Abstract
Background
Normotensive pregnancy may develop into preeclampsia (PE) and other adverse pregnancy complications (APCs), for which the causes are still unknown. Suboptimal health status (SHS), a physical state between health and disease, might contribute to the development and progression of PE. By integration of a routine health measure in this Ghanaian Suboptimal Health Cohort Study, we explored the usefulness of a 25-question item SHS questionnaire (SHSQ-25) for early screening and prediction of normotensive pregnant women (NTN-PW) likely to develop PE.
Methods
We assessed the overall health status among a cohort of 593 NTN-PW at baseline (10–20 weeks gestation) and followed them at 21–31 weeks until 32–42 weeks. After an average of 20 weeks follow-up, 498 participants returned and were included in the final analysis. Hematobiochemical, clinical and sociodemographic data were obtained.
Results
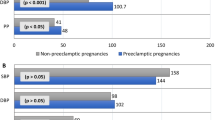
Of the 498 participants, 49.8% (248/498) had ‘high SHS’ at baseline (61.7% (153/248) later developed PE) and 38.3% (95/248) were NTN-PW, whereas 50.2% (250/498) had ‘optimal health’ (17.6% (44/250) later developed PE) and 82.4% (206/250) were NTN-PW. At baseline, high SHS score yielded a significantly (p < 0.05) increased adjusted odds ratio, a wider area under the curve (AUC) and a higher sensitivity and specificity for the prediction of PE (3.67; 0.898; 91.9% and 87.8%), PE coexisting with intrauterine growth restriction (2.86, 0.838; 91.5% and 75.9%), stillbirth (2.52; 0.783; 96.6% and 60.0%), hemolysis elevated liver enzymes and low platelet count (HELLP) syndrome (2.08; 0.800; 97.2% and 63.8%), acute kidney injury (2.20; 0.825; 95.3% and 70.0%) and dyslipidaemia (2.80; 0.8205; 95.7% and 68.4%) at 32–42 weeks gestation.
Conclusions
High SHS score is associated with increased incidence of PE; hence, SHSQ-25 can be used independently as a risk stratification tool for adverse pregnancy outcomes thereby creating an opportunity for predictive, preventive and personalized medicine.



Similar content being viewed by others
Abbreviations
- SHS:
-
suboptimal health status
- OHS:
-
optimal health status
- SHSQ-25:
-
25-question-based suboptimal health status questionnaire
- GHOACS:
-
Ghanaian Suboptimal Health Cohort Study
- PE:
-
preeclampsia
- APCs:
-
adverse pregnancy complications
- PPPM:
-
preventive, predictive and personalized medicine
- IUGR:
-
intrauterine growth restriction
- HELLP:
-
hemolysis elevated liver enzymes and low platelet count
- SBP:
-
systolic blood pressure
- DBP:
-
diastolic blood pressure
- Mg:
-
magnesium
- Ca:
-
calcium
- Na:
-
sodium
- K:
-
potassium
- Cl:
-
chloride
- LDH:
-
lactate dehydrogenase
- UA:
-
uric acid
- RDW:
-
red cell distribution width
- FBG:
-
fasting blood glucose
- TG:
-
triglyceride
- TC:
-
total cholesterol
- HDL-c:
-
high-density lipoprotein cholesterol
- LDL-c:
-
low-density lipoprotein cholesterol
- ALT:
-
alanine aminotransferase
- AST:
-
aspartate aminotransferase
- GGT:
-
gamma glutamyl transferase
- TP:
-
total protein
- ALB:
-
albumin
- ALP:
-
alkaline phosphatase
- aOR:
-
adjusted odds ratio
- CI:
-
confidence interval
- ROC:
-
receiver’s operating characteristics
- AUC:
-
area under the ROC curve
References
Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet (London, England). 2016;387(10017):462–74. https://doi.org/10.1016/s0140-6736(15)00838-7.
Phipps E, Prasanna D, Brima W, Jim B. Preeclampsia: updates in pathogenesis, definitions, and guidelines. Clin J Am Soc Nephrol. 2016;11(6):1102–13. https://doi.org/10.2215/cjn.12081115.
Turpin CA, Sakyi SA, Owiredu WK, Ephraim RK, Anto EO. Association between adverse pregnancy outcome and imbalance in angiogenic regulators and oxidative stress biomarkers in gestational hypertension and preeclampsia. BMC Pregnancy Childbirth. 2015;15:189. https://doi.org/10.1186/s12884-015-0624-y.
Jim B, Karumanchi SA. Preeclampsia: pathogenesis, prevention, and long-term complications. Semin Nephrol. 2017;37(4):386–97. https://doi.org/10.1016/j.semnephrol.2017.05.011.
