Abstract
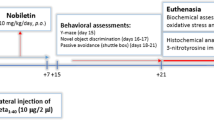
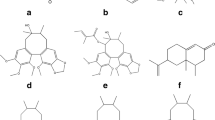
Alzheimer’s disease (AD) is a devastating neurodegenerative disorder in which superior brain functions, such as memory and cognition, are impaired. Currently, no effective treatment is available for AD. Although andrographolide (ANDRO), a compound extracted from the herb Andrographis paniculata, has shown interesting effects in models of several diseases, including AD, its effects on other molecular changes observed in AD, such as neuroinflammation and oxidative stress, have not yet been studied. To evaluate the impact of ANDRO-based intervention on the levels of amyloid-β (Aβ) and neuroinflammatory and oxidative stress markers in the brains of aged Octodon degus, a Chilean rodent, fifty-six-month-old O. degus were treated intraperitoneally with 2 or 4 mg/kg ANDRO. Vehicle-injected and 12-month-old O. degus were used as positive controls. Then, the protein levels of selected markers were assessed via immunohistochemistry and immunoblotting. ANDRO significantly reduced the total Aβ burden as well as astrogliosis and interleukin-6 levels. Moreover, ANDRO significantly reduced the levels of 4-hydroxynonenal and N-tyrosine adducts, suggesting a relevant reduction in oxidative stress within aged O. degus brain. Considering that O. degus has been proposed as a potential “natural” model for sporadic AD due to the development of neuropathological markers that resemble this pathology, our results suggest that ANDRO should be further studied to establish its potential as a therapeutic drug for AD.







Similar content being viewed by others
References
Colombres M, Sagal JP, Inestrosa NC (2004) An overview of the current and novel drugs for Alzheimer's disease with particular reference to anti-cholinesterase compounds. Curr Pharm Des 10(25):3121–3130
Silvestrelli G, Lanari A, Parnetti L, Tomassoni D, Amenta F (2006) Treatment of Alzheimer's disease: From pharmacology to a better understanding of disease pathophysiology. Mech Ageing Dev 127(2):148–157. https://doi.org/10.1016/j.mad.2005.09.018
Querfurth HW, LaFerla FM (2010) Alzheimer's disease. N Engl J Med 362(4):329–344. https://doi.org/10.1056/NEJMra0909142
Serrano-Pozo A, Frosch M, Masliah E, Hyman B (2011) Neuropathological alterations in Alzheimer disease. Cold Spring Harb Perspect Med 1:a006189
Brosseron F, Krauthausen M, Kummer M, Heneka MT (2014) Body fluid cytokine levels in mild cognitive impairment and Alzheimer's disease: A comparative overview. Mol Neurobiol 50(2):534–544. https://doi.org/10.1007/s12035-014-8657-1
Arrazola MS, Silva-Alvarez C, Inestrosa NC (2015) How the Wnt signaling pathway protects from neurodegeneration: The mitochondrial scenario. Front Cell Neurosci 9:166. https://doi.org/10.3389/fncel.2015.00166
Zhao Y, Zhao B (2013) Oxidative stress and the pathogenesis of Alzheimer's disease. Oxidative Med Cell Longev 2013:316523. https://doi.org/10.1155/2013/316523
Fuentealba RA, Farias G, Scheu J, Bronfman M, Marzolo MP, Inestrosa NC (2004) Signal transduction during amyloid-beta-peptide neurotoxicity: Role in Alzheimer disease. Brain Res Brain Res Rev 47(1–3):275–289. https://doi.org/10.1016/j.brainresrev.2004.07.018
Cerpa W, Dinamarca MC, Inestrosa NC (2008) Structure-function implications in Alzheimer's disease: Effect of Abeta oligomers at central synapses. Curr Alzheimer Res 5(3):233–243
