R. A., Allen, B. G., Guan, X., Spitz, D. R., & Fath, M. A. (2016). Enhancement of radiation response in breast cancer stem cells by inhibition of thioredoxin- and glutathione-dependent metabolism. Radiation Research, 186(4), 385–395. https://doi.org/10.1667/RR14463.1.
Li, W., Ma, H., Zhang, J., Zhu, L., Wang, C., & Yang, Y. (2017). Unraveling the roles of CD44/CD24 and ALDH1 as cancer stem cell markers in tumorigenesis and metastasis. Scientific Reports, 7(1), 13856. https://doi.org/10.1038/s41598-017-14364-2.
Sakunrangsit, N., & Ketchart, W. (2019). Plumbagin inhibits cancer stem-like cells, angiogenesis and suppresses cell proliferation and invasion by targeting Wnt/beta-catenin pathway in endocrine resistant breast cancer. Pharmacological Research, 150, 104517. https://doi.org/10.1016/j.phrs.2019.104517.
Zhang, H., Chang, W. J., Li, X. Y., Zhang, N., Kong, J. J., & Wang, Y. F. (2014). Liver cancer stem cells are selectively enriched by low-dose cisplatin. Brazilian Journal of Medical and Biological Research, 47(6), 478–482. https://doi.org/10.1590/1414-431x20143415.
Tan, S., Yamashita, A., Gao, S. J., & Kurisawa, M. (2019). Hyaluronic acid hydrogels with defined crosslink density for the efficient enrichment of breast cancer stem cells. Acta Biomaterialia, 94, 320–329. https://doi.org/10.1016/j.actbio.2019.05.040.
Kong, Y., Lyu, N., Wu, J., Tang, H., Xie, X., Yang, L., Li, X., Wei, W., & Xie, X. (2018). Breast cancer stem cell markers CD44 and ALDH1A1 in serum: distribution and prognostic value in patients with primary breast cancer. Journal of Cancer, 9(20), 3728–3735. https://doi.org/10.7150/jca.28032.
Ma, S., Chan, K. W., Lee, T. K., Tang, K. H., Wo, J. Y., Zheng, B. J., & Guan, X. Y. (2008). Aldehyde dehydrogenase discriminates the CD133 liver cancer stem cell populations. Molecular Cancer Research, 6(7), 1146–1153. https://doi.org/10.1158/1541-7786.MCR-08-0035.
Codony-Servat, J., Codony-Servat, C., Cardona, A. F., Gimenez-Capitan, A., Drozdowskyj, A., Berenguer, J., Bracht, J. W. P., Ito, M., Karachaliou, N., & Rosell, R. (2019). Cancer stem cell biomarkers in EGFR-mutation-positive non-small-cell lung cancer. Clinical Lung Cancer, 20(3), 167–177. https://doi.org/10.1016/j.cllc.2019.02.005.
Moreb, J. S., Ucar, D., Han, S., Amory, J. K., Goldstein, A. S., Ostmark, B., & Chang, L. J. (2012). The enzymatic activity of human aldehyde dehydrogenases 1A2 and 2 (ALDH1A2 and ALDH2) is detected by Aldefluor, inhibited by diethylaminobenzaldehyde and has significant effects on cell proliferation and drug resistance. Chemico-Biological Interactions, 195(1), 52–60. https://doi.org/10.1016/j.cbi.2011.10.007.
Meital, L. T., Coward, A. S., Windsor, M. T., Bailey, T. G., Kuballa, A., & Russell, F. D. (2019). A simple and effective method for the isolation and culture of human monocytes from small volumes of peripheral blood. Journal of Immunological Methods, 472, 75–78. https://doi.org/10.1016/j.jim.2019.04.005.
Di, G., Li, Y., Zhao, X., Wang, N., Fu, J., Li, M., Huang, M., You, W., Kong, X., & Ke, C. (2019). Differential proteomic profiles and characterizations between hyalinocytes and granulocytes in ivory shell Babylonia areolata. Fish & Shellfish Immunology, 92, 405–420. https://doi.org/10.1016/j.fsi.2019.06.036.
Karim, M. R., & Wang, Y. F. (2019). Phenotypic identification of CD19(+)CD5(+)CD1d(+) regulatory B cells that produce interleukin 10 and transforming growth factor beta1 in human peripheral blood. Archives of Medical Science, 15(5), 1176–1183. https://doi.org/10.5114/aoms.2018.77772.
