Abstract
Background
The optimal positioning of eribulin treatment remains unclear. This study aimed to investigate the effectiveness of eribulin administration as first- and second-line chemotherapy in patients with endocrine-resistant advanced or metastatic breast cancer (AMBC) in the real-world clinical setting.
Methods
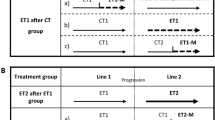
This multi-institutional prospective cohort study enrolled patients with triple-negative AMBC or estrogen receptor-positive AMBC refractory to at least one previous endocrine therapy. The overall survival (OS) from the start of first-line (OS1) and second-line chemotherapy (OS2) was assessed. Data analysis included real-world chemotherapy sequences of first- to third-line chemotherapy regimens. The adjusted hazard ratio (HR) with 95% confidence interval (CI) for treatment regimen comparison was calculated using a stratified proportional hazards model.
Results
Among 201 patients enrolled, 180 were included in the final analysis. Eribulin was administered as first- and second-line chemotherapy to 46 (26.6%) and 70 (47.9%) patients, respectively. Median OS1 and OS2 were 2.25 (95% CI 1.07–2.68) and 1.75 (95% CI, 1.28–2.45) years for first- and second-line eribulin, respectively. Oral 5-FU followed by eribulin had a numerically longer OS1 (2.84 years) than the other sequences. Among patients who proceeded to second-line or later chemotherapy, the median OS1 for those treated with anthracycline or taxane as first- or second-line (n = 98) was 2.56 years (95% CI 2.27–2.74), while it was 2.87 years (95% CI 2.20–4.32) for those who avoided anthracycline and taxane as first- and second-line (n = 48) (adjusted HR, 1.20; 95% CI 0.70–2.06). In the exploratory analysis, OS1 was 2.55 (95% CI 2.14–2.75) and 2.91 years (95% CI 2.61–4.32) for those aged < 65 and ≥ 65 years, respectively (adjusted HR of ≥ 65, 0.91; 95% CI 0.56–1.46).
Conclusions
Eribulin or oral 5-FU administration in first- and second-line chemotherapy without anthracycline/taxane was acceptable in the real-world setting.
Trial registration
This study is registered with Clinical Trials.gov (NCT 02,551,263).




Similar content being viewed by others
References
Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N Engl J Med. 2012;367:1998–2005. https://doi.org/10.1056/NEJMoa1206809.
Cardoso F, Paluch-Shimon S, Senkus E, Curigliano G, Aapro MS, André F, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5). Ann Oncol. 2020;31:1623–49. https://doi.org/10.1016/j.annonc.2020.09.010.
Cardoso F, Spence D, Mertz S, Corneliussen-James D, Sabelko K, Gralow J, et al. Global analysis of advanced/metastatic breast cancer: decade report (2005–2015). Breast. 2018;39:131–8. https://doi.org/10.1016/j.breast.2018.03.002.
Shimoi T, Nagai SE, Yoshinami T, Takahashi M, Arioka H, Ishihara M, et al. The Japanese Breast Cancer Society Clinical Practice Guidelines for systemic treatment of breast cancer. 2018 ed.. Breast Cancer 2020;27: 322–31. https://doi.org/10.1007/s12282-020-01085-0
Hortobagyi GN. Treatment of breast cancer. N Engl J Med. 1998;339:974–84. https://doi.org/10.1056/NEJM199810013391407.
Schmid P, Adams S, Rugo HS, Schneeweiss A, Barrios CH, Iwata H, et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med. 2018;379:2108–21. https://doi.org/10.1056/NEJMoa1809615.
Robson M, Im SA, Senkus E, Xu B, Domchek SM, Masuda N, et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377:523–33. https://doi.org/10.1056/NEJMoa1706450.