Cacace R, Sleegers K, Van Broeckhoven C (2016) Molecular genetics of early-onset Alzheimer's disease revisited. Alzheimers Dement 12(6):733–748. https://doi.org/10.1016/j.jalz.2016.01.012
Inestrosa NC, Rios JA, Cisternas P, Tapia-Rojas C, Rivera DS, Braidy N, Zolezzi JM, Godoy JA et al (2015) Age progression of neuropathological markers in the brain of the Chilean rodent Octodon degus, a natural model of Alzheimer's disease. Brain Pathol 25(6):679–691. https://doi.org/10.1111/bpa.12226
Ardiles AO, Tapia-Rojas CC, Mandal M, Alexandre F, Kirkwood A, Inestrosa NC, Palacios AG (2012) Postsynaptic dysfunction is associated with spatial and object recognition memory loss in a natural model of Alzheimer's disease. Proc Natl Acad Sci U S A 109(34):13835–13840. https://doi.org/10.1073/pnas.1201209109
Rivera DS, Lindsay CB, Codocedo JF, Morel I, Pinto C, Cisternas P, Bozinovic F, Inestrosa NC (2016) Andrographolide recovers cognitive impairment in a natural model of Alzheimer’s disease (Octodon degus). Neurobiol Aging 46:204–220. https://doi.org/10.1016/j.neurobiolaging.2016.06.0
Cisternas P, Zolezzi JM, Lindsay C, Rivera DS, Martinez A, Bozinovic F, Inestrosa NC (2018) New insights into the spontaneous human Alzheimer's disease-like model Octodon degus: Unraveling amyloid-beta peptide aggregation and age-related amyloid pathology. J Alzheimers Dis 66(3):1145–1163. https://doi.org/10.3233/JAD-180729
Panossian A, Hovhannisyan A, Mamikonyan G, Abrahamian H, Hambardzumyan E, Gabrielian E, Goukasova G, Wikman G et al (2000) Pharmacokinetic and oral bioavailability of andrographolide from Andrographis paniculata fixed combination Kan Jang in rats and human. Phytomedicine 7(5):351–364
Jayakumar T, Hsieh CY, Lee JJ, Sheu JR (2013) Experimental and clinical pharmacology of Andrographis paniculata and its major bioactive Phytoconstituent Andrographolide. Evid Based Complement Alternat Med 2013:846740. https://doi.org/10.1155/2013/846740
Serrano FG, Tapia-Rojas C, Carvajal FJ, Hancke J, Cerpa W, Inestrosa NC (2014) Andrographolide reduces cognitive impairment in young and mature AbetaPPswe/PS-1 mice. Mol Neurodegener 9:61. https://doi.org/10.1186/1750-1326-9-61
Varela-Nallar L, Arredondo SB, Tapia-Rojas C, Hancke J, Inestrosa NC (2015) Andrographolide stimulates neurogenesis in the adult Hippocampus. Neural Plast 2015:935403. https://doi.org/10.1155/2015/935403
Sikes R, Gannon W (2011) Guidelines of the American Society of Mammalogists for the use of wild mammals in research. J Mammal 92:235–253
Toledo EM, Inestrosa NC (2010) Activation of Wnt signaling by lithium and rosiglitazone reduced spatial memory impairment and neurodegeneration in brains of an APPswe/PSEN1DeltaE9 mouse model of Alzheimer's disease. Mol Psychiatry 15(3):272–285. https://doi.org/10.1038/mp.2009.72
Tapia-Rojas C, Inestrosa NC (2018) Loss of canonical Wnt signaling is involved in the pathogenesis of Alzheimer's disease. Neural Regen Res 13(10):1705–1710. https://doi.org/10.4103/1673-5374.238606
Hock BJ Jr, Lamb BT (2001) Transgenic mouse models of Alzheimer's disease. Trends Genet 17(10):S7–S12
