Abstract
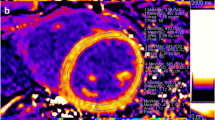
In extensive nonreperfused myocardial infarction (MI), remote fibrosis has been documented. Early reperfusion by primary angioplasty represents the gold standard method to minimize the extension of the infarction. We aimed to ascertain whether fibrosis also affects remote regions in reperfused MI in swine and patients. Swine were subjected to a transient occlusion of the left anterior descending artery followed by 1-week or 1-month reperfusion. Collagen content in the remote area macroscopically, microscopically, by magnetic resonance microimaging, and at the molecular level was similar to controls. In patients with previous MI, samples from autopsies displayed a significant increase in collagen content only in the infarct region. In patients with previous MI submitted to cardiac magnetic resonance-T1 mapping, the extracellular volume fraction in remote segments was similar to that for controls. In all scenarios, the remote region did not show a significant increase of collagen content in comparison with controls.






Similar content being viewed by others
Abbreviations
- α-SMA:
-
Alpha-smooth muscle actin
- CMR:
-
Cardiac magnetic resonance
- COL1A1:
-
Collagen type I alpha 1
- COL1A2:
-
Collagen type I alpha 2
- COL3A1:
-
Collagen type III alpha 1
- ECV:
-
Extracellular volume fraction
- MI:
-
Myocardial infarction
- TGF-β:
-
Transforming growth factor-β
- TS:
-
Thioflavin-S
- TTZ:
-
2,3,5-Triphenyltetrazolium chloride
References
van den Borne, S. W. M., Diez, J., Blankesteijn, W. M., Verjans, J., Hofstra, L., & Narula, J. (2010). Myocardial remodeling after infarction: the role of myofibroblasts. Nature Reviews Cardiology, 7, 30–37.
Daskalopoulos, E. P., Janssen, B. J. A., & Blankesteijn, W. M. (2012). Myofibroblasts in the infarct area: concepts and challenges. Microscopy and Microanalysis, 18, 35–49.
Beltrami, C. A., Finato, N., Rocco, M., Feruglio, G. A., Puricelli, C., Cigola, E., Quaini, F., Sonnenblick, E. H., Olivetti, G., & Anversa, P. (1994). Structural basis of end-stage failure in ischemic cardiomyopathy in humans. Circulation, 89, 151–163.
Cleutjens, J. P. M., Verluyten, M. J. A., Smiths, J. F. M., & Daemen, M. J. A. P. (1995). Collagen remodeling after myocardial infarction in the rat heart. American Journal of Pathology, 147, 325–338.
Sun, Y., & Weber, K. T. (2000). Infarct scar: a dynamic tissue. Cardiovascular Research, 46, 250–256.
Sun, Y., Zhang, J. Q., Zhang, J., & Lamparter, S. (2000). Cardiac remodeling by fibrous tissue after infarction in rats. Journal of Laboratory and Clinical Medicine, 135, 316–323.
Sun, Y. (2009). Myocardial repair/remodelling following infarction: roles of local factors. Cardiovascular Research, 81, 482–490.
dos Santos, L., Gonçalves, G. A., Davel, A. P., Santos, A. A., Krieger, J. E., Rossoni, L. V., & Tucci, P. J. (2013). Cell therapy prevents structural, functional and molecular remodeling of remote non-infarcted myocardium. International Journal of Cardiology, 168, 3829–3836.
Hervas, A., de Dios, E., Forteza, M. J., Miñana, G., Nuñez, J., Ruiz-Sauri, A., Bonanad, C., Perez-Sole, N., Chorro, F. J., & Bodi, V. (2015). Intracoronary infusion of thioflavin-S to study microvascular obstruction in a model of myocardial infarction. Revista Española de Cardiología, 68, 928–934.
Hervas, A., Ruiz-Sauri, A., de Dios, E., Forteza, M. J., Minana, G., Nunez, J., Gomez, C., Bonanad, C., Perez-Sole, N., Gavara, J., Chorro, F. J., & Bodi, V. (2016). Inhomogeneity of collagen organization within the fibrotic scar after myocardial infarction: results in a swine model and in human samples. Journal of Anatomy, 228, 47–58.
Marijianowski, M. M. H., Teeling, P., & Becker, A. E. (1997). Remodeling after myocardial infarction in humans is not associated with interstitial fibrosis of noninfarcted myocardium. Journal of the American College of Cardiology, 30, 76–82.
Tarkia, M., Stark, C., Haavisto, M., Kentala, R., Vähäsilta, T., Savunen, T., Strandberg, M., Hynninen, V. V., Saunavaara, V., Tolvanen, T., Teräs, M., Rokka, J., Pietilä, M., Saukko, P., Roivainen, A., Saraste, A., & Knuuti, J. (2015). Cardiac remodeling in a new pig model of chronic heart failure: assessment of left ventricular functional, metabolic, and structural changes using PET, CT, and echocardiography. Journal of Nuclear Cardiology, 22, 655–665.
van den Borne, S. W. M., Isobe, S., Verjans, J. W., Petrov, A., Lovhaug, D., Li, P., Zandbergen, H. R., Ni, Y., Frederik, P., Zhou, J., Arbo, B., Rogstad, A., Cuthbertson, A., Chettibi, S., Reutelingsperger, C., Blankesteijn, W. M., Smits, J. F., Daemen, M. J., Zannad, F., Vannan, M. A., Narula, N., Pitt, B., Hofstra, L., & Narula, J. (2008). Molecular imaging of interstitial alterations in remodeling myocardium after myocardial infarction. Journal of the American College of Cardiology, 52, 2017–2028.