Sumankuuro J, Crockett J, Wang S. Maternal health care initiatives: causes of morbidities and mortalities in two rural districts of Upper West Region, Ghana. PLoS One. 2017;12(8):e0183644. https://doi.org/10.1371/journal.pone.0183644.
Adua E, Frimpong K, Li X, Wang W. Emerging issues in public health: a perspective on Ghana’s healthcare expenditure, policies and outcomes. EPMA J. 2017;8(3):197–206. https://doi.org/10.1007/s13167-017-0109-3.
Sandesh P, Bruce H, Yadav B, Sharma P. Psychosocial stress during pregnancy and its relation to fetal outcome: a study from Patan Hospital, Lalitpur, Nepal. J Instit Med. 2018;41(2):73–9.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, et al. Medicine in the early twenty-first century: paradigm and anticipation—EPMA position paper 2016. EPMA J. 2016;7:23. https://doi.org/10.1186/s13167-016-0072-4.
Golubnitschaja O, Kinkorova J, Costigliola V. Predictive, preventive and personalised medicine as the hardcore of ‘Horizon 2020’: EPMA position paper. EPMA J. 2014;5(1):6. https://doi.org/10.1186/1878-5085-5-6.
Lemke HU, Golubnitschaja O. Towards personal health care with model-guided medicine: long-term PPPM-related strategies and realisation opportunities within ‘Horizon 2020’. EPMA J. 2014;5(1):8. https://doi.org/10.1186/1878-5085-5-8.
Golubnitschaja O. Time for new guidelines in advanced diabetes care: paradigm change from delayed interventional approach to predictive, preventive & personalized medicine. EPMA J. 2010;1(1):3–12. https://doi.org/10.1007/s13167-010-0014-5.
Yan Y-X, Liu Y-Q, Li M, Hu P-F, Guo A-M, Yang X-H, et al. Development and evaluation of a questionnaire for measuring suboptimal health status in urban Chinese. J Epidemiol. 2009;19(6):333–41.
Wang W, Russell A, Yan Y. Traditional Chinese medicine and new concepts of predictive, preventive and personalized medicine in diagnosis and treatment of suboptimal health. EPMA J. 2014;5(1):4. https://doi.org/10.1186/1878-5085-5-4.
Wang Y, Ge S, Yan Y, Wang A, Zhao Z, Yu X, et al. China suboptimal health cohort study: rationale, design and baseline characteristics. J Transl Med. 2016;14(1):291. https://doi.org/10.1186/s12967-016-1046-y.
Wang W, Yan Y. Suboptimal health: a new health dimension for translational medicine. Clin Transl Med. 2012;1(1):28. https://doi.org/10.1186/2001-1326-1-28.
Ge S, Xu X, Zhang J, Hou H, Wang H, Liu D, et al. Suboptimal health status as an independent risk factor for type 2 diabetes mellitus in a community-based cohort: the China suboptimal health cohort study. EPMA J. 2019;10(1):65–72. https://doi.org/10.1007/s13167-019-0159-9.
Yan YX, Dong J, Liu YQ, Yang XH, Li M, Shia G, et al. Association of suboptimal health status and cardiovascular risk factors in urban Chinese workers. J Urban Health. 2012;89(2):329–38. https://doi.org/10.1007/s11524-011-9636-8.
Wang Y, Liu X, Qiu J, Wang H, Liu D, Zhao Z, et al. Association between ideal cardiovascular health metrics and suboptimal health status in Chinese population. Sci Rep. 2017;7(1):14975. https://doi.org/10.1038/s41598-017-15101-5.
Adua E, Roberts P, Wang W. Incorporation of suboptimal health status as a potential risk assessment for type II diabetes mellitus: a case-control study in a Ghanaian population. EPMA J. 2017;8(4):345–55. https://doi.org/10.1007/s13167-017-0119-1.
Kupaev V, Borisov O, Marutina E, Yan YX, Wang W. Integration of suboptimal health status and endothelial dysfunction as a new aspect for risk evaluation of cardiovascular disease. EPMA J. 2016;7(1):19. https://doi.org/10.1186/s13167-016-0068-0.
Alzain MA, Asweto CO, Zhang J, Fang H, Zhao Z, Guo X, et al. Telomere length and accelerated biological aging in the China suboptimal health cohort: a case-control study. Omics. 2017;21(6):333–9. https://doi.org/10.1089/omi.2017.0050.
Yan YX, Dong J, Liu YQ, Zhang J, Song MS, He Y, et al. Association of suboptimal health status with psychosocial stress, plasma cortisol and mRNA expression of glucocorticoid receptor alpha/beta in lymphocyte. Stress (Amsterdam, Netherlands). 2015;18(1):29–34. https://doi.org/10.3109/10253890.2014.999233.
American College of Obstetricians and Gynecologists, Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122–31. https://doi.org/10.1097/01.aog.0000437382.03963.88.