Braidy N, Munoz P, Palacios AG, Castellano-Gonzalez G, Inestrosa NC, Chung RS, Sachdev P, Guillemin GJ (2012) Recent rodent models for Alzheimer's disease: Clinical implications and basic research. J Neural Transm 119(2):173–195. https://doi.org/10.1007/s00702-011-0731-5
Inestrosa N, Reyes A, Chacón M, Cerpa W, Villalón A, Montiel J, Merabachvili G, Aldunate R et al (2005) Human-like rodent amyloid-beta-peptide determines Alzheimer pathology in aged wild-type Octodon degu. Neurobiol Aging 26(7):1023–1028
Deacon RM, Altimiras FJ, Bazan-Leon EA, Pyarasani RD, Nachtigall FM, Santos LS, Tsolaki AG, Pednekar L et al (2015) Natural AD-like neuropathology in Octodon degus: Impaired burrowing and Neuroinflammation. Curr Alzheimer Res 12(4):314–322
van Groen T, Kadish I, Popovic N, Popovic M, Caballero-Bleda M, Bano-Otalora B, Vivanco P, Rol MA et al (2011) Age-related brain pathology in Octodon degu: Blood vessel, white matter and Alzheimer-like pathology. Neurobiol Aging 32(9):1651–1661. https://doi.org/10.1016/j.neurobiolaging.2009.10.008
Haass C, Selkoe DJ (2007) Soluble protein oligomers in neurodegeneration: Lessons from the Alzheimer's amyloid beta-peptide. Nat Rev Mol Cell Biol 8(2):101–112. https://doi.org/10.1038/nrm2101
Tapia-Rojas C, Burgos PV, Inestrosa NC (2016) Inhibition of Wnt signaling induces amyloidogenic processing of amyloid precursor protein and the production and aggregation of amyloid-beta (Abeta)42 peptides. J Neurochem 139(6):1175–1191. https://doi.org/10.1111/jnc.13873
Andreasson K, Bachstetter A, Colonna M, Ginhoux HC, Lamb B (2016) Targeting innate immunity for neurodegenerative disorders of the central nervous system. J Neurochem 138(5):653–693. https://doi.org/10.1111/jnc.13667
Hanke ML, Kielian T (2011) Toll-like receptors in health and disease in the brain: Mechanisms and therapeutic potential. Clin Sci (Lond) 121(9):367–387. https://doi.org/10.1042/CS20110164
Landreth G, Reed-Geaghan E (2009) Toll-like receptors in Alzheimer's disease. Curr Top Microbiol Immunol 336:137–153. https://doi.org/10.1007/978-3-642-00549-7_8
Eng LF, Yu AC, Lee YL (1992) Astrocytic response to injury. Prog Brain Res 94:353–365
Zolezzi JM, Inestrosa NC (2017) Wnt/TLR dialog in Neuroinflammation, relevance in Alzheimer's disease. Front Immunol 8:187. https://doi.org/10.3389/fimmu.2017.00187
McDonald CL, Hennessy E, Rubio-Araiz A, Keogh B, McCormack W, McGuirk P, Reilly M, Lynch MA (2016) Inhibiting TLR2 activation attenuates amyloid accumulation and glial activation in a mouse model of Alzheimer's disease. Brain Behav Immun 58:191–200. https://doi.org/10.1016/j.bbi.2016.07.143
Liu S, Liu Y, Hao W, Wolf L, Kiliaan AJ, Penke B, Rube CE, Walter J et al (2012) TLR2 is a primary receptor for Alzheimer's amyloid beta peptide to trigger neuroinflammatory activation. J Immunol 188(3):1098–1107. https://doi.org/10.4049/jimmunol.1101121
Bolin LM, Zhaung A, Strychkarska-Orczyk I, Nelson E, Huang I, Malit M, Nguyen Q (2005) Differential inflammatory activation of IL-6 (−/−) astrocytes. Cytokine 30(2):47–55. https://doi.org/10.1016/j.cyto.2004.11.007
Eng LF, Ghirnikar RS (1994) GFAP and astrogliosis. Brain Pathol 4(3):229–237
Gendelman HE (2002) Neural immunity: Friend or foe? J Neuro-Oncol 8(6):474–479. https://doi.org/10.1080/13550280290168631
Zhou X, Li J, Yang W (2014) Calcium/calmodulin-dependent protein kinase II regulates cyclooxygenase-2 expression and prostaglandin E2 production by activating cAMP-response element-binding protein in rat peritoneal macrophages. Immunology 143(2):287–299. https://doi.org/10.1111/imm.12309