Yang, X., Zeng, Q., Goktas, E., Gopal, K., Al-Aswad, L., Blumberg, D. M., Cioffi, G. A., Liebmann, J. M., & Tezel, G. (2019). T-Lymphocyte subset distribution and activity in patients with glaucoma. Investigative Ophthalmology & Visual Science, 60(4), 877–888. https://doi.org/10.1167/iovs.18-26129.
Emad, A., & Drouin, R. (2014). Evaluation of the impact of density gradient centrifugation on fetal cell loss during enrichment from maternal peripheral blood. Prenatal Diagnosis, 34(9), 878–885. https://doi.org/10.1002/pd.4387.
Liu, W. H., Wang, X., You, N., Tao, K. S., Wang, T., Tang, L. J., & Dou, K. F. (2012). Efficient enrichment of hepatic cancer stem-like cells from a primary rat HCC model via a density gradient centrifugation-centered method. PLoS ONE, 7(4), e35720. https://doi.org/10.1371/journal.pone.0035720.
Smith, L. M., Nesterova, A., Ryan, M. C., Duniho, S., Jonas, M., Anderson, M., Zabinski, R. F., Sutherland, M. K., Gerber, H. P., Van Orden, K. L., Moore, P. A., Ruben, S. M., & Carter, P. J. (2008). CD133/prominin-1 is a potential therapeutic target for antibody-drug conjugates in hepatocellular and gastric cancers. British Journal of Cancer, 99(1), 100–109. https://doi.org/10.1038/sj.bjc.6604437.
Singh, R., Setiady, Y. Y., Ponte, J., Kovtun, Y. V., Lai, K. C., Hong, E. E., Fishkin, N., Dong, L., Jones, G. E., Coccia, J. A., Lanieri, L., Veale, K., Costoplus, J. A., Skaletskaya, A., Gabriel, R., Salomon, P., Wu, R., Qiu, Q., Erickson, H. K., Lambert, J. M., Chari, R. V., & Widdison, W. C. (2016). A new triglycyl peptide linker for antibody-drug conjugates (ADCs) with improved targeted killing of cancer cells. Molecular Cancer Therapeutics, 15(6), 1311–1320. https://doi.org/10.1158/1535-7163.MCT-16-0021.
Toshiyama, R., Konno, M., Eguchi, H., Takemoto, H., Noda, T., Asai, A., Koseki, J., Haraguchi, N., Ueda, Y., Matsushita, K., Asukai, K., Ohashi, T., Iwagami, Y., Yamada, D., Sakai, D., Asaoka, T., Kudo, T., Kawamoto, K., Gotoh, K., Kobayashi, S., Satoh, T., Doki, Y., Nishiyama, N., Mori, M., & Ishii, H. (2019). Poly(ethylene glycol)-poly(lysine) block copolymer-ubenimex conjugate targets aminopeptidase N and exerts an antitumor effect in hepatocellular carcinoma stem cells. Oncogene, 38(2), 244–260. https://doi.org/10.1038/s41388-018-0406-x.
Jiang, Y., Li, X., Hou, J., Huang, Y., Wang, X., Jia, Y., Wang, Q., Xu, W., Zhang, J., & Zhang, Y. (2018). Synthesis and biological characterization of ubenimex-fluorouracil conjugates for anti-cancer therapy. European Journal of Medicinal Chemistry, 143, 334–347. https://doi.org/10.1016/j.ejmech.2017.11.074.
Guo, Q., Jing, F. J., Qu, H. J., Xu, W., Han, B., Xing, X. M., Ji, H. Y., & Jing, F. B. (2019). Ubenimex reverses MDR in gastric cancer Cells by activating Caspase-3-Mediated apoptosis and suppressing the expression of membrane transport proteins. BioMed Research International, 2019, 4390839. https://doi.org/10.1155/2019/4390839.
Jiang, Y., Li, X., Hou, J., Huang, Y., Jia, Y., Zou, M., Zhang, J., Wang, X., Xu, W., & Zhang, Y. (2016). Discovery of BC-01, a novel mutual prodrug (hybrid drug) of ubenimex and fluorouracil as anticancer agent. European Journal of Medicinal Chemistry, 121, 649–657. https://doi.org/10.1016/j.ejmech.2016.05.068.
