Abstract
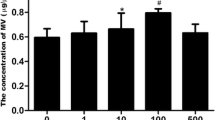
Extracellular vesicles (EVs) shed from kidney mesenchymal stem cells (KMSCs) show protective effects against acute kidney injury and progressive kidney fibrosis via mRNA transfer. Previous studies report improvement of renal anemia following administration of genetically modified MSCs or peritoneal mesothelial cells that secrete erythropoietin (EPO). Here, we determined whether EPO-secreting KMSC-derived EVs (EPO(+)-EVs) can improve renal anemia in mouse models of chronic kidney disease (CKD). The mouse CKD and renal anemia model was induced by electrocoagulation of the right renal cortex and sequential left nephrectomy. At six weeks post-nephrectomy, we observed significantly lower hemoglobin (10.4 ± 0.2 vs. 13.2 ± 0.2 g/dL) and significantly higher blood urea nitrogen and serum creatinine levels in CKD mice relative to controls (60.5 ± 0.5 and 0.37 ± 0.09 mg/dL vs. 19.9 ± 0.5 and 0.12 ± 0.02 mg/dL, respectively). Genetically engineered EPO(+)–KMSCs secreted 71 IU/mL EPO/106 cells/24 h in vitro, and EPO(+)–EVs isolated by differential ultracentrifugation expressed EPO mRNA and horizontally transferred EPO mRNA into target cells in vitro and in vivo. Furthermore, at two weeks post-injection of EPO(+)–KMSCs or EPO(+)-EVs into CKD mice with renal anemia, we observed significant increases in hemoglobin levels (11.7 ± 0.2 and 11.5 ± 0.2 vs. 10.1 ± 0.2 g/dL, respectively) and significantly lower serum creatinine levels at eight weeks in comparison to mice receiving vehicle control (0.30 ± 0.00 and 0.23 ± 0.03 vs. 0.43 ± 0.06 mg/dL, respectively). These results demonstrate that intraperitoneal administration of EPO(+)-EVs significantly increased hemoglobin levels and renal function in CKD mice, suggesting the efficacy of these genetically engineered EVs as a promising novel strategy for the treatment of renal anemia.
Graphical Abstract









Similar content being viewed by others
Data Availability
Not applicable.
Code Availability
Not applicable.
References
KDOQI; National Kidney Foundation (2006). KDOQI clinical practice guidelines and clinical practice recommendations for anemia in chronic kidney disease. American Journal of Kidney Diseases, 47(5 Suppl 3), S11–S145.
Babitt, J. L., & Lin, H. Y. (2012). Mechanisms of anemia in CKD. Journal of the American Society of Nephrology, 23(10), 1631–1634.
Winearls, C. G., Oliver, D. O., Pippard, M. J., Reid, C., Downing, M. R., & Cotes, P. M. (1986). Effect of human erythropoietin derived from recombinant DNA on the anaemia of patients maintained by chronic haemodialysis. Lancet, 2(8517), 1175–1178.
Eschbach, J. W., Egrie, J. C., Downing, M. R., Browne, J. K., & Adamson, J. W. (1987). Correction of the anemia of end-stage renal disease with recombinant human erythropoietin. Results of a combined phase I and II clinical trial. The New England Journal of Medicine, 316(2), 73–78.
Macdougall, I. C. (2001). Present and future strategies in the treatment of renal anaemia. Nephrology, Dialysis, Transplantation, 16(Suppl 5), 50–55.
Eliopoulos, N., Gagnon, R. F., Francois, M., & Galipeau, J. (2006). Erythropoietin delivery by genetically engineered bone marrow stromal cells for correction of anemia in mice with chronic renal failure. Journal of the American Society of Nephrology, 17(6), 1576–1584.
