Abstract
Introduction
Frailty is considered as an early stage of disability which, differently from disability, is still amenable for preventive interventions and is reversible. In 2011, the “Geriatric Frailty Clinic (G.F.C) for Assessment of Frailty and Prevention of Disability” was created in Toulouse, France, in association with the University Department of General Medicine and the Midi-Pyrenees Regional Health Authority. This structure aims to support the comprehensive and multidisciplinary assessment of frail older persons, to identify the specific causes of frailty and to design a personalized preventive plan of intervention against disability. In the present paper, we describe the G.F.C structure, organization, details of the global evaluation and preventive interventions against disability, and provide the main characteristics of the first 1,108 patients evaluated during the first two years of operation.
Methods
Persons aged 65 years and older, considered as frail by their physician (general practitioner, geriatrician or specialist) in the Toulouse area, are invited to undergo a multidisciplinary evaluation at the G.F.C. Here, the individual is assessed in order to detect the potential causes for frailty and/or disability. At the end of the comprehensive evaluation, the team members propose to the patient (in agreement with the general practitioner) a Personalized Prevention Plan (PPP) specifically tailored to his/her needs and resources. The G.F.C also provides the patient’s follow-up in close connection with family physicians.
Results
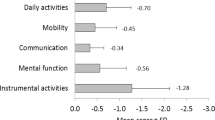
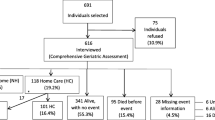
Mean age of our population was 82.9 6.1 years. Most patients were women (n=686, 61.9%). According to the Fried criteria, 423 patients (39.1%) were pre-frail, and 590 (54.5%) frail. Mean ADL (Activities of Daily Living) score was 5.5±1.0. Consistently, IADL (Instrumental ADL) showed a mean score of 5.6 2.4. The mean gait speed was 0.78±0.27 and 25.6% (272) of patients had a SPPB (Short Physical Performance Battery) score equal to or higher than 10. Dementia was observed in 14.9% (111) of the G.F.C population according to the CDR scale (CDR ≥2). Eight percent (84) presented an objective state of protein-energy malnutrition with MNA (Mini Nutritional Assessment) score < 17 and 39.5% (414) were at risk of malnutrition (MNA=17–23.5). Concerning PPP, for 54.6% (603) of patients, we found at least one medical condition which needed a new intervention and for 32.8% (362) substantial therapeutic changes were recommended. A nutritional intervention was proposed for 61.8% (683) of patients, a physical activity intervention for 56.7% (624) and a social intervention for 25.7% (284). At the time of analysis, a one-year reassessment had been carried out for 139 (26.7%) of patients.
Conclusions
The G.F.C was developed to move geriatric medicine to frailty, an earlier stage of disability still reversible. Its particularity is that it is intended for a single target population that really needs preventive measures: the frail elderly screened by physicians. The screening undergone by physicians was really effective because 93.6% of the subjects who referred to this structure were frail or pre-frail according to Fried’s classification and needed different medical interventions. The creation of units like the G.F.C, specialized in evaluation, management and prevention of disability in frail population, could be an interesting option to support general practitioners, promote the quality of life of older people and increase life expectancy without disability.
Similar content being viewed by others
References
Kinsella K, Phillips DR. Global aging: the challenge of success. Population bulletin vol. 60, no. 1. Washington: Population Reference Bureau, 2005.
United Nations. The world at six billion. 12 October 1999. www.un.org/esa/population/publications/sixbillion/sixbilpartl.pdf (accessed January 15,2014).
World Population Prospects: The 2006 Revision, http://www.un.org/esa/population/publications/wpp2006/WPP2006_Highlights_rev.pdf (accessed January 15,2014)
Bandeen-Roche K, Xue Q-L, Ferrucci L, Walston J, Guralnik JM, Chaves P, Zeger SL, Fried LP. Phenotype of frailty: characterization in the women’s health and aging studies. J. Gerontol A Biol Sci Med Sci 2006; 61: 262–266.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56: M146–M156.
Song X, Mitnitski A, Rockwood K. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc 2010; 58: 681–687.
Mission au profit du président de la république. Rapport Andre Trillard; June 2011. http://www.ladocumentationfrancaise.fr/var/storage/rapports-publics/114000390/0000.pdf (accessed February 13,2014).
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013; 381:752–762.
De Vries NM, Staal JB, van Ravensberg CD, Hobbelen JSM, Olde Rikkert MGM, Nijhuis-van der Sanden MWG. Outcome instruments to measure frailty: a systematic review. Ageing Res Rev 2011; 10: 104–114.
Sternberg SA, Wershof Schwartz A, Karunananthan S, Bergman H, Mark Clarfield A. The identification of frailty: a systematic literature review. J Am Geriatr Soc 2011; 59: 2129–2138.