Jiang, Y., Hou, J., Li, X., Huang, Y., Wang, X., Wu, J., Zhang, J., Xu, W., & Zhang, Y. (2016). Discovery of a novel chimeric ubenimex-gemcitabine with potent oral antitumor activity. Bioorganic & Medicinal Chemistry, 24(22), 5787–5795. https://doi.org/10.1016/j.bmc.2016.09.033.
Martin-Padura, I., Marighetti, P., Agliano, A., Colombo, F., Larzabal, L., Redrado, M., Bleau, A. M., Prior, C., Bertolini, F., & Calvo, A. (2012). Residual dormant cancer stem-cell foci are responsible for tumor relapse after antiangiogenic metronomic therapy in hepatocellular carcinoma xenografts. Laboratory Investigation, 92(7), 952–966. https://doi.org/10.1038/labinvest.2012.65.
Kim, B. H., Park, J. W., Kim, J. S., Lee, S. K., & Hong, E. K. (2019). Stem cell markers predict the response to sorafenib in patients with hepatocellular carcinoma. Gut Liver, 13(3), 342–348. https://doi.org/10.5009/gnl18345.
Yoshida, M., Yamashita, T., Okada, H., Oishi, N., Nio, K., Hayashi, T., Nomura, Y., Hayashi, T., Asahina, Y., Ohwada, M., Sunagozaka, H., Takatori, H., Colombo, F., Porretti, L., Honda, M., & Kaneko, S. (2017). Sorafenib suppresses extrahepatic metastasis de novo in hepatocellular carcinoma through inhibition of mesenchymal cancer stem cells characterized by the expression of CD90. Scientific Reports, 7(1), 11292. https://doi.org/10.1038/s41598-017-11848-z.
Badar, T., & Shah, N. N. (2020). Chimeric antigen receptor T cell therapy for acute lymphoblastic leukemia. Current Treatment Options in Oncology, 21(2), 16. https://doi.org/10.1007/s11864-020-0706-6.
Jin, X., Cao, Y., Wang, L., Sun, R., Cheng, L., He, X., Xiao, X., Jiang, Y., Li, Q., Zhang, H., Lu, W., Lyu, C., Jiang, Y., Meng, J., & Zhao, M. (2019). HLA-matched and HLA-haploidentical allogeneic CD19-directed chimeric antigen receptor T-cell infusions are feasible in relapsed or refractory B-cell acute lymphoblastic leukemia before hematopoietic stem cell transplantation. Leukemia. https://doi.org/10.1038/s41375-019-0610-x.
Huang, H., Wu, H. W., & Hu, Y. X. (2020). Current advances in chimeric antigen receptor T-cell therapy for refractory/relapsed multiple myeloma. Journal of Zhejiang University. Science. B, 21(1), 29–41. https://doi.org/10.1631/jzus.B1900351.
Lin, J. K., Muffly, L. S., Spinner, M. A., Barnes, J. I., Owens, D. K., & Goldhaber-Fiebert, J. D. (2019). Cost effectiveness of chimeric antigen receptor T-Cell therapy in multiply relapsed or refractory adult large B-Cell lymphoma. Journal of Clinical Oncology, 37(24), 2105–2119. https://doi.org/10.1200/JCO.18.02079.
Ahamadi-Fesharaki, R., Fateh, A., Vaziri, F., Solgi, G., Siadat, S. D., Mahboudi, F., & Rahimi-Jamnani, F. (2019). Single-chain variable fragment-based bispecific antibodies: hitting two targets with one sophisticated arrow. Molecular Therapy - Oncolytics, 14, 38–56. https://doi.org/10.1016/j.omto.2019.02.004.
Knodler, M., Korfer, J., Kunzmann, V., Trojan, J., Daum, S., Schenk, M., Kullmann, F., Schroll, S., Behringer, D., Stahl, M., Al-Batran, S. E., Hacker, U., Ibach, S., Lindhofer, H., & Lordick, F. (2018). Randomised phase II trial to investigate catumaxomab (anti-EpCAM x anti-CD3) for treatment of peritoneal carcinomatosis in patients with gastric cancer. British Journal of Cancer, 119(3), 296–302. https://doi.org/10.1038/s41416-018-0150-6.
Kurbacher, C. M., Horn, O., Kurbacher, J. A., Herz, S., Kurbacher, A. T., Hildenbrand, R., & Bollmann, R. (2015). Outpatient intraperitoneal catumaxomab therapy for malignant ascites related to advanced gynecologic neoplasms. Oncologist, 20(11), 1333–1341. https://doi.org/10.1634/theoncologist.2015-0076.