Chiang, C. K., Tanaka, T., Inagi, R., Fujita, T., & Nangaku, M. (2011). Indoxyl sulfate, a representative uremic toxin, suppresses erythropoietin production in a HIF-dependent manner. Laboratory Investigation, 91(11), 1564–1571.
Schorey, J. S., & Bhatnagar, S. (2008). Exosome function: from tumor immunology to pathogen biology. Traffic, 9(6), 871–881.
Camussi, G., Deregibus, M. C., Bruno, S., Cantaluppi, V., & Biancone, L. (2010). Exosomes/microvesicles as a mechanism of cell-to-cell communication. Kidney International, 78(9), 838–848.
Morel, O., Toti, F., Hugel, B., & Freyssinet, J. M. (2004). Cellular microparticles: a disseminated storage pool of bioactive vascular effectors. Current Opinion in Hematology, 11(3), 156–164.
Ratajczak, J., Miekus, K., Kucia, M., et al. (2006). Embryonic stem cell-derived microvesicles reprogram hematopoietic progenitors: evidence for horizontal transfer of mRNA and protein delivery. Leukemia, 20(5), 847–856.
Bruno, S., Grange, C., Deregibus, M. C., et al. (2009). Mesenchymal stem cell-derived microvesicles protect against acute tubular injury. Journal of the American Society of Nephrology, 20(5), 1053–1067.
Gatti, S., Bruno, S., Deregibus, M. C., et al. (2011). Microvesicles derived from human adult mesenchymal stem cells protect against ischaemia-reperfusion-induced acute and chronic kidney injury. Nephrology, Dialysis, Transplantation, 26(5), 1474–1483.
Choi, H. Y., Moon, S. J., Ratliff, B. B., et al. (2014). Microparticles from kidney-derived mesenchymal stem cells act as carriers of proangiogenic signals and contribute to recovery from acute kidney injury. PLoS One, 9(2), e87853.
Choi, H. Y., Lee, H. G., Kim, B. S., et al. (2015). Mesenchymal stem cell-derived microparticles ameliorate peritubular capillary rarefaction via inhibition of endothelial-mesenchymal transition and decrease tubulointerstitial fibrosis in unilateral ureteral obstruction. Current Stem Cell Research & Therapy, 6, 18.
Cantaluppi, V., Gatti, S., Medica, D., et al. (2012). Microvesicles derived from endothelial progenitor cells protect the kidney from ischemia-reperfusion injury by microRNA-dependent reprogramming of resident renal cells. Kidney International, 82(4), 412–427.
Satheesh Madhav, N. V. (2011). Review on microparticulate drug delivery system. International Journal of PharmTech Research, 3(3), 1242–1254.
Plotkin, M. D., & Goligorsky, M. S. (2006). Mesenchymal cells from adult kidney support angiogenesis and differentiate into multiple interstitial cell types including erythropoietin-producing fibroblasts. American Journal of Physiology. Renal Physiology, 291(4), F902–F912.
Skalamera, D., Dahmer, M., Purdon, A. S., et al. (2012). Generation of a genome scale lentiviral vector library for EF1alpha promoter-driven expression of human ORFs and identification of human genes affecting viral titer. PLoS One, 7(12), e51733.
Arnaoutova, I., & Kleinman, H. K. (2010). In vitro angiogenesis: endothelial cell tube formation on gelled basement membrane extract. Nature Protocols, 5(4), 628–635.
Dragovic, R. A., Gardiner, C., Brooks, A. S., et al. (2011). Sizing and phenotyping of cellular vesicles using Nanoparticle Tracking Analysis. Nanomedicine: the Official Journal of the American Academy of Nanomedicine, 7(6), 780–788.
Deregibus, M. C., Cantaluppi, V., Calogero, R., et al. (2007). Endothelial progenitor cell derived microvesicles activate an angiogenic program in endothelial cells by a horizontal transfer of mRNA. Blood, 110(7), 2440–2448.