Katsumata N, Watanabe T, Minami H, Aogi K, Tabei T, Sano M, et al. Phase III trial of doxorubicin plus cyclophosphamide (AC), docetaxel, and alternating AC and docetaxel as front-line chemotherapy for metastatic breast cancer: Japan Clinical Oncology Group trial (JCOG9802). Ann Oncol. 2009;20:1210–5. https://doi.org/10.1093/annonc/mdn781.
Sledge GW, Neuberg D, Bernardo P, Ingle JN, Martino S, Rowinsky EK, et al. Phase III trial of doxorubicin, paclitaxel, and the combination of doxorubicin and paclitaxel as front-line chemotherapy for metastatic breast cancer: an intergroup trial (E1193). J Clin Oncol. 2003;21:588–92. https://doi.org/10.1200/JCO.2003.08.013.
Takashima T, Mukai H, Hara F, Matsubara N, Saito T, Takano T, et al. Taxanes versus S-1 as the first-line chemotherapy for metastatic breast cancer (SELECT BC): an open-label, non-inferiority, randomised phase 3 trial. Lancet Oncol. 2016;17:90–8. https://doi.org/10.1016/S1470-2045(15)00411-8.
Mukai H, Uemura Y, Akabane H, Watanabe T, Park Y, Takahashi M, et al. Anthracycline-containing regimens or taxane versus S-1 as first-line chemotherapy for metastatic breast cancer. Br J Cancer. 2021;125:1217–25. https://doi.org/10.1038/s41416-021-01531-6.
Jordan MA, Kamath K, Manna T, Okouneva T, Miller HP, Davis C, et al. The primary antimitotic mechanism of action of the synthetic halichondrin E7389 is suppression of microtubule growth. Mol Cancer Ther. 2005;4:1086–95. https://doi.org/10.1158/1535-7163.MCT-04-0345.
Smith JA, Wilson L, Azarenko O, Zhu X, Lewis BM, Littlefield BA, et al. Eribulin binds at microtubule ends to a single site on tubulin to suppress dynamic instability. Biochemistry. 2010;49:1331–7. https://doi.org/10.1021/bi901810u.
Cortes J, O’Shaughnessy J, Loesch D, Blum JL, Vahdat LT, Petrakova K, et al. Eribulin monotherapy versus treatment of physician’s choice in patients with metastatic breast cancer (EMBRACE): a phase 3 open-label randomised study. Lancet. 2011;377:914–23. https://doi.org/10.1016/S0140-6736(11)60070-6.
Kaufman PA, Awada A, Twelves C, Yelle L, Perez EA, Velikova G, et al. Phase III open-label randomized study of eribulin mesylate versus capecitabine in patients with locally advanced or metastatic breast cancer previously treated with an anthracycline and a taxane. J Clin Oncol. 2015;33:594–601. https://doi.org/10.1200/JCO.2013.52.4892.
Yoshida T, Ozawa Y, Kimura T, Sato Y, Kuznetsov G, Xu S, et al. Eribulin mesilate suppresses experimental metastasis of breast cancer cells by reversing phenotype from epithelial-mesenchymal transition (EMT) to mesenchymal-epithelial transition (MET) states. Br J Cancer. 2014;110:1497–505. https://doi.org/10.1038/bjc.2014.80.
Kashiwagi S, Asano Y, Goto W, Takada K, Takahashi K, Hatano T, et al. Mesenchymal-epithelial transition and tumor vascular remodeling in eribulin chemotherapy for breast cancer. Anticancer Res. 2018;38:401–10. https://doi.org/10.21873/anticanres.12236
Funahashi Y, Okamoto K, Adachi Y, Semba T, Uesugi M, Ozawa Y, et al. Eribulin mesylate reduces tumor microenvironment abnormality by vascular remodeling in preclinical human breast cancer models. Cancer Sci. 2014;105:1334–42. https://doi.org/10.1111/cas.12488.