Borlak, J., Langer, F., Spanel, R., Schondorfer, G., & Dittrich, C. (2016). Immune-mediated liver injury of the cancer therapeutic antibody catumaxomab targeting EpCAM, CD3 and Fcgamma receptors. Oncotarget, 7(19), 28059–28074. https://doi.org/10.18632/oncotarget.8574.
Pinato, D. J., Guerra, N., Fessas, P., Murphy, R., Mineo, T., Mauri, F. A., Mukherjee, S. K., Thursz, M., Wong, C. N., Sharma, R., & Rimassa, L. (2020). Immune-based therapies for hepatocellular carcinoma. Oncogene, 39(18), 3620–3637. https://doi.org/10.1038/s41388-020-1249-9.
Turton, K. L., Meier-Stephenson, V., Badmalia, M. D., Coffin, C. S., & Patel, T. R. (2020). Host transcription factors in hepatitis B virus RNA synthesis. Viruses, 12(2). https://doi.org/10.3390/v12020160.
Yip, T. C., Wong, G. L., Wong, V. W., Tse, Y. K., Liang, L. Y., Hui, V. W., Lee, H. W., Lui, G. C., & Chan, H. L. (2019). Reassessing the accuracy of PAGE-B-related scores to predict hepatocellular carcinoma development in patients with chronic hepatitis B. Journal of Hepatology. https://doi.org/10.1016/j.jhep.2019.12.005.
Sartorius, K., Makarova, J., Sartorius, B., An, P., Winkler, C., Chuturgoon, A., & Kramvis, A. (2019). The regulatory role of MicroRNA in Hepatitis-B virus-associated hepatocellular carcinoma (HBV-HCC) pathogenesis. Cells, 8(12). https://doi.org/10.3390/cells8121504.
Liu, Y. C., Lu, L. F., Li, C. J., Sun, N. K., Guo, J. Y., Huang, Y. H., Yeh, C. T., & Chao, C. C. (2019). Hepatitis B virus X protein induces RHAMM-dependent motility in hepatocellular carcinoma cells via PI3K-Akt-Oct-1 signaling. Molecular Cancer Research. https://doi.org/10.1158/1541-7786.MCR-19-0463.
Jin, Y., Lee, W. Y., Toh, S. T., Tennakoon, C., Toh, H. C., Chow, P. K., Chung, A. Y., Chong, S. S., Ooi, L. L., Sung, W. K., & Lee, C. G. (2019). Comprehensive analysis of transcriptome profiles in hepatocellular carcinoma. Journal of Translational Medicine, 17(1), 273. https://doi.org/10.1186/s12967-019-2025-x.
Xu, Q. G., Yuan, S. X., Tao, Q. F., Yu, J., Cai, J., Yang, Y., Guo, X. G., Lin, K. Y., Ma, J. Z., Dai, D. S., Wang, Z. G., Gu, F. M., Zhao, L. H., Li, L. Q., Liu, J. F., Sun, S. H., Zang, Y. J., Liu, H., Yang, F., & Zhou, W. P. (2019). A novel HBx genotype serves as a preoperative predictor and fails to activate the JAK1/STATs pathway in hepatocellular carcinoma. Journal of Hepatology, 70(5), 904–917. https://doi.org/10.1016/j.jhep.2019.01.007.
Wei, J. Y., Lin, D. N., Wu, Z. B., Zhu, J. Y., Zhao, Z. X., Mei, Y. Y., Lin, C. S., Zhang, J., & Zhang, X. H. (2018). Safety and efficacy of DCV-based DAAs therapy for chronic HCV infection in China. Zhonghua Gan Zang Bing Za Zhi, 26(12), 933–939. https://doi.org/10.3760/cma.j.issn.1007-3418.2018.12.011.
Tsukamoto, H., Mishra, L., & Machida, K. (2014). Alcohol, TLR4-TGF-beta antagonism, and liver cancer. Hepatology International, 8(Suppl 2), 408–412. https://doi.org/10.1007/s12072-013-9489-1.
Levrero, M. (2006). Viral hepatitis and liver cancer: the case of hepatitis C. Oncogene, 25(27), 3834–3847. https://doi.org/10.1038/sj.onc.1209562.
Arzumanyan, A., Friedman, T., Ng, I. O., Clayton, M. M., Lian, Z., & Feitelson, M. A. (2011). Does the hepatitis B antigen HBx promote the appearance of liver cancer stem cells? Cancer Research, 71(10), 3701–3708. https://doi.org/10.1158/0008-5472.CAN-10-3951.