Baj-Krzyworzeka, M., Szatanek, R., Weglarczyk, K., et al. (2006). Tumour-derived microvesicles carry several surface determinants and mRNA of tumour cells and transfer some of these determinants to monocytes. Cancer Immunology, Immunotherapy, 55(7), 808–818.
Gagnon, R. F., & Gallimore, B. (1988). Characterization of a mouse model of chronic uremia. Urological Research, 16(2), 119–126.
Yamada, K., Miwa, T., Liu, J., Nangaku, M., & Song, W. C. (2004). Critical protection from renal ischemia reperfusion injury by CD55 and CD59. Journal of Immunology, 172(6), 3869–3875.
Kang, D. H., Kim, Y. G., Andoh, T. F., et al. (2001). Post-cyclosporine-mediated hypertension and nephropathy: amelioration by vascular endothelial growth factor. American Journal of Physiology. Renal Physiology, 280(4), F727–F736.
Bot, J., Whitaker, D., Vivian, J., Lake, R., Yao, V., & McCauley, R. (2003). Culturing mouse peritoneal mesothelial cells. Pathology Research and Practice, 199(5), 341–344.
Streja, E., Park, J., Chan, T. Y., et al. (2016). Erythropoietin dose and mortality in hemodialysis patients: marginal structural model to examine causality. International Journal of Nephrology 2016, 6087134.
Naffakh, N., Henri, A., Villeval, J. L., et al. (1995). Sustained delivery of erythropoietin in mice by genetically modified skin fibroblasts. Proceedings of the National Academy of Sciences of the United States of America, 92(8), 3194–3198.
Descamps, V., Blumenfeld, N., Beuzard, Y., & Perricaudet, M. (1996). Keratinocytes as a target for gene therapy. Sustained production of erythropoietin in mice by human keratinocytes transduced with an adenoassociated virus vector. Archives of Dermatology, 132(10), 1207–1211.
Dalle, B., Payen, E., Regulier, E., et al. (1999). Improvement of mouse beta-thalassemia upon erythropoietin delivery by encapsulated myoblasts. Gene Therapy, 6(2), 157–161.
Einbinder, T., Sufaro, Y., Yusim, I., et al. (2003). Correction of anemia in uremic mice by genetically modified peritoneal mesothelial cells. Kidney International, 63(6), 2103–2112.
Noh, H., Yu, M. R., Kim, H. J., et al. (2012). Uremia induces functional incompetence of bone marrow-derived stromal cells. Nephrology, Dialysis, Transplantation, 27(1), 218–225.
Wang, W., Liu, X., Wang, W., et al. (2016). The effects of indoxyl sulfate on human umbilical cord-derived mesenchymal stem cells in vitro. Cellular Physiology and Biochemistry, 38(1), 401–414.
Ratajczak, J., Wysoczynski, M., Hayek, F., Janowska-Wieczorek, A., & Ratajczak, M. Z. (2006). Membrane-derived microvesicles: important and underappreciated mediators of cell-to-cell communication. Leukemia, 20(9), 1487–1495.
Lappin, T. R., Maxwell, A. P., & Johnston, P. G. (2002). EPO’s alter ego: erythropoietin has multiple actions. Stem Cells, 20(6), 485–492.
Osada, S., Ebihara, I., Setoguchi, Y., Takahashi, H., Tomino, Y., & Koide, H. (1999). Gene therapy for renal anemia in mice with polycystic kidney using an adenovirus vector encoding the human erythropoietin gene. Kidney International, 55(4), 1234–1240.
Allan, D., Tieu, A., Lalu, M., & Burger, D. (2020). Mesenchymal stromal cell-derived extracellular vesicles for regenerative therapy and immune modulation: Progress and challenges toward clinical application. Stem Cells Translational Medicine, 9(1), 39–46.
Wang, Y., Lu, X., He, J., & Zhao, W. (2015). Influence of erythropoietin on microvesicles derived from mesenchymal stem cells protecting renal function of chronic kidney disease. Stem Cell Research & Therapy, 6, 100.