Twelves C, Cortes J, Kaufman PA, Yelle L, Awada A, Binder TA, et al. “New” metastases are associated with a poorer prognosis than growth of pre-existing metastases in patients with metastatic breast cancer treated with chemotherapy. Breast Cancer Res. 2015;17:150. https://doi.org/10.1186/s13058-015-0657-1.
Kotake T, Kikawa Y, Takahara S, Tsuyuki S, Yoshibayashi H, Suzuki E. Impact of eribulin monotherapy on post-progression survival in patients with HER2-negative advanced or metastatic breast cancer. Int J Cancer Clin Res. 2016;3:061. https://doi.org/10.23937/2378-3419/3/4/1061
Takashima T, Tokunaga S, Tei S, Nishimura S, Kawajiri H, Kashiwagi S, et al. A phase II, multicenter, single-arm trial of eribulin as first-line chemotherapy for HER2-negative locally advanced or metastatic breast cancer. Springerplus. 2016;5:164. https://doi.org/10.1186/s40064-016-1833-1.
Hayashida T, Jinno H, Mori K, Sato H, Matsui A, Sakurai T, et al. Phase II trial of eribulin mesylate as a first- or second-line treatment for locally advanced or metastatic breast cancer: a multicenter, single-arm trial. BMC Cancer. 2018;18:701. https://doi.org/10.1186/s12885-018-4628-7.
Kimura K, Iwamoto M, Tanaka S, Yamamoto D, Yoshidome K, Ogura H, et al. A phase II, multicenter, single-arm trial of eribulin as first- or second-line chemotherapy for HER2-negative advanced or metastatic breast cancer: evaluation of efficacy, safety, and patient-reported outcomes. Cancer Chemother Pharmacol. 2018;81:923–33. https://doi.org/10.1007/s00280-018-3567-y.
Ortega V, Antón A, Garau I, Afonso N, Calvo L, Fernández Y, et al. Phase II, multicenter, single-arm trial of eribulin as first-line therapy for patients with aggressive taxane-pretreated HER2-negative metastatic breast cancer: the MERIBEL study. Clin Breast Cancer. 2019;19:105–12. https://doi.org/10.1016/j.clbc.2018.12.012.
Cortes J, Hudgens S, Twelves C, Perez EA, Awada A, Yelle L, et al. Health-related quality of life in patients with locally advanced or metastatic breast cancer treated with eribulin mesylate or capecitabine in an open-label randomized phase 3 trial. Breast Cancer Res Treat. 2015;154:509–20. https://doi.org/10.1007/s10549-015-3633-7.
Liu MC, Hillman DW, Frith AE, Lyss AP, Weckstein DJ, Moreno-Aspitia A, et al. Randomized phase III trial of eribulin (E) versus standard weekly paclitaxel (P) as first- or second-line therapy for locally recurrent or metastatic breast cancer (MBC). J Clin Oncol. 2020;38 (15_suppl):1016–. https://doi.org/10.1200/JCO.2020.38.15_suppl.1016
Van Herck Y, Feyaerts A, Alibhai S, Papamichael D, Decoster L, Lambrechts Y, et al. Is cancer biology different in older patients? Lancet Healthy Longev. 2021;2:e663–77. https://doi.org/10.1016/S2666-7568(21)00179-3.
Petrelli F, Cabiddu M, Coinu A, Borgonovo K, Ghilardi M, Lonati V, et al. Prognostic role of lactate dehydrogenase in solid tumors: a systematic review and meta-analysis of 76 studies. Acta Oncol. 2015;54:961–70. https://doi.org/10.3109/0284186X.2015.1043026.
Ding J, Karp JE, Emadi A. Elevated lactate dehydrogenase (LDH) can be a marker of immune suppression in cancer: interplay between hematologic and solid neoplastic clones and their microenvironments. Cancer Biomark. 2017;19:353–63. https://doi.org/10.3233/CBM-160336.
