Abstract
Purpose
Design and evaluate a knowledge-based model using commercially available artificial intelligence tools for automated treatment planning to efficiently generate clinically acceptable hippocampal avoidance prophylactic cranial irradiation (HA-PCI) plans in patients with small-cell lung cancer.
Materials and methods
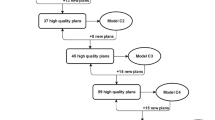
Data from 44 patients with different grades of head flexion (range 45°) were used as the training datasets. A Rapid Plan knowledge-based planning (KB) routine was applied for a prescription of 25 Gy in 10 fractions using two volumetric modulated arc therapy (VMAT) arcs. The 9 plans used to validate the initial model were added to generate a second version of the RP model (Hippo-MARv2). Automated plans (AP) were compared with manual plans (MP) according to the dose-volume objectives of the PREMER trial. Optimization time and model quality were assessed using 10 patients who were not included in the first 44 datasets.
Results
A 55% reduction in average optimization time was observed for AP compared to MP. (15 vs 33 min; p = 0.001).Statistically significant differences in favor of AP were found for D98% (22.6 vs 20.9 Gy), Homogeneity Index (17.6 vs 23.0) and Hippocampus D mean (11.0 vs 11.7 Gy). The AP met the proposed objectives without significant deviations, while in the case of the MP, significant deviations from the proposed target values were found in 2 cases.
Conclusion
The KB model allows automated planning for HA-PCI. Automation of radiotherapy planning improves efficiency, safety, and quality and could facilitate access to new techniques.


Similar content being viewed by others
References
Aupérin A, Arriagada R, Pignon JP, Le Péchoux C, Gregor A, Stephens RJ, et al. Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic cranial irradiation overview collaborative group. N Engl J Med. 1999;341:476–84. https://doi.org/10.1056/NEJM199908123410703.
Slotman B, Faivre-Finn C, Kramer G, Rankin E, Snee M, Hatton M, et al. EORTC radiation oncology group and lung cancer group. Prophylactic cranial irradiation in extensive small-cell lung cancer. N Engl J Med. 2007;357:664–72. https://doi.org/10.1056/NEJMoa071780.
Takahashi T, Yamanaka T, Seto T, Harada H, Nokihara H, Saka H, et al. Prophylactic cranial irradiation versus observation in patients with extensive-disease small-cell lung cancer: a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2017;18:663–71. https://doi.org/10.1016/S1470-2045(17)30230-9.
Wolfson AH, Bae K, Komaki R, Meyers C, Movsas B, Le Pechoux C, et al. Primary analysis of a phase II randomized trial radiation therapy oncology group (RTOG) 0212: impact of different total doses and schedules of prophylactic cranial irradiation on chronic neurotoxicity and quality of life for patients with limited-disease small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2011;81:77–84. https://doi.org/10.1016/j.ijrobp.2010.05.013.
Lok BH, Ma J, Foster A, Perez CA, Shi W, Zhang Z, et al. Factors influencing the utilization of prophylactic cranial irradiation in patients with limited-stage small cell lung cancer. Adv Radiat Oncol. 2017;2:548–54. https://doi.org/10.1016/j.adro.2017.08.001.
Belderbos J, De Ruysscher D, De Jaeger K, Koppe F, Lambrecht MLF, Lievens YN, et al. Phase III trial of prophylactic cranial irradiation with or without hippocampus avoidance in SCLC. J Thorac Oncol. 2021;16:840–9. https://doi.org/10.1016/j.jtho.2020.12.024.
Rodríguez de Dios N, Couñago F, Murcia-Mejía M, Rico-Oses M, Calvo-Crespo P, Samper P, et al. Randomized phase iii trial of prophylactic cranial irradiation with or without hippocampal avoidance for small-cell lung cancer (PREMER): A GICOR-GOECP-SEOR study. J Clin Oncol. 2021;39:3118–27. https://doi.org/10.1200/JCO.21.00639.
Brown PD, Parsons MW, Rusthoven CG, Gondi V. Hippocampal avoidance cranial irradiation: a new standard of care? J Clin Oncol. 2021;39:3093–6. https://doi.org/10.1200/JCO.21.01632.
Hernandez V, Hansen CR, Widesott L, Bäck A, Canters R, Fusella M, et al. What is plan quality in radiotherapy? The importance of evaluating dose metrics, complexity, and robustness of treatment plans. Radiother Oncol. 2020;153:26–33. https://doi.org/10.1016/j.radonc.2020.09.038.
Datta NR, Samiei M, Bodis S. Radiation therapy infrastructure and human resources in low- and middle-income countries: present status and projections for 2020. Int J Radiat Oncol Biol Phys. 2014;1(89):448–57. https://doi.org/10.1016/j.ijrobp.2014.03.002.
Gondi V, Tome WA, Rowley H, Mehta MP. HFippocampal contouring: a contouring atlas for RTOG0933. http://www.rtog.org/CoreLab/ContouringAtlases/HippocampalSparing.aspx
Aviles JEA, Marcos MIC, Sasaki D, Sutherland K, Kane B, Kuusela E. Creation of knowledge-based planning models intended for large scale distribution: minimizing the effect of outlier plans. J Appl Clin Med Phys. 2018;19:215–26. https://doi.org/10.1002/acm2.12322.
Brown PD, Gondi V, Pugh S, Tome WA, Wefel JS, Armstrong TS, for NRG Oncology, et al. Hippocampal avoidance during whole brain radiotheraphy plus memantine for patients with brain metastases: phase III trial NRG Oncology CC001. J Clin Oncol. 2020;38:1019–29.
Das IJ, Cheng C-W, Chopra KL, Mitra RK, Srivastava SP, Glatstein E. Intensity-modulated radiation therapy dose prescription, recording, and delivery: patterns of variability among institutions and treatment planning systems. J Natl Cancer Inst. 2008;100:300–7. https://doi.org/10.1093/jnci/djn020.
Momin S, Fu Y, Lei Y, Roper J, Bradley JD, Curran WJ, et al. Knowledge-based radiation treatment planning: a data-driven method survey. J Appl Clin Med Phys. 2021;22:16–44. https://doi.org/10.1002/acm2.13337.
Fogliata A, Cozzi L, Reggiori G, Stravato A, Lobefalo F, Franzese C, et al. RapidPlan knowledge based planning: iterative learning process and model ability to steer planning strategies. Radiat Oncol. 2019;14:187. https://doi.org/10.1186/s13014-019-1403-0.
Kavanaugh J, Holler S, DeWees T, Robinson C, Bradley JD, Iyengar P, et al. Multi-institutional validation of a knowledge-based planning model for patients enrolled in RTOG 0617: implications for plan quality controls in cooperative group trials. Pract Radiat Oncol. 2019;9:218–27. https://doi.org/10.1016/j.prro.2018.11.007.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Núria Rodríguez de Dios reports personal fees from AstraZeneca, and Siemens Healthcare outside the submitted work. Manuel Algara reports personal fees from Siemens Healthcare and Sysmex outside the submitted work. Enric Fernández-Velilla reports personal fees from Siemens Healthcare outside the submitted work. All other authors declare no competing interests.
Ethical approval and Informed consent
Patients signed the IC to receive HA-PCI according to the routine clinical practice of the department. The analysis of plans was done retrospectively
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Dios N, R., Moñino A, M., Liu, C. et al. Machine learning-based automated planning for hippocampal avoidance prophylactic cranial irradiation. Clin Transl Oncol 25, 503–509 (2023). https://doi.org/10.1007/s12094-022-02963-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-022-02963-z