Abstract
In Pompe disease, deficient lysosomal acid α-glucosidase (GAA) activity causes glycogen accumulation in the muscles, which leads to weakness, cardiomyopathy, and respiratory failure. Although glycogen accumulation also occurs in the nervous system, the burden of neurological deficits in Pompe disease remains obscure. In this study, a neuron-specific gene therapy was administered to Pompe mice through intracerebroventricular injection of a viral vector carrying a neuron-specific promoter. The results revealed that gene therapy increased GAA activity and decreased glycogen content in the brain and spinal cord but not in the muscles of Pompe mice. Gene therapy only slightly increased the muscle strength of Pompe mice but substantially improved their performance on the rotarod, a test measuring motor coordination. Gene therapy also decreased astrogliosis and increased myelination in the brain and spinal cord of Pompe mice. Therefore, a neuron-specific treatment improved the motor coordination of Pompe mice by lowering glycogen accumulation, decreasing astrogliosis, and increasing myelination. These findings indicate that neurological deficits are responsible for a significant burden in Pompe disease.







Similar content being viewed by others
References
Hirschhorn R, Reuser A (2001) Glycogen storage disease type II: acid alpha-glucosidase (acid maltase) deficiency. In: Scriver C, Beaudet A, Sly W, Valle D (eds) The metabolic and molecular bases of inherited disease, vol III, 8th edn. McGraw-Hill, New York, pp. 3389–3420
Van den Hout H, Reuser AJ, Vulto AG, Loonen MC, Cromme-Dijkhuis A, Van der Ploeg AT (2000) Recombinant human alpha-glucosidase from rabbit milk in Pompe patients. Lancet 356(9227):397–398
Amalfitano A, McVie-Wylie AJ, Hu H, Dawson TL, Raben N, Plotz P, Chen YT (1999) Systemic correction of the muscle disorder glycogen storage disease type II after hepatic targeting of a modified adenovirus vector encoding human acid-alpha-glucosidase. Proc Natl Acad Sci U S A 96(16):8861–8866
Kishnani P, Corzo D, Nicolino M, Byrne B, Mandel H, Hwu WL, Leslie N, Levine J et al (2007) Recombinant human acid {alpha}-glucosidase. Major clinical benefits in infantile-onset Pompe disease. Neurology 68(2):99–109
Kishnani PS, Corzo D, Leslie ND, Gruskin D, Van der Ploeg A, Clancy JP, Parini R, Morin G et al (2009) Early treatment with alglucosidase alpha prolongs long-term survival of infants with Pompe disease. Pediatr Res 66(3):329–335
Van den Hout JM, Kamphoven JH, Winkel LP, Arts WF, De Klerk JB, Loonen MC, Vulto AG, Cromme-Dijkhuis A et al (2004) Long-term intravenous treatment of Pompe disease with recombinant human alpha-glucosidase from milk. Pediatrics 113(5):e448–e457
Nicolino M, Byrne B, Wraith JE, Leslie N, Mandel H, Freyer DR, Arnold GL, Pivnick EK et al (2009) Clinical outcomes after long-term treatment with alglucosidase alfa in infants and children with advanced Pompe disease. Genet Med 11(3):210–219
Chien YH, Chiang SC, Zhang XK, Keutzer J, Lee NC, Huang AC, Chen CA, Wu MH et al (2008) Early detection of Pompe disease by newborn screening is feasible: results from the Taiwan screening program. Pediatrics 122(1):e39–e45
Chien YH, Lee NC, Thurberg BL, Chiang SC, Zhang XK, Keutzer J, Huang AC, Wu MH et al (2009) Pompe disease in infants: improving the prognosis by newborn screening and early treatment. Pediatrics 124(6):e1116–e1125
Chien YH, Lee NC, Chen CA, Tsai FJ, Tsai WH, Shieh JY, Huang HJ, Hsu WC, Tsai TH, Hwu WL (2015) Long-term prognosis of patients with infantile-onset Pompe disease diagnosed by newborn screening and treated since birth. J Pediatr 166 (4):985-991 e981-982. doi:10.1016/j.jpeds.2014.10.068
van Gelder CM, van Capelle CI, Ebbink BJ, Moor-van Nugteren I, van den Hout JM, Hakkesteegt MM, van Doorn PA, de Coo IF et al (2012) Facial-muscle weakness, speech disorders and dysphagia are common in patients with classic infantile Pompe disease treated with enzyme therapy. J Inherit Metab Dis 35(3):505–511
Peng SS, Hwu WL, Lee NC, Tsai FJ, Tsai WH, Chien YH (2016) Slow, progressive myopathy in neonatally treated patients with infantile-onset Pompe disease: a muscle magnetic resonance imaging study. Orphanet J Rare Dis 11(1):63
Ebbink BJ, Poelman E, Plug I, Lequin MH, van Doorn PA, Aarsen FK, van der Ploeg AT, van den Hout JM (2016) Cognitive decline in classic infantile Pompe disease: an underacknowledged challenge. Neurology 86(13):1260–1261