Funding
This study was supported by a faculty research grant from Yonsei University College of Medicine (6-2014-0042), a research grant from CHA Bundang Medical Center (2015 − 0301), and the Basic Science Research Program through the National Research Foundation of Korea (2012R1A1A2009345) funded by the Ministry of Education of the Republic of Korea.
Author information
Authors and Affiliations
Contributions
Conceptualization: Hoon Young Choi and Hyeong Cheon Park; Methodology: Hoon Young Choi, Hyeong Cheon Park, Tae Yeon Kim, Mirae Lee, Soo Hyun Kim, and Jong Hyun Jhee; Formal analysis and investigation: Hoon Young Choi, Tae Yeon Kim, Mirae Lee, Soo Hyun Kim, and Hyung Jong Kim; Writing - original draft preparation: Hoon Young Choi and Hyeong Cheon Park; Writing - review and editing: Hoon Young Choi, Yong Kyu Lee, Hyung Jong Kim, and Hyeong Cheon Park; Funding acquisition: Yong Kyu Lee, Hyung Jong Kim, and Hyeong Cheon Park; Supervision: Hyung Jong Kim, Jong Hyun Jhee ,and Hyeong Cheon Park.
All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interests.
Ethics Approval
The animal study protocol was performed in accordance with guidelines for laboratory animals and approved by the Institutional Animal Care and Use Committee, Department of Laboratory Animal Medicine, Medical Research Center, Yonsei University College of Medicine (2010-0226-1).
Consent for Publication
Not applicable.
Consent to Participate
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the Topical Collection: Special Issue on Exosomes and Microvesicles: from Stem Cell Biology to Translation in Human Diseases
Guest Editor: Giovanni Camussi
Supplementary Information
Supplemental Figure S1
Immunofluorescence staining of cytokeratin in mouse peritoneal mesothelial cells (PMCs). Immunofluorescence microscopy showing cytokeratin-labeled (red) mouse PMCs. DAPI, 4’,6-diamidino-2-phenylindole. (PNG 315 kb)
Supplemental Figure S2
Anemia and renal function in normal mice and mouse models of chronic kidney disease (CKD). (A) Hemoglobin levels and (B) blood urea nitrogen levels (BUN) and serum creatinine (Cr) levels in normal and CKD mice. *P < 0.05 vs. vehicle control, Kruskal–Wallis test. (PNG 60 kb)
Supplemental Figure S3
Masson’s trichrome staining of tissue from mouse models of chronic kidney disease (CKD). (A) Extensive fibrotic lesions were present in the cortex and corticomedullary junction of kidney sections from CKD mice after 6 and 9 weeks. (B) Semiquantitative injury scoring of the cortex and corticomedullary junction of kidney sections from CKD mice after 6 and 9 weeks. (PNG 2399 kb)
Supplement Figure S4
Erythropoietin (EPO)(+)–kidney-derived mesenchymal stem cell (KMSC)-derived extracellular vesicles (EPO(+)-EVs) mediate horizontal EPO mRNA transfer into human tubular cells (HK-2) and human podocytes in vitro. (A) Immunofluorescence microscopy showing red CellTracker™ -labeled EVs in human tubular cells (HK-2) and human podocytes. (B) EPO mRNA levels in HK-2 and human podocytes treated in vitro with EPO(+)-EVs. EPO(−)-EVs were used as negative controls.(PNG 413 kb)
Rights and permissions
About this article
Cite this article
Choi, H.Y., Kim, T.Y., Lee, M. et al. Kidney Mesenchymal Stem Cell‐derived Extracellular Vesicles Engineered to Express Erythropoietin Improve Renal Anemia in Mice with Chronic Kidney Disease. Stem Cell Rev and Rep 18, 980–992 (2022). https://doi.org/10.1007/s12015-021-10141-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-021-10141-x