Chang CC, Duann YF, Yen TL, Chen YY, Jayakumar T, Ong ET, Sheu JR (2014) Andrographolide, a novel NF-kappaB inhibitor, inhibits vascular smooth muscle cell proliferation and cerebral endothelial cell inflammation. Acta Cardiol Sin 30(4):308–315
Minghetti L (2005) Role of inflammation in neurodegenerative diseases. Curr Opin Neurol 18(3):315–321
Chiou WF, Lin JJ, Chen CF (1998) Andrographolide suppresses the expression of inducible nitric oxide synthase in macrophage and restores the vasoconstriction in rat aorta treated with lipopolysaccharide. Br J Pharmacol 125(2):327–334. https://doi.org/10.1038/sj.bjp.0702073
Hidalgo MA, Hancke JL, Bertoglio JC, Burgos R (2013) Andrographolide a new potential drug for the long term treatment of rheumatoid arthritis disease. In: Hiroaki M (ed) Innovative Rheumatology First Edn. IntehOpen Limited, London
Shen YC, Chen CF, Chiou WF (2002) Andrographolide prevents oxygen radical production by human neutrophils: Possible mechanism(s) involved in its anti-inflammatory effect. Br J Pharmacol 135(2):399–406. https://doi.org/10.1038/sj.bjp.0704493
Wang X, Ye P, Cao R, Yang X, Xiao W, Zhang Y, Bai Y, Wu H (2014) The association of homocysteine with metabolic syndrome in a community-dwelling population: Homocysteine might be concomitant with metabolic syndrome. PLoS One 9(11):e113148. https://doi.org/10.1371/journal.pone.0113148
Cojocaru IM, Cojocaru M, Miu G, Sapira V (2011) Study of interleukin-6 production in Alzheimer's disease. Rom J Intern Med 49(1):55–58
Wong SY, Tan MG, Banks WA, Wong WS, Wong PT, Lai MK (2016) Andrographolide attenuates LPS-stimulated up-regulation of C-C and C-X-C motif chemokines in rodent cortex and primary astrocytes. J Neuroinflammation 13:34. https://doi.org/10.1186/s12974-016-0498-6
Kaushik DK, Basu A (2013) A friend in need may not be a friend indeed: Role of microglia in neurodegenerative diseases. CNS Neurol Disord Drug Targets 12(6):726–740
Mosher KI, Wyss-Coray T (2014) Microglial dysfunction in brain aging and Alzheimer's disease. Biochem Pharmacol 88(4):594–604. https://doi.org/10.1016/j.bcp.2014.01.008
Rawdin BJ, Mellon SH, Dhabhar FS, Epel ES, Puterman E, Su Y, Burke HM, Reus VI et al (2013) Dysregulated relationship of inflammation and oxidative stress in major depression. Brain Behav Immun 31:143–152. https://doi.org/10.1016/j.bbi.2012.11.011
Miranda S, Opazo C, Larrondo LF, Munoz FJ, Ruiz F, Leighton F, Inestrosa NC (2000) The role of oxidative stress in the toxicity induced by amyloid beta-peptide in Alzheimer's disease. Prog Neurobiol 62(6):633–648
Butterfield DA, Lauderback CM (2002) Lipid peroxidation and protein oxidation in Alzheimer's disease brain: Potential causes and consequences involving amyloid beta-peptide-associated free radical oxidative stress. Free Radic Biol Med 32(11):1050–1060
Lee JE, Han PL (2013) An update of animal models of Alzheimer disease with a reevaluation of plaque depositions. Exp Neurobiol 22(2):84–95. https://doi.org/10.5607/en.2013.22.2.84
Rowe CC, Villemagne VL (2013) Amyloid imaging with PET in early Alzheimer disease diagnosis. Med Clin North Am 97(3):377–398. https://doi.org/10.1016/j.mcna.2012.12.017