Kwon, Y. C., Sasaki, R., Meyer, K., & Ray, R. (2017). Hepatitis C virus core protein modulates endoglin (CD105) signaling pathway for liver pathogenesis. Journal of Virology, 91(21). https://doi.org/10.1128/JVI.01235-17.
Rozeik, M. S., Hammam, O. A., Ali, A. I., Magdy, M., Khalil, H., Anas, A., Abo El Hassan, A. A., Rahim, A. A., & El-Shabasy, A. I. (2017). Evaluation of CD44 and CD133 as markers of liver cancer stem cells in Egyptian patients with HCV-induced chronic liver diseases versus hepatocellular carcinoma. Electronic Physician, 9(7), 4708–4717. https://doi.org/10.19082/4708.
Castelli, G., Pelosi, E., & Testa, U. (2017). Liver cancer: molecular characterization, clonal evolution and cancer stem cells. Cancers (Basel), 9(9). https://doi.org/10.3390/cancers9090127.
Wang, S., Cai, L., Zhang, F., Shang, X., Xiao, R., & Zhou, H. (2020). Inhibition of EZH2 attenuates sorafenib resistance by targeting NOTCH1 activation-dependent liver cancer stem cells via NOTCH1-related MicroRNAs in Hepatocellular carcinoma. Translational Oncology, 13(3), 100741. https://doi.org/10.1016/j.tranon.2020.01.002.
Wang, L., Li, X., Zhang, W., Yang, Y., Meng, Q., Wang, C., Xin, X., Jiang, X., Song, S., Lu, Y., Pu, H., Gui, X., Li, T., Xu, J., Li, J., Jia, S., & Lu, D. (2020). miR24-2 promotes malignant progression of human liver cancer stem cells by enhancing tyrosine kinase src epigenetically. Molecular Therapy, 28(2), 572–586. https://doi.org/10.1016/j.ymthe.2019.10.015.
Wei, Z., Jia, J., Heng, G., Xu, H., Shan, J., Wang, G., Liu, C., Xia, J., Zhou, H., Wu, M., Yang, Z., Wang, M., Xiong, Z., Huang, H., Liu, L., & Qian, C. (2019). Sirtuin-1/Mitochondrial ribosomal protein S5 axis enhances the metabolic flexibility of liver cancer stem cells. Hepatology, 70(4), 1197–1213. https://doi.org/10.1002/hep.30622.
Zheng, H., Pomyen, Y., Hernandez, M. O., Li, C., Livak, F., Tang, W., Dang, H., Greten, T. F., Davis, J. L., Zhao, Y., Mehta, M., Levin, Y., Shetty, J., Tran, B., Budhu, A., & Wang, X. W. (2018). Single-cell analysis reveals cancer stem cell heterogeneity in hepatocellular carcinoma. Hepatology, 68(1), 127–140. https://doi.org/10.1002/hep.29778.
Zhang, Q., He, Y., Luo, N., Patel, S. J., Han, Y., Gao, R., Modak, M., Carotta, S., Haslinger, C., Kind, D., Peet, G. W., Zhong, G., Lu, S., Zhu, W., Mao, Y., Xiao, M., Bergmann, M., Hu, X., Kerkar, S. P., Vogt, A. B., Pflanz, S., Liu, K., Peng, J., Ren, X., & Zhang, Z. (2019). Landscape and dynamics of single immune cells in hepatocellular carcinoma. Cell, 179(4), 829–845 e820. https://doi.org/10.1016/j.cell.2019.10.003.
Liao, X., Song, L., Zhang, L., Wang, H., Tong, Q., Xu, J., Yang, G., Yang, S., & Zheng, H. (2018). LAMP3 regulates hepatic lipid metabolism through activating PI3K/Akt pathway. Molecular and Cellular Endocrinology, 470, 160–167. https://doi.org/10.1016/j.mce.2017.10.010.
Author information
Authors and Affiliations
Contributions
Author Lu Liu performed the initial literature search and prepared the Figures and Tables. Both authors contributed equally to the writing; JB wrote the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare they have no financial interests.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, L., Borlak, J. Advances in Liver Cancer Stem Cell Isolation and their Characterization. Stem Cell Rev and Rep 17, 1215–1238 (2021). https://doi.org/10.1007/s12015-020-10114-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-020-10114-6