Prat-Vidal, C., Gálvez-Montón, C., Nonell, L., Puigdecanet, E., Astier, L., Solé, F., & Bayes-Genis, A. (2013). Identification of temporal and region-specific myocardial gene expression patterns in response to infarction in swine. PLoS ONE, 8, e54785.
Monreal, G., Nicholson, L. M., Han, B., Joshi, M. S., Phillips, A. B., Wold, L. E., Bauer, J. A., & Gerhardt, M. A. (2008). Cytoskeletal remodeling of desmin is a more accurate measure of cardiac dysfunction than fibrosis or myocyte hypertrophy. Life Sciences, 83, 786–794.
Frangogiannis, N. G. (2014). The inflammatory response in myocardial injury, repair and remodeling. Nature Reviews Cardiology, 11, 255–265.
Vilahur, G., Juan-Babot, O., Peña, E., Oñate, B., Casaní, L., & Badimon, L. (2011). Molecular and cellular mechanisms involved in cardiac remodeling after acute myocardial infarction. Journal of Molecular and Cellular Cardiology, 50, 522–533.
Hao, J., Ju, H., Zhao, S., Junaid, A., Scammell-La Fleur, T., & Dixon, I. M. C. (1999). Elevation of expression of Smads 2, 3, and 4, decorin and TGF-beta in the chronic phase of myocardial infarct scar healing. Journal of Molecular and Cellular Cardiology, 31, 667–678.
Willems, I. E. M. G., Havenith, M. G., De Mey, J. G. R., & Daemen, M. J. A. P. (1994). The alpha-smooth muscle actin-positive cells in healing human myocardial scars. American Journal of Pathology, 145, 868–875.
Gonzalez-Segura, A., Morales, J. M., Gonzalez-Darder, J. M., Cardona-Marsal, R., Lopez-Gines, C., Cerda-Nicolas, M., & Monleon, D. (2011). Magnetic resonance microscopy at 14 Tesla and correlative histopathology of human brain tumor tissue. PLoS One, 6, e27442.
White, S. K., Sado, D. M., Fontana, M., Banypersad, S. M., Maestrini, V., Flett, A. S., Piechnik, S. K., Robson, M. D., Hausenloy, D. J., Sheikh, A. M., Hawkins, P. N., & Moon, J. C. (2013). T1 mapping for myocardial extracellular volume measurement by CMR: bolus only versus primed infusion technique. JACC. Cardiovascular Imaging, 6, 955–962.
Ugander, M., Oki, A. J., Hsu, L. Y., Kellman, P., Greiser, A., Aletras, A. H., Sibley, C. T., Chen, M. Y., Bandettini, W. P., & Arai, A. E. (2012). Extracellular volume imaging by magnetic resonance imaging provides insights into overt and sub-clinical myocardial pathology. European Heart Journal, 33, 1268–1278.
de Souza, R. R. (2002). Aging of myocardial collagen. Biogerontology, 3, 325–335.
Olivetti, G., Melissari, M., Capasso, J. M., & Anversa, P. (1991). Cardiomyopathy of the aging human heart. Myocyte loss and reactive cellular hypertrophy. Circulation Research, 68, 1560–1568.
Horn, M. A., & Trafford, A. W. (2015). Aging and the cardiac collagen matrix: novel mediators of fibrotic remodelling. Journal of Molecular and Cellular Cardiology. doi:10.1016/j.yjmcc.2015.11.005.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Human Subjects Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and conform to the ethical guidelines of the 1975 Declaration of Helsinki as revised in 2000.
Animal Studies Statement
The local Animal Care and Use Committee approved the study, and it conforms to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1993).
Conflict of Interest
The authors declare that they have no conflicts of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Sources of Funding
This work was supported by the ‘Instituto de Salud Carlos III’ and co-funded by ‘FEDER’ [grant numbers PI14/00271, PIE15/00013] and by the ‘Generalitat Valenciana’ [grant number PROMETEO/2013/007].
Additional information
Associate Editor Enrique Lara-Pezzi oversaw the review of this article
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Online Resource 1
Expanded methodology used in the study. (PDF 443 kb)
Online Resource 2
Table of risk factors and baseline characteristics of controls and patients with previous myocardial infarcts submitted to cardiac magnetic resonance-T1 mapping. (PDF 53 kb)
Rights and permissions
About this article
Cite this article
Hervas, A., Ruiz-Sauri, A., Gavara, J. et al. A Multidisciplinary Assessment of Remote Myocardial Fibrosis After Reperfused Myocardial Infarction in Swine and Patients. J. of Cardiovasc. Trans. Res. 9, 321–333 (2016). https://doi.org/10.1007/s12265-016-9698-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12265-016-9698-9