Li Z, Xu X, Leng X, He M, Wang J, Cheng S, Wu H (2016) Roles of reactive oxygen species in cell signaling pathways and immune responses to viral infections. Arch Virol 162(3):603–610. https://doi.org/10.1007/s00705-016-3130-2
Gill R, Tsung A, Billiar T (2010) Linking oxidative stress to inflammation: Toll-like receptors. Free Radic Biol Med 48(9):1121–1132. https://doi.org/10.1016/j.freeradbiomed.2010.01.006
Kim D, Lee K, Gabr A, Choi G, Kim J, Ko S, Han H (2016) Aβ-induced Drp1 phosphorylation through Akt activation promotes excessive mitochondrial fission leading to neuronal apoptosis. Biochim Biophys Acta 1863(11):2820–2834. https://doi.org/10.1016/j.bbamcr.2016.09.003
Forloni G, Lucca E, Angeretti N, Della Torre P, Salmona M (1997) Amidation of beta-amyloid peptide strongly reduced the amyloidogenic activity without alteration of the neurotoxicity. J Neurochem 69(5):2048–2054
Butterfield DA, Castegna A, Lauderback CM, Drake J (2002) Evidence that amyloid beta-peptide-induced lipid peroxidation and its sequelae in Alzheimer's disease brain contribute to neuronal death. Neurobiol Aging 23(5):655–664
Butterfield DA, Swomley AM, Sultana R (2013) Amyloid beta-peptide (1-42)-induced oxidative stress in Alzheimer disease: Importance in disease pathogenesis and progression. Antioxid Redox Signal 19(8):823–835. https://doi.org/10.1089/ars.2012.5027
Pratico D (2008) Oxidative stress hypothesis in Alzheimer's disease: A reappraisal. Trends Pharmacol Sci 29(12):609–615. https://doi.org/10.1016/j.tips.2008.09.001
Padurariu M, Ciobica A, Lefter R, Serban IL, Stefanescu C, Chirita R (2013) The oxidative stress hypothesis in Alzheimer's disease. Psychiatr Danub 25(4):401–409
Swomley AM, Forster S, Keeney JT, Triplett J, Zhang Z, Sultana R, Butterfield DA (2014) Abeta, oxidative stress in Alzheimer disease: Evidence based on proteomics studies. Biochim Biophys Acta 1842(8):1248–1257. https://doi.org/10.1016/j.bbadis.2013.09.015
Gemma C, Vila J, Bachstetter A, Bickford PC (2007) Oxidative stress and the aging brain: From theory to prevention. In DR Riddle (ed) Brain aging: Models, methods, and mechanisms, CRC Press/Taylor & Francis, Boca Ratón
Bradley MA, Markesbery WR, Lovell MA (2010) Increased levels of 4-hydroxynonenal and acrolein in the brain in preclinical Alzheimer disease. Free Radic Biol Med 48(12):1570–1576. https://doi.org/10.1016/j.freeradbiomed.2010.02.016
Sasaoka T (2012) Oxidative stress in neurodegenerative diseases: Friend and foe. Clin Exp Pharmacol Physiol 39(7):597–598. https://doi.org/10.1111/j.1440-1681.2012.05723.x
Beckman JS (1996) Oxidative damage and tyrosine nitration from peroxynitrite. Chem Res Toxicol 9(5):836–844. https://doi.org/10.1021/tx9501445
Wang DP, Yin H, Lin Q, Fang SP, Shen JH, Wu YF, Su SH, Hai J (2019) Andrographolide enhances hippocampal BDNF signaling and suppresses neuronal apoptosis, astroglial activation, neuroinflammation, and spatial memory deficits in a rat model of chronic cerebral hypoperfusion. Naunyn Schmiedeberg's Arch Pharmacol 392:1277–1284. https://doi.org/10.1007/s00210-019-01672-9
Tapia-Rojas C, Schuller A, Lindsay CB, Ureta RC, Mejias-Reyes C, Hancke J, Melo F, Inestrosa NC (2015) Andrographolide activates the canonical Wnt signalling pathway by a mechanism that implicates the non-ATP competitive inhibition of GSK-3beta: Autoregulation of GSK-3beta in vivo. Biochem J 466(2):415–430. https://doi.org/10.1042/BJ20140207