Gloth FM 3rd, Walston J, Meyer J, Pearson J. Reliability and validity of the Frail Elderly Functional Assessment questionnaire. Am J Phys Med Rehabil 1995; 74: 45–53.
Gloth FM 3rd, Scheve AA, Shah S, Ashton R, McKinney R. The Frail Elderly Functional Assessment questionnaire: its responsiveness and validity in alternative settings. Arch Phys Med Rehabil 1999; 80: 1572–1576.
Subra J, Gillette-Guyonnet S, Cesari M, Oustric S, Vellas B; Platform Team. The integration of frailty into clinical practice: preliminary results from the Gérontopôle. J Nutr Health Aging. 2012; 16: 714–720.
Vellas B, Balardy L, Gillette-Guyonnet S, Abellan Van Kan G, Ghisolfi-Marque A, Subra J, Bismuth S, Oustric S, Cesari M. Looking for frailty in community-dwelling older persons: the Gérontopôle Frailty Screening Tool (GFST). J Nutr Health Aging 2013; 17:629–631.
Fiche points clés et solutions, Haute Autorité de Santé (HAS), http://www.hassante.fr/portail/upload/docs/application/pdf/2013-06/fiche_parcours_fragilite_vf.pdf (accessed January 15, 2014).
Buschke H, Kuslansky G, Katz M, Stewart WF, Sliwinski MJ, Eckholdt HM, Lipton RB. Screening for dementia with the memory impairment screen. Neurology 1999; 52: 231–238.
Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12: 189–198.
Morris JC. Clinical dementia rating: a reliable and valid diagnostic and staging measure for dementia of the Alzheimer type. Int Psychogeriatr Suppl 1997; 1:173–176; discussion 177–178.
Katz S, Ford AB, Moskovitz RW, Jackson BA, Jaffe MW. Studies of Illness in the Aged. the Index of Adl: A Standardized Measure of Biological and Psychosocial Function. JAMA 1963; 185: 914–919.
Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969; 9: 179–186.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994; 49: M85–M94.
Guigoz Y, Vellas B. The Mini Nutritional Assessment (MNA) for grading the nutritional state of elderly patients: presentation of the MNA, history and validation. Nestle Nutr Workshop Ser Clin Perform Programme 1999; 1: 3–11; discussion 11–12.
Sheikh JI, Yesavage JA. Geriatric Depression Scale: recent evidence and development of a shorter version. Clin Gerontol 1986; 5: 165–172.
Sindhusake D, Mitchell P, Smith W, Golding M, Newall P, Hartley D, et al. Validation of self-reported hearing loss. The Blue Mountains Hearing Study. Int J Epidemiol 2001; 30: 1371–1378.
O’Connell B, Fonda D, Day K, Ostaszkiewicz J, Hawkins M, Gaskin C, Pinikahana J. Development of screening and assessment tools for continence management in residential aged care. An Australian Government Initiative. Deakin University 2006. http://www.bladderbowel.gov.au/assets/doc/ncms/Phasel-2WorkforceSupport7RESI.pdf (accessed January 27, 2014).
Chalmers JM, King PL, Spencer AJ, Wright FA, Carter KD. The oral health assessment tool validity and reliability. Aust Dent J 2005; 50: 191–199.
Barry MJ, Fowler FJ Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, Cockett AT. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association, J Urol 1992; 148: 1549–1557.
Cesari M, Gambassi G, van Kan GA, Vellas B. The frailty phenotype and the frailty index: different instruments for different purposes. Age Ageing 2014; 43: 10–12.
Carr D, Jackson T, Alquire P. Characteristics of an elderly driving population referred to a geriatric assessment center. J Am Geriatr Soc 1990; 38: 1145–1150.
Epstein AM, Hall JA, Besdine R, Cumella E Jr, Feldstein M, McNeil BJ, Rowe JW. The emergence of geriatric assessment units. The “new technology of geriatrics”. Ann Intern Med 1987; 106: 299–303.
Supiano MA, Alessi C, Chernoff R, Goldberg A, Morley JE, Schmader KE, Shay K; GRECC Directors Association. Department of Veterans Affairs Geriatric Research. Education and Clinical Centers: translating aging research into clinical geriatrics. J Am Geriatr Soc 2012; 60: 1347–1356.
Longo WE, Cheadle W, Fink A, Kozol R, DePalma R, Rege R, Neumayer L, Tarpley J, Tarpley M, Joehl R, Miller TA, Rosendale D, Itani K. The role of the Veterans Affairs Medical Centers in patient care, surgical education, research and faculty development. Am J Surg 2005; 190: 662–675.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Tavassoli, N., Guyonnet, S., Abellan Van Kan, G. et al. Description of 1,108 older patients referred by their physician to the “Geriatric Frailty Clinic (G.F.C) for assessment of frailty and prevention of disability” at the gerontopole. J Nutr Health Aging 18, 457–464 (2014). https://doi.org/10.1007/s12603-014-0462-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-014-0462-z