Abstract
Introduction
Bacteria and cancer cells share a common trait—both possess an electronegative surface that distinguishes them from healthy mammalian counterparts. This opens opportunities to repurpose antimicrobial peptides (AMPs), which are cationic amphiphiles that kill bacteria by disrupting their anionic cell envelope, into anticancer peptides (ACPs). To test this assertion, we investigate the mechanisms by which a pathogen-specific AMP, originally designed to kill bacterial Tuberculosis, potentiates the lytic destruction of drug-resistant cancers and synergistically enhances chemotherapeutic potency.
Materials and Methods
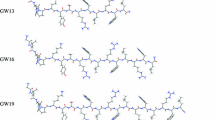
De novo peptide design, paired with cellular assays, elucidate structure-activity relationships (SAR) important to ACP potency and specificity. Using the sequence MAD1, microscopy, spectrophotometry and flow cytometry identify the peptide’s anticancer mechanisms, while parallel combinatorial screens define chemotherapeutic synergy in drug-resistant cell lines and patient derived ex vivo tumors.
Results
SAR investigations reveal spatial sequestration of amphiphilic regions increases ACP potency, but at the cost of specificity. Selecting MAD1 as a lead sequence, mechanistic studies identify that the peptide forms pore-like supramolecular assemblies within the plasma and nuclear membranes of cancer cells to potentiate death through lytic and apoptotic mechanisms. This diverse activity enables MAD1 to synergize broadly with chemotherapeutics, displaying remarkable combinatorial efficacy against drug-resistant ovarian carcinoma cells and patient-derived tumor spheroids.
Conclusions
We show that cancer-specific ACPs can be rationally engineered using nature’s AMP toolbox as templates. Selecting the antimicrobial peptide MAD1, we demonstrate the potential of this strategy to open a wealth of synthetic biotherapies that offer new, combinatorial opportunities against drug resistant tumors.






Similar content being viewed by others
References
Agarwal, R., and S. B. Kaye. Ovarian cancer: strategies for overcoming resistance to chemotherapy. Nat. Rev. Cancer 3:502–516, 2003.
Ahmed, N., and K. Stenvers. Getting to know ovarian cancer ascites: opportunities for targeted therapy-based translational research. Front. Oncol. 3:256, 2013.
Aina, O. H., R. Liu, J. L. Sutcliffe, J. Marik, C.-X. Pan, and K. S. Lam. From combinatorial chemistry to cancer-targeting peptides. Mol. Pharm. 4:631–651, 2007.
Al-Benna, S., Y. Shai, F. Jacobsen, and L. Steinstraesser. Oncolytic activities of host defense peptides. Int. J. Mol. Sci. 12:8027–8051, 2011.
Al-Lazikani, B., U. Banerji, and P. Workman. Combinatorial drug therapy for cancer in the post-genomic era. Nat. Biotechnol. 30:679, 2012.
Andrushchenko, V. V., H. J. Vogel, and E. J. Prenner. Solvent-dependent structure of two tryptophan-rich antimicrobial peptides and their analogs studied by FTIR and CD spectroscopy. Biochim. Biophys. Acta - Biomembr. 1758:1596–1608, 2006.
Anugraham, M., F. Jacob, S. Nixdorf, A. V. Everest-Dass, V. Heinzelmann-Schwarz, and N. H. Packer. Specific glycosylation of membrane proteins in epithelial ovarian cancer cell lines: Glycan structures reflect gene expression and DNA methylation status. Mol. Cell. Proteomics 13:2213–2232, 2014.
Aronson, M. R., A. W. Simonson, L. M. Orchard, M. Llinás, and S. H. Medina. Lipopeptisomes: Anticancer peptide-assembled particles for fusolytic oncotherapy. Acta Biomater. 80:269–277, 2018.
Ashkenazi, A. Targeting the extrinsic apoptosis pathway in cancer. Cytokine Growth Factor Rev. 19:325–331, 2008.
Bahar, A. A., and D. Ren. Antimicrobial peptides. Pharmaceuticals 6:1543–1575, 2013.
Chen, W., H. Ding, P. Feng, H. Lin, and K.-C. Chou. iACP: a sequence-based tool for identifying anticancer peptides. Oncotarget 7:16895, 2016.
Cochran, A. G., N. J. Skelton, and M. A. Starovasnik. Tryptophan zippers: stable, monomeric β-hairpins. Proc. Natl. Acad. Sci. 98:5578–5583, 2001.
DeStefano, C. B., and S. V. Liu. Combinatorial immunotherapy and chemotherapy. In: Early Phase Cancer Immunotherapy, edited by S. P. Patel, and R. Kurzrock. Cham: Springer, 2018, pp. 199–218.
Eckstein, N. Platinum resistance in breast and ovarian cancer cell lines. J. Exp. Clin. Cancer Res. 30:91, 2011.