Malacova E, Regan A, Nassar N, Raynes-Greenow C, Leonard H, Srinivasjois R, et al. Risk of stillbirth, preterm delivery, and fetal growth restriction following exposure in a previous birth: systematic review and meta-analysis. BJOG : Int J Obstet Gynaecol. 2018;125(2):183–92. https://doi.org/10.1111/1471-0528.14906.
Alese MO, Moodley J, Naicker T. Preeclampsia and HELLP syndrome, the role of the liver. J Matern Fetal Neonatal Med. 2019:1–7. https://doi.org/10.1080/14767058.2019.1572737.
Rao S, Jim B. Acute kidney injury in pregnancy: the changing landscape for the 21st century. Kidney Int Rep. 2018;3(2):247–57. https://doi.org/10.1016/j.ekir.2018.01.011.
Nasioudis D, Doulaveris G, Kanninen TT. Dyslipidemia in pregnancy and maternal-fetal outcome. Minerva Ginecol. 2019;71(2):155–62. https://doi.org/10.23736/s0026-4784.18.04330-7.
Laresgoiti-Servitje E. A leading role for the immune system in the pathophysiology of preeclampsia. J Leukoc Biol. 2013;94(2):247–57. https://doi.org/10.1189/jlb.1112603.
LaMarca B, Cornelius DC, Harmon AC, Amaral LM, Cunningham MW, Faulkner JL, et al. Identifying immune mechanisms mediating the hypertension during preeclampsia. Am J Physiol Regul Integr Comp Physiol. 2016;311(1):R1–9. https://doi.org/10.1152/ajpregu.00052.2016.
Kalafat E, Thilaganathan B. Cardiovascular origins of preeclampsia. Curr Opin Obstet Gynecol. 2017;29(6):383–9. https://doi.org/10.1097/gco.0000000000000419.
Perry H, Khalil A, Thilaganathan B. Preeclampsia and the cardiovascular system: an update. Trends Cardiovasc Med. 2018;28(8):505–13. https://doi.org/10.1016/j.tcm.2018.04.009.
Carter W, Bick D, Mackintosh N, Sandall J. A narrative synthesis of factors that affect women speaking up about early warning signs and symptoms of pre-eclampsia and responses of healthcare staff. BMC Pregnancy Childbirth. 2017;17(1):63. https://doi.org/10.1186/s12884-017-1245-4.
Delahaije D, Dirksen C, Peeters L, Smits L. PP105. Mental health problems following preeclampsia or HELLP syndrome: do we have a case? A systematic review. Pregnancy Hypertens. 2012;2(3):296. https://doi.org/10.1016/j.preghy.2012.04.216.
Ephraim RK, Osakunor DN, Denkyira SW, Eshun H, Amoah S, Anto EO. Serum calcium and magnesium levels in women presenting with pre-eclampsia and pregnancy-induced hypertension: a case-control study in the Cape Coast metropolis, Ghana. BMC Pregnancy Childbirth. 2014;14:390. https://doi.org/10.1186/s12884-014-0390-2.
Guo X, Xu L, Huang J, Zhao M. Case-control study on serum calcium and magnesium levels in women presenting with preeclampsia. BMC Pregnancy Childbirth. 2017;20(14):390.
Djagbletey R, Darkwa EO, de Graft-Johnson PK, DAY S, Essuman R, Aryee G, et al. serum calcium and magnesium levels in normal Ghanaian pregnant women: a comparative cross-sectional study. Open Access Macedonian J Med Sci. 2018;6(11):2006–11. https://doi.org/10.3889/oamjms.2018.352.
Anto EO, Owiredu WKBA, Sakyi SA, Turpin CA, Ephraim RKD, Fondjo LA, et al. Adverse pregnancy outcomes and imbalance in angiogenic growth mediators and oxidative stress biomarkers is associated with advanced maternal age births: a prospective cohort study in Ghana. PLoS One. 2018;13(7):e0200581. https://doi.org/10.1371/journal.pone.0200581.
Ephraim R, Doe P, Amoah S, Antoh E. Lipid profile and high maternal body mass index is associated with preeclampsia: a case-control study of the Cape Coast Metropolis. Ann Med Health Sci Res. 2014;4(5):746–50. https://doi.org/10.4103/2141-9248.141542.
Demirci O, Tugrul AS, Dolgun N, Sozen H, Eren S. Serum lipids level assessed in early pregnancy and risk of pre-eclampsia. J Obstet Gynaecol Res. 2011;37(10):1427–32. https://doi.org/10.1111/j.1447-0756.2011.01562.x.
Tangren JS, Wan M, Adnan WAH, Powe CE, Ecker J, Bramham K, et al. Risk of Preeclampsia and Pregnancy Complications in Women With a History of Acute Kidney Injury. Hypertension. 2018;72(2):451–9. https://doi.org/10.1161/hypertensionaha.118.11161.