Zhao S, Jiang T, Zhang L, Yang H, Liu X, Jia Y, et al. Clinicopathological and prognostic significance of regulatory T cells in patients with non-small cell lung cancer: a systematic review with meta-analysis. Oncotarget. 2016;7:36065–73. https://doi.org/10.18632/oncotarget.9130
Stämpfli MR, Anderson GP. How cigarette smoke skews immune responses to promote infection, lung disease and cancer. Nat Rev Immunol. 2009;9:377–84. https://doi.org/10.1038/nri2530.
Acknowledgements
The Translational Research Center for Medical Innovation (TRI) conducted this study jointly with the Kobe City Medical Center General Hospital, Kyoto University Hospital, and other medical institutions. We would like to thank Dr. Tabuchi, Ms. Nomura, Ms. Nakagawa, Mr. Kidena, and the investigators of the KBCRN E-SPEC study as well as the patients who participated in the study. We would like to thank Editage (www.editage.com) for English language editing.
Funding
This work was supported by Eisai Co., Ltd. Eisai was not involved in the design and conduct of the study or in the data analysis and interpretation of the results. A quadripartite contract for conducting this study was made between Eisai, Kobe City Medical Center General Hospital, Kyoto University and TRI.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yuichiro Kikawa received honoraria from Eisai, Novartis, Pfizer, Eli Lilly, Taiho, and Chugai, outside the submitted work. Hiroyasu Yamashiro received honoraria from Chugai, Daiich-Sankyo, Pfizer, Kyowa Kirin, Eisai, Eli Lilly, Takeda, and Taiho, outside the submitted work. Masahiro Takada received honoraria from Chugai, AstraZeneca, Pfizer, Eli Lilly, Eisai, Daiichi Sankyo, and Kyowa-Kirin as well as grants from Eisai and Nipponkayaku, outside the submitted work. Hiroshi Ishiguro received honoraria from JMS, Taiho, Daiichi-Sankyo, Eisai, Chugai, and Kyowa-Hakko-Kirin outside the submitted work and is on the board of directors of the JBCRG association, Kyoto Breast cancer Research Network; he is also an Executive Committee member of Japan Supportive, Palliative and Psychosocial Oncology Group. Tatsuo Kagimura received grants from Eisai, during the conduct of the study. Tetsuya Taguchi received honoraria from Eisai, Daiichi Sankyo, and Chugai, outside the submitted work. Tomoharu Sugie received honoraria from Chugai, Eisai, Pfizer, Astra Zeneca, Lilly, MSD, Novaris, Takeda, Kyowa-Kirin, Genomic Health, and Devicor as well as grants from KBBM, outside the submitted work. Masakazu Toi received grants and honoraria from Chugai, Takeda, Pfizer, Kyowa-Hakko-Kirin, Taiho, Eisai, Daiichi-Sankyo, Astra Zeneca, Shimadzu, and Nippon Kayaku; honoraria from Eli Lilly, MSD, Genomic Health, Novartis, Konica Minolta, BMS, and Yakult; grants from JBCRG association, Astellas, and AFI technologies, outside the submitted work; and is on the board of directors of the JBCRG association, Organisation for Oncology and Translational Research, and Kyoto Breast cancer Research Network. The remaining authors have no conflicts of interest to disclose.
Ethics approval
The institutional review board at each study site approved the final protocol. This study was conducted in accordance with the Japanese Guidelines for Clinical Research of the Ministry of Health, Labour and Welfare and the Declaration of Helsinki.
Informed consent
All participants provided written informed consent prior to study participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Kikawa, Y., Kotake, T., Tsuyuki, S. et al. Effectiveness of eribulin as first-line or second-line chemotherapy for HER2-negative hormone-resistant advanced or metastatic breast cancer: findings from the multi-institutional, prospective, observational KBCRN A001: E-SPEC study. Breast Cancer 29, 796–807 (2022). https://doi.org/10.1007/s12282-022-01357-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12282-022-01357-x