Emelianova, A. A., D. V. Kuzmin, P. V. Panteleev, M. Sorokin, A. A. Buzdin, and T. V. Ovchinnikova. Anticancer activity of the goat antimicrobial peptide ChMAP-28. Front. Pharmacol. 9:1501, 2018.
Felício, M. R., O. N. Silva, S. Gonçalves, N. C. Santos, and O. L. Franco. Peptides with dual antimicrobial and anticancer activities. Front. Chem. 5:5, 2017.
Fuster, M. M., and J. D. Esko. The sweet and sour of cancer: glycans as novel therapeutic targets. Nat. Rev. Cancer 5:526–542, 2005.
Gajski, G., and V. Garaj-Vrhovac. Melittin: a lytic peptide with anticancer properties. Environ. Toxicol. Pharmacol. 36:697–705, 2013.
Gaspar, D., A. S. Veiga, and M. A. R. B. Castanho. From antimicrobial to anticancer peptides. A review. Front. Microbiol. 4:294, 2013.
Hou, L., X. Zhao, P. Wang, Q. Ning, M. Meng, and C. Liu. Antitumor activity of antimicrobial peptides containing CisoDGRC in CD13 negative breast cancer cells. PLoS ONE 8:e53491, 2013.
Huang, Y., X. Wang, H. Wang, Y. Liu, and Y. Chen. Studies on mechanism of action of anticancer peptides by modulation of hydrophobicity within a defined structural framework. Mol. Cancer Ther. 10:416–426, 2011.
Ishikawa, K., S. H. Medina, J. P. Schneider, and A. J. S. S. Klar. Glycan alteration imparts cellular resistance to a membrane-lytic anticancer peptide. Cell Chem. Biol. 24:149–158, 2017.
Kim, I.-W., J. H. Lee, Y.-N. Kwon, E.-Y. Yun, S.-H. Nam, M.-Y. Ahn, D.-C. Kang, and J. S. Hwang. Anticancer activity of a synthetic peptide derived from harmoniasin, an antibacterial peptide from the ladybug Harmonia axyridis. Int. J. Oncol. 43:622–628, 2013.
Kościuczuk, E. M., P. Lisowski, J. Jarczak, N. Strzałkowska, A. Jóźwik, J. Horbańczuk, J. Krzyżewski, L. Zwierzchowski, and E. Bagnicka. Cathelicidins: family of antimicrobial peptides. A review. Mol. Biol. Rep. 39:10957–10970, 2012.
Kumar, P., J. N. Kizhakkedathu, and S. K. Straus. Antimicrobial peptides: diversity, mechanism of action and strategies to improve the activity and biocompatibility in vivo. Biomolecules 8:4, 2018.
Kuroda, K., T. Fukuda, H. Isogai, K. Okumura, M. Krstic-Demonacos, and E. Isogai. Antimicrobial peptide FF/CAP18 induces apoptotic cell death in HCT116 colon cancer cells via changes in the metabolic profile. Int. J. Oncol. 46:1516–1526, 2015.
Lawler, S. E., M.-C. Speranza, C.-F. Cho, and E. A. Chiocca. Oncolytic viruses in cancer treatment: a review. JAMA Oncol. 3:841–849, 2017.
Manzo, G., M. A. Scorciapino, P. Wadhwani, J. Bürck, N. Pietro Montaldo, M. Pintus, R. Sanna, M. Casu, A. Giuliani, G. Pirri, V. Luca, A. S. Ulrich, and A. C. Rinaldi. Enhanced amphiphilic profile of a short β-stranded peptide improves its antimicrobial activity. PLoS ONE 10:1–18, 2015.
Medina, S. H., and J. P. Schneider. Cancer cell surface induced peptide folding allows intracellular translocation of drug. J. Control. Release 209:317–326, 2015.
Przybyło, M., D. Hoja-Lukowicz, A. Lityńska, and P. Laidler. Different glycosylation of cadherins from human bladder non-malignant and cancer cell lines. Cancer Cell Int. 2:6, 2002.
Ramón-García, S., R. Mikut, C. Ng, S. Ruden, R. Volkmer, M. Reischl, K. Hilpert, and C. J. Thompson. Targeting mycobacterium tuberculosis and other microbial pathogens using improved synthetic antibacterial peptides. Antimicrob. Agents Chemother. 57:2295–2303, 2013.
Reißer, S., E. Strandberg, T. Steinbrecher, and A. S. Ulrich. 3D hydrophobic moment vectors as a tool to characterize the surface polarity of amphiphilic peptides. Biophys. J. 106:2385–2394, 2014.
Riedl, S., D. Zweytick, and K. Lohner. Membrane-active host defense peptides–challenges and perspectives for the development of novel anticancer drugs. Chem. Phys. Lipids 164:766–781, 2011.