DeRuisseau LR, Fuller DD, Qiu K, DeRuisseau KC, Donnelly WH Jr, Mah C, Reier PJ, Byrne BJ (2009) Neural deficits contribute to respiratory insufficiency in Pompe disease. Proc Natl Acad Sci U S A 106(23):9419–9424
Dubrovsky A, Corderi J, Lin M, Kishnani PS, Jones HN (2011) Expanding the phenotype of late-onset Pompe disease: tongue weakness: a new clinical observation. Muscle Nerve 44(6):897–901
Raben N, Nagaraju K, Lee E, Kessler P, Byrne B, Lee L, LaMarca M, King C et al (1998) Targeted disruption of the acid alpha-glucosidase gene in mice causes an illness with critical features of both infantile and adult human glycogen storage disease type II. J Biol Chem 273(30):19086–19092
Sidman RL, Taksir T, Fidler J, Zhao M, Dodge JC, Passini MA, Raben N, Thurberg BL et al (2008) Temporal neuropathologic and behavioral phenotype of 6neo/6neo Pompe disease mice. J Neuropathol Exp Neurol 67(8):803–818
Iida A, Takino N, Miyauchi H, Shimazaki K, Muramatsu S (2013) Systemic delivery of tyrosine-mutant AAV vectors results in robust transduction of neurons in adult mice. Biomed Res Int 2013:974819
Koeberl DD, Luo X, Sun B, McVie-Wylie A, Dai J, Li S, Banugaria SG, Chen YT et al (2011) Enhanced efficacy of enzyme replacement therapy in Pompe disease through mannose-6-phosphate receptor expression in skeletal muscle. Mol Genet Metab 103(2):107–112
Joly MS, Martin RP, Mitra-Kaushik S, Phillips L, D'Angona A, Richards SM, Joseph AM (2014) Transient low-dose methotrexate generates B regulatory cells that mediate antigen-specific tolerance to alglucosidase alfa. J Immunol 193(8):3947–3958
Khanna R, Flanagan JJ, Feng J, Soska R, Frascella M, Pellegrino LJ, Lun Y, Guillen D et al (2012) The pharmacological chaperone AT2220 increases recombinant human acid alpha-glucosidase uptake and glycogen reduction in a mouse model of Pompe disease. PLoS One 7(7):e40776
Raben N, Nagaraju K, Lee E, Plotz P (2000) Modulation of disease severity in mice with targeted disruption of the acid alpha-glucosidase gene. Neuromuscul Disord 10(4–5):283–291
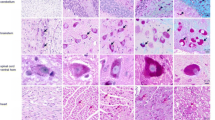
Taksir TV, Griffiths D, Johnson J, Ryan S, Shihabuddin LS, Thurberg BL (2007) Optimized preservation of CNS morphology for the identification of glycogen in the Pompe mouse model. J Histochem Cytochem 55(10):991–998
Kikuchi T, Yang HW, Pennybacker M, Ichihara N, Mizutani M, Van Hove JL, Chen YT (1998) Clinical and metabolic correction of pompe disease by enzyme therapy in acid maltase-deficient quail. J Clin Invest 101(4):827–833
Falk DJ, Todd AG, Lee S, Soustek MS, ElMallah MK, Fuller DD, Notterpek L, Byrne BJ (2015) Peripheral nerve and neuromuscular junction pathology in Pompe disease. Hum Mol Genet 24(3):625–636
Wahl SE, McLane LE, Bercury KK, Macklin WB, Wood TL (2014) Mammalian target of rapamycin promotes oligodendrocyte differentiation, initiation and extent of CNS myelination. J Neurosci 34(13):4453–4465
Rozas G, Guerra MJ, Labandeira-Garcia JL (1997) An automated rotarod method for quantitative drug-free evaluation of overall motor deficits in rat models of parkinsonism. Brain Res Brain Res Protoc 2(1):75–84
Lee NC, Shieh YD, Chien YH, Tzen KY, Yu IS, Chen PW, Hu MH, Hu MK et al (2013) Regulation of the dopaminergic system in a murine model of aromatic L-amino acid decarboxylase deficiency. Neurobiol Dis 52:177–190
Deacon RM (2013) Measuring the strength of mice. J Vis Exp (76)
ElMallah MK, Falk DJ, Lane MA, Conlon TJ, Lee KZ, Shafi NI, Reier PJ, Byrne BJ et al (2012) Retrograde gene delivery to hypoglossal motoneurons using adeno-associated virus serotype 9. Hum Gene Ther Methods 23(2):148–156
Lee KZ, Qiu K, Sandhu MS, Elmallah MK, Falk DJ, Lane MA, Reier PJ, Byrne BJ et al (2011) Hypoglossal neuropathology and respiratory activity in pompe mice. Front Physiol 2:31
Augustine EF, Mink JW (2013) Enzyme replacement in neuronal storage disorders in the pediatric population. Curr Treat Options Neurol 15(5):634–651
Deacon RM (2013) Measuring motor coordination in mice. J Vis Exp (75):e2609
Dunham NW, Miya TS (1957) A note on a simple apparatus for detecting neurological deficit in rats and mice. J Am Pharm Assoc Am Pharm Assoc 46(3):208–209
McKenzie IA, Ohayon D, Li H, de Faria JP, Emery B, Tohyama K, Richardson WD (2014) Motor skill learning requires active central myelination. Science 346(6207):318–322
Martin JJ, de Barsy T, van Hoof F, Palladini G (1973) Pompe’s disease: an inborn lysosomal disorder with storage of glycogen. A study of brain and striated muscle. Acta Neuropathol 23(3):229–244
Burda JE, Bernstein AM, Sofroniew MV (2016) Astrocyte roles in traumatic brain injury. Exp Neurol 275(Pt 3):305–315