Tapia-Rojas C, Inestrosa NC (2018) Wnt signaling loss accelerates the appearance of neuropathological hallmarks of Alzheimer's disease in J20-APP transgenic and wild-type mice. J Neurochem 144(4):443–465. https://doi.org/10.1111/jnc.14278
Cisternas P, Oliva CA, Torres VI, Barrera DP, Inestrosa NC (2019) Presymptomatic treatment with Andrographolide improves brain metabolic markers and cognitive behavior in a model of early-onset Alzheimer’s disease. Front Cell Neurosci. https://doi.org/10.3389/fncel.2019.00295
Lu J, Ma Y, Wu J, Huang H, Wang X, Chen Z, Chen J, He H et al (2019) A review for the neuroprotective effects of andrographolide in the central nervous system. Biomed Pharmacother 117:109078. https://doi.org/10.1016/j.biopha.2019.109078
Carretta MD, Alarcon P, Jara E, Solis L, Hancke JL, Concha II, Hidalgo MA, Burgos RA (2009) Andrographolide reduces IL-2 production in T-cells by interfering with NFAT and MAPK activation. Eur J Pharmacol 602(2–3):413–421. https://doi.org/10.1016/j.ejphar.2008.11.011
Chen HW, Lin AH, Chu HC, Li CC, Tsai CW, Chao CY, Wang CJ, Lii CK et al (2011) Inhibition of TNF-alpha-induced inflammation by andrographolide via down-regulation of the PI3K/Akt signaling pathway. J Nat Prod 74(11):2408–2413. https://doi.org/10.1021/np200631v
Peng S, Hang N, Liu W, Guo W, Jiang C, Yang X, Xu Q, Sun Y (2016) Andrographolide sulfonate ameliorates lipopolysaccharide-induced acute lung injury in mice by down-regulating MAPK and NF-kappaB pathways. Acta Pharm Sin B 6(3):205–211. https://doi.org/10.1016/j.apsb.2016.02.002
Zhan JY, Wang XF, Liu YH, Zhang ZB, Wang L, Chen JN, Huang S, Zeng HF et al (2016) Andrographolide sodium bisulfate prevents UV-induced skin Photoaging through inhibiting oxidative stress and inflammation. Mediat Inflamm 2016:3271451. https://doi.org/10.1155/2016/3271451
More SV, Kumar H, Kim IS, Song SY, Choi DK (2013) Cellular and molecular mediators of neuroinflammation in the pathogenesis of Parkinson's disease. Mediat Inflamm 2013:952375. https://doi.org/10.1155/2013/952375
Acknowledgments
We thank the “Lithium in Health and Disease” project from the Sociedad Química y Minera de Chile (SQM).
Funding
This work was supported by a postdoctoral grant from FONDECYT (N° 3,140,395 to DSR and N° 11,160,651 to PC) and by grants from the Basal Center of Excellence in Science and Technology (CONICYT PIA/BASAL FB0002 to FB 0002–2014 (Line 3), CONICYT-AFB 170005 and FONDECYT N° 1,160,724 to NCI).
Author information
Authors and Affiliations
Contributions
CL contributed to the western blot analyses and the drafting of this work; JMZ prepared and critically revised the final draft of this manuscript; DSR administered the ANDRO and vehicle solution and manuscript revision; PC contributed to the immunofluorescence analysis and to manuscript revision; NCI and FB contributed to the conception and design of this work as well as the revision of the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lindsay, C.B., Zolezzi, J.M., Rivera, D.S. et al. Andrographolide Reduces Neuroinflammation and Oxidative Stress in Aged Octodon degus. Mol Neurobiol 57, 1131–1145 (2020). https://doi.org/10.1007/s12035-019-01784-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-019-01784-6