Rivel, T., C. Ramseyer, and S. Yesylevskyy. The asymmetry of plasma membranes and their cholesterol content influence the uptake of cisplatin. Sci. Rep. 9:1–14, 2019.
Seo, M.-D., H.-S. Won, J.-H. Kim, T. Mishig-Ochir, and B.-J. Lee. Antimicrobial peptides for therapeutic applications: a review. Molecules 17:12276–12286, 2012.
Sharma, B., and S. S. Kanwar. Phosphatidylserine: a cancer cell targeting biomarker. Semin. Cancer Biol. 52:17–25, 2018.
Simonson, A. W., A. Lawanprasert, T. D. P. Goralski, K. C. Keiler, and S. H. Medina. Bioresponsive peptide-polysaccharide nanogels—a versatile delivery system to augment the utility of bioactive cargo. Nanomedicine 17:391–400, 2019.
Simonson, A. W., A. S. Mongia, M. R. Aronson, J. N. Alumasa, D. C. Chan, A. Bolotsky, A. Ebrahimi, E. A. Proctor, K. C. Keiler, and S. H. Medina. Pathogen-specific de novo antimicrobials engineered through membrane porin biomimicry. ChemRxiv 2020. https://doi.org/10.26434/chemrxiv.12267992.v1.
Suarez-Jimenez, G.-M., A. Burgos-Hernandez, and J.-M. Ezquerra-Brauer. Bioactive peptides and depsipeptides with anticancer potential: sources from marine animals. Mar. Drugs 10:963–986, 2012.
Tao, P., R. Wang, and L. Lai. Calculating partition coefficients of peptides by the addition method. J. Mol. Model. 5:189–195, 1999.
Teixeira, V., M. J. Feio, and M. Bastos. Role of lipids in the interaction of antimicrobial peptides with membranes. Prog. Lipid Res. 51:149–177, 2012.
Thundimadathil, J. Cancer treatment using peptides: current therapies and future prospects. J. Amino Acids 2012:967347, 2012.
Tyagi, A., P. Kapoor, R. Kumar, K. Chaudhary, A. Gautam, and G. P. S. Raghava. In silico models for designing and discovering novel anticancer peptides. Sci. Rep. 3:2984, 2013.
Uphoff, C. C., and H. G. Drexler. Detection of mycoplasma contaminations. In: Basic Cell Culture Protocols, edited by C. D. Helgason, and C. L. Miller. Totowa, NJ: Humana Press, 2005, pp. 13–23.
Zhao, J., Y. Huang, D. Liu, and Y. Chen. Two hits are better than one: synergistic anticancer activity of α-helical peptides and doxorubicin/epirubicin. Oncotarget 6:1769, 2015.
Zheng, L.-H., Y.-J. Wang, J. Sheng, F. Wang, Y. Zheng, X.-K. Lin, and M. Sun. Antitumor peptides from marine organisms. Mar. Drugs 9:1840–1859, 2011.
Acknowledgments
We thank the laboratory of Dr. Joel Schneider at the National Cancer Institute for providing cancer cell lines. We also thank Dr. Matthew Taylor (Penn State University, College of Medicine, Hershey, PA) for donating the NL20 cell line. We thank the laboratories of Dr. Zissis Chroneos (Penn State University, College of Medicine, Hershey, PA), Dr. Pak Kin Wong (Penn State University, PA), and Dr. Kenneth Keiler (Penn State University, PA) for sharing the bacterial strains employed in these studies. We acknowledge and thank the Penn State Microscopy and Cytometry Facility—University Park, PA for assistance with confocal and electron microscopy. We also acknowledge the Penn State X-Ray Crystallography Facility—University Park, PA for use of the CD spectrophotometer. Funding for this research was provided by the Penn State Institute of Energy and the Environment Human Health and the Environment Seed Grant (S.H.M.), NIH:R00CA194309 (K.M.A.), NIH:F31CA236372 (E.S.D.), Penn State College of Engineering Grant (M.R.A.) and Penn State Graduate Research Fellowship (A.W.S.).
Conflict of interest
Authors Matthew R. Aronson, Erika S. Dahl, Jacob A. Halle, Andrew W. Simonson, Rose A. Gogal, Adam B. Glick, Katherine M. Aird and Scott H. Medina declare they have no conflict of interest.
Research Involving Human Rights
No human studies were carried out by the authors for this article. No animal studies were carried out by the authors for this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Michael R. King oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Aronson, M.R., Dahl, E.S., Halle, J.A. et al. Re-engineering Antimicrobial Peptides into Oncolytics Targeting Drug-Resistant Ovarian Cancers. Cel. Mol. Bioeng. 13, 447–461 (2020). https://doi.org/10.1007/s12195-020-00626-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12195-020-00626-z