Bosch ME, Aldrich A, Fallet R, Odvody J, Burkovetskaya M, Schuberth K, Fitzgerald JA, Foust KD et al (2016) Self-complementary AAV9 gene delivery partially corrects pathology associated with juvenile neuronal ceroid Lipofuscinosis (CLN3). J Neurosci 36(37):9669–9682
Acknowledgments
This work was funded by a grant from the Ministry of Science and Technology (103-2314-B-002-057-MY3) of Taiwan. The authors would like to thank the scientists from the Taiwan Mouse Clinic and the National Taiwan University Disease Animal Research Center, both of which are funded by the National Research Program for Biopharmaceuticals (NRPB), and doctor Kun-Ze Lee for the setting up of respiratory study. We thank Mika Ito and Naomi Takino (Jichi Medical University, Japan) for their help with the production of the AAV vectors.
Author information
Authors and Affiliations
Contributions
N.L, W.H., and Y.C. designed and conducted the study and performed statistical analysis. S.M. provided the AAVN vector. D.F., B.B., and L.T. supervised the immunohistochemistry and respiratory study. C.C, N.S., and K.C. performed the immunohistochemistry, functional study, and molecular studies. All authors participated in the manuscript preparation and approved the final version for submission.
Corresponding author
Ethics declarations
The authors have disclosed the potential conflicts of interest. The experimental procedures were approved and performed in accordance with the guidelines of the National Taiwan University College of Medicine and the College of Public Health Institutional Animal Care and Use Committee (IACUC No. 20120334). There is no human samples in this study and no inform consent is needed.
Conflict of Interest
S. M. owns equity in a gene therapy company (Gene Therapy Research Institution) that commercializes the use of AAV vectors for gene therapy applications. To the extent that the work in this manuscript increases the value of these commercial holdings, S. M. has a conflict of interest. No competing financial interests exist for other authors.
Electronic Supplementary Material
Supplementary Fig. 1
(a) Distribution of vg. Real-time PCR analysis of vg copy number in the brain, spinal cord, liver, and quadriceps of the untreated (Pompe; red) and gene therapy-treated (Pompe-GT; blue) Pompe mice. The detection limit was 10 copies/μg DNA. * indicates p < 0.05. (b) Anti-GAA titers at the end of the study in the untreated, ERT-treated and gene therapy-treated Pompe mice. ERT, but not gene therapy, triggered a strong antibody response. * indicates p < 0.05. (JPEG 237 kb)
Supplementary Fig. 2
Biodistribution of the injected virus. AAVN-GFP was injected in the same way as AAVN-GAA, and coronal sections were stained with anti-GFP. Images are at ×100 or ×400 magnification. Positive staining was observed in the neurons in the cortex (arrow; a and d) and Purkinje cells and other cell types in the cerebellum (arrow; b and e) but not in the striatum (c and f) or the anterior horn motor neurons in the cervical spinal cord (h and k). The light staining in the anterior horn motor neurons is likely background. Many fibers in the posterior horn stained positive (i and l). The window in panel L demonstrates a high magnification picture of the dot-like positive staining nerve fibers. (JPEG 1146 kb)
Supplementary Fig. 3
Immunohistochemical staining of neuromuscular junctions in the diaphragm muscle. (a-d) Alexa Fluor 594-conjugated α-bungarotoxin staining of end plates of control mice (a) and untreated (Pompe; b), ERT-treated (Pompe-ERT; c), and gene therapy-treated (Pompe-GT; d) Pompe mice. End plates in the untreated Pompe mice were enlarged and fragmented (arrow), but neither ERT or gene therapy significantly improved the morphology of end plates. (e-h) α-bungarotoxin (red) and neurofilament plus ZNP-1 (green) triple staining in the untreated Pompe mice. (e) α-bungarotoxin staining. (f) Neurofilament plus ZNP-1 staining. (g) A merged view. (h) A high magnification picture of an end plate after triple staining. There was no significant abnormality in the neurofilaments plus ZNP-1. All images are at ×200 magnification except for panel h (×400). (JPEG 450 kb)
Rights and permissions
About this article
Cite this article
Lee, NC., Hwu, WL., Muramatsu, SI. et al. A Neuron-Specific Gene Therapy Relieves Motor Deficits in Pompe Disease Mice. Mol Neurobiol 55, 5299–5309 (2018). https://doi.org/10.1007/s12035-017-0763-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-017-0763-4