O’Brien M, Baczyk D, Kingdom JC. Endothelial dysfunction in severe preeclampsia is mediated by soluble factors, rather than extracellular vesicles. Sci Rep. 2017;7(1):5887. https://doi.org/10.1038/s41598-017-06178-z.
Anto EO, Roberts P, Turpin CA, Wang W. Oxidative stress as a key signaling pathway in placental angiogenesis changes in preeclampsia: updates in pathogenesis, novel biomarkers and therapeutics. Curr Pharmacogenomics Pers Med (Formerly Current Pharmacogenomics). 2018;16(3):167–81.
Rondo PH, Ferreira RF, Nogueira F, Ribeiro MC, Lobert H, Artes R. Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. Eur J Clin Nutr. 2003;57(2):266–72. https://doi.org/10.1038/sj.ejcn.1601526.
Valsamakis G, Kanaka-Gantenbein C, Malamitsi-Puchner A, Mastorakos G. Causes of intrauterine growth restriction and the postnatal development of the metabolic syndrome. Ann N Y Acad Sci. 2006;1092:138–47. https://doi.org/10.1196/annals.1365.012.
Gibbins KJ, Silver RM, Pinar H, Reddy UM, Parker CB, Thorsten V, et al. Stillbirth, hypertensive disorders of pregnancy, and placental pathology. Placenta. 2016;43:61–8. https://doi.org/10.1016/j.placenta.2016.04.020.
Prakash J, Ganiger VC, Prakash S, Iqbal M, Kar DP, Singh U, et al. Acute kidney injury in pregnancy with special reference to pregnancy-specific disorders: a hospital based study (2014-2016). J Nephrol. 2018;31(1):79–85. https://doi.org/10.1007/s40620-017-0466-y.
Gallos ID, Sivakumar K, Kilby MD, Coomarasamy A, Thangaratinam S, Vatish M. Pre-eclampsia is associated with, and preceded by, hypertriglyceridaemia: a meta-analysis. BJOG. 2013;120(11):1321–32. https://doi.org/10.1111/1471-0528.12375.
Liu D, Chu X, Wang H, Dong J, Ge SQ, Zhao ZY, et al. The changes of immunoglobulin G N-glycosylation in blood lipids and dyslipidaemia. J Transl Med. 2018;16(1):235. https://doi.org/10.1186/s12967-018-1616-2.
Acknowledgements
We wish to thank the biomedical staff of the Department of Biochemistry and Serology, and midwives of the Department of Obstetrics and Gynaecology of the Komfo Anokye Teaching Hospital, Ghana, for their support during the participant’s recruitment and biological sample processing. We also thank the research assistants of the Department of Molecular Medicine, Kwame Nkrumah University of Science and Technology for their support during the biological sample analysis. We finally thank the American Association of Clinical Chemistry (AACC) Academy Research Fellows for selecting our abstract coined from the present study entitled, ‘Algorithm of Suboptimal Health Status, Serum Magnesium and Calcium Levels as a Novel Approach for Prediction and Identification of Pregnant Women Likely to Develop Preeclampsia and Adverse Perinatal Complications in a Ghanaian Population’ for Scientific Excellence in Maternal and Foetal Medicine and AACC Academy’s Distinguished Abstract Award at the 71st AACC Scientific Annual Meeting, Anaheim, CA.
Funding
This work was supported by the Australia-China International Collaborative Grant (NHMRC-APP1112767-NSFC81561120) and Edith Cowan University (ECU)-Collaborative Enhancement Scheme Round 1 (G1003363). Enoch Odame Anto was supported by ECU-International Postgraduate Research Scholarship.
Author information
Authors and Affiliations
Contributions
EOA, PR, DC and WW conceived the study. EOA and CAT performed the investigation and collected the data. EOA performed the statistical analysis. EOA, PR, DC, EA, YW and WW wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for publication
Not applicable.
Ethical approval and consent to participate
Approval for this study was obtained from the Committee on Human Research Publication and Ethics (CHRPE) of the School of Medical Science (SMS) /KNUST and Komfo Anokye Teaching Hospital (KATH) (CHRPE/AP/146/17) and the Human Research Ethics Committee of Edith Cowan University (ECU) (17509). This study was conducted in accordance with the guidelines of the Helsinki Declaration. Written informed consent in the form of a signature and fingerprint was obtained from all participants and legally authorized representatives after the protocol of the study was explained to them in plain English language and native Ghanaian language where appropriate.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anto, E.O., Roberts, P., Coall, D. et al. Integration of suboptimal health status evaluation as a criterion for prediction of preeclampsia is strongly recommended for healthcare management in pregnancy: a prospective cohort study in a Ghanaian population. EPMA Journal 10, 211–226 (2019). https://doi.org/10.1007/s13167-019-00183-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-019-00183-0