Abstract
Background:
Nowadays, biological tissue engineering is a growing field of research. Biocompatibility is a key indicator for measuring tissue engineering biomaterials, which is of great significance for the replacement and repair of damaged tissues.
Methods:
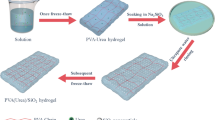
In this study, using gelatin, carboxymethyl chitosan, and sodium alginate, a tissue engineering material scaffold that can carry cells was successfully prepared. The material was characterized by Fourier transforms infrared spectroscopy. In addition, the prepared scaffolds have physicochemical properties, such as swelling ratio, biodegradability. we observed the biocompatibility of the hydrogel to different adult stem cells (BMSCs and ADSCs) in vivo and in vitro. Adult stem cells were planted on gelatin-carboxymethyl chitosan-sodium alginate (Gel/SA/CMCS) hydrogels for 7 days in vitro, and the survival of stem cells in vitro was observed by live/died staining. Gel/SA/CMCS hydrogels loaded with stem cells were subcutaneously transplanted into nude mice for 14 days of in vivo culture observation. The survival of adult stem cells was observed by staining for stem cell surface markers (CD29, CD90) and Ki67.
Results:
The scaffolds had a microporous structure with an appropriate pore size (about 80 μm). Live/died staining showed that adult stem cells could stably survive in Gel/SA/CMCS hydrogels for at least 7 days. After 14 days of culture in nude mice, Ki67 staining showed that the stem cells supported by Gel/SA/CMCS hydrogel still had high proliferation activity.
Conclusion:
Gel/SA/CMCSs hydrogel has a stable interpenetrating porous structure, suitable swelling performance and degradation rate, can promote and support the survival of adult stem cells in vivo and in vitro, and has good biocompatibility. Therefore, Gel/SA/CMCS hydrogel is a strong candidate for biological tissue engineering materials.
Graphical Abstract











Similar content being viewed by others
References
Zurina IM, Presniakova VS, Butnaru DV, Svistunov AA, Timashev PS, Rochev YA. Tissue engineering using a combined cell sheet technology and scaffolding approach. Acta Biomater. 2020;113:63–83.
Berthiaume F, Maguire TJ, Yarmush ML. Tissue engineering and regenerative medicine: history, progress, and challenges. Annu Rev Chem Biomol Eng. 2011;2:403–30.
Wang Y, Kim HJ, Vunjak-Novakovic G, Kaplan DL. Stem cell-based tissue engineering with silk biomaterials. Biomaterials. 2006;27:6064–82.
He Y, Zhao W, Dong Z, Ji Y, Li M, Hao Y, et al. A biodegradable antibacterial alginate/carboxymethyl chitosan/Kangfuxin sponges for promoting blood coagulation and full-thickness wound healing. Int J Biol Macromol. 2021;167:182–92.
Huang J, Fu H, Wang Z, Meng Q, Liu S, Wang H, et al. BMSCs-laden gelatin/sodium alginate/carboxymethyl chitosan hydrogel for 3D bioprinting. RSC Adv. 2016;6:108423–30.
Ansari S, Diniz IM, Chen C, Sarrion P, Tamayol A, Wu BM, et al. Human periodontal ligament- and gingiva-derived mesenchymal stem cells promote nerve regeneration when encapsulated in alginate/hyaluronic acid 3D scaffold. Adv Healthc Mater. 2017;6:1700670.
He Y, Li Y, Sun Y, Zhao S, Feng M, Xu G, et al. A double-network polysaccharide-based composite hydrogel for skin wound healing. Carbohydr Polym. 2021;261:117870.
Yang X, Yang H, Jiang X, Yang B, Zhu K, Lai NC, et al. Injectable chitin hydrogels with self-healing property and biodegradability as stem cell carriers. Carbohydr Polym. 2021;256:117574.
Liu X, Hao M, Chen Z, Zhang T, Huang J, Dai J, et al. 3D bioprinted neural tissue constructs for spinal cord injury repair. Biomaterials. 2021;272:120771.
Hassanzadeh P, Atyabi F, Dinarvand R. Tissue engineering: Still facing a long way ahead. J Control Release. 2018;279:181–97.
Shafiee A, Atala A. Tissue engineering: Toward a new era of medicine. Annu Rev Med. 2017;68:29–40.
Gu Z, Huang K, Luo Y, Zhang L, Kuang T, Chen Z, et al. Double network hydrogel for tissue engineering. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2018;10:e1520.
Long Y, Yan L, Dai H, Yang D, Wu X, Dong X, et al. Enhanced proliferation and differentiation of neural stem cells by peptide-containing temperature-sensitive hydrogel scaffold. Mater Sci Eng C Mater Biol Appl. 2020;116:111258.
Bakhshandeh B, Zarrintaj P, Oftadeh MO, Keramati F, Fouladiha H, Sohrabi-Jahromi S, et al. Tissue engineering; strategies, tissues, and biomaterials. Biotechnol Genet Eng Rev. 2017;33:144–72.
Huang GY, Zhou LH, Zhang QC, Chen YM, Sun W, Xu F, et al. Microfluidic hydrogels for tissue engineering. Biofabrication. 2011;3:012001.
Hu Y, Dan W, Xiong S, Kang Y, Dhinakar A, Wu J, et al. Development of collagen/polydopamine complexed matrix as mechanically enhanced and highly biocompatible semi-natural tissue engineering scaffold. Acta Biomater. 2017;47:135–48.
Basu A, Kunduru KR, Abtew E, Domb AJ. Polysaccharide-Based Conjugates for Biomedical Applications. Bioconjug Chem. 2015;26:1396–412.
Varaprasad K, Jayaramudu T, Kanikireddy V, Toro C, Sadiku ER. Alginate-based composite materials for wound dressing application: A mini review. Carbohydr Polym. 2020;236:116025.
Wang YL, Zhou YN, Li XY, Huang J, Wahid F, Zhong C. Continuous production of antibacterial carboxymethyl chitosan-zinc supramolecular hydrogel fiber using a double-syringe injection device. Int J Biol Macromol. 2020;156:252–61.
Wang D, Zhang N, Meng G, He J, Wu F. The effect of form of carboxymethyl-chitosan dressings on biological properties in wound healing. Colloids Surf B Biointerfaces. 2020;194:111191.
Yan T, Hui W, Zhu S, He J, Liu Z, Cheng J. Carboxymethyl chitosan based redox-responsive micelle for near-infrared fluorescence image-guided photo-chemotherapy of liver cancer. Carbohydr Polym. 2021;253:117284.
Jiang Z, Wang S, Hou J, Chi J, Wang S, Shao K, et al. Effects of carboxymethyl chitosan oligosaccharide on regulating immunologic function and inhibiting tumor growth. Carbohydr Polym. 2020;250:116994.
Aljohani W, Ullah MW, Zhang X, Yang G. Bioprinting and its applications in tissue engineering and regenerative medicine. Int J Biol Macromol. 2018;107:261–75.
Vorwald CE, Gonzalez-Fernandez T, Joshee S, Sikorski P, Leach JK. Tunable fibrin-alginate interpenetrating network hydrogels to support cell spreading and network formation. Acta Biomater. 2020;108:142–52.
Liu Q, Wang J, Chen Y, Zhang Z, Saunders L, Schipani E, et al. Suppressing mesenchymal stem cell hypertrophy and endochondral ossification in 3D cartilage regeneration with nanofibrous poly(l-lactic acid) scaffold and matrilin-3. Acta Biomater. 2018;76:29–38.
Teekakirikul P, Zhu W, Huang HC, Fung E. Hypertrophic cardiomyopathy: An overview of genetics and management. Biomolecules. 2019;9:878.
Craciun AM, Mititelu Tartau L, Pinteala M, Marin L. Nitrosalicyl-imine-chitosan hydrogels based drug delivery systems for long term sustained release in local therapy. J Colloid Interface Sci. 2019;536:196–207.
Echave MC, Saenz delBurgo L, Pedraz JL, Orive G. Gelatin as biomaterial for tissue engineering. Curr Pharm Des. 2017;23:3567–84.
Wang S, Guan S, Li W, Ge D, Xu J, Sun C, et al. 3D culture of neural stem cells within conductive PEDOT layer-assembled chitosan/gelatin scaffolds for neural tissue engineering. Mater Sci Eng C Mater Biol Appl. 2018;93:890–901.
Cheng Y, Hu Z, Zhao Y, Zou Z, Lu S, Zhang B, et al. Sponges of carboxymethyl chitosan grafted with collagen peptides for wound healing. Int J Mol Sci. 2019;20:3890.
Yu H, Zhang X, Song W, Pan T, Wang H, Ning T, et al. Effects of 3-dimensional bioprinting alginate/gelatin hydrogel scaffold extract on proliferation and differentiation of human dental pulp stem cells. J Endod. 2019;45:706–15.
Wang J, Zhou L, Sun Q, Cai H, Tan WS. Porous chitosan derivative scaffolds affect proliferation and osteogenesis of mesenchymal stem cell via reducing intracellular ROS. Carbohydr Polym. 2020;237:116108.
Wang K, Nune KC, Misra RD. The functional response of alginate-gelatin-nanocrystalline cellulose injectable hydrogels toward delivery of cells and bioactive molecules. Acta Biomater. 2016;36:143–51.
An S, Ling J, Gao Y, Xiao Y. Effects of varied ionic calcium and phosphate on the proliferation, osteogenic differentiation and mineralization of human periodontal ligament cells in vitro. J Periodontal Res. 2012;47:374–82.
Zimet P, Mombru AW, Mombru D, Castro A, Villanueva JP, Pardo H, Rufo C. Physico-chemical and antilisterial properties of nisin-incorporated chitosan/carboxymethyl chitosan films. Carbohydr Polym. 2019;219:334–43.
Shariatinia Z. Carboxymethyl chitosan: Properties and biomedical applications. Int J Biol Macromol. 2018;120:1406–19.
Wahid F, Yin JJ, Xue DD, Xue H, Lu YS, Zhong C, et al. Synthesis and characterization of antibacterial carboxymethyl Chitosan/ZnO nanocomposite hydrogels. Int J Biol Macromol. 2016;88:273–9.
Zhao X, Li P, Guo B, Ma PX. Antibacterial and conductive injectable hydrogels based on quaternized chitosan-graft-polyaniline/oxidized dextran for tissue engineering. Acta Biomater. 2015;26:236–48.
Periayah MH, Halim AS, Mat Saad AZ. Mechanism action of platelets and crucial blood coagulation pathways in hemostasis. Int J Hematol Oncol Stem Cell Res. 2017;11:319–27.
Bakshi PS, Selvakumar D, Kadirvelu K, Kumar NS. Chitosan as an environment friendly biomaterial - a review on recent modifications and applications. Int J Biol Macromol. 2020;150:1072–83.
Chen Y, Wu L, Li P, Hao X, Yang X, Xi G, et al. Polysaccharide based hemostatic strategy for ultrarapid hemostasis. Macromol Biosci. 2020;20:e1900370.
Liu Y, Sui Y, Liu C, Liu C, Wu M, Li B, et al. A physically crosslinked polydopamine/nanocellulose hydrogel as potential versatile vehicles for drug delivery and wound healing. Carbohydr Polym. 2018;188:27–36.
Li S, Dong S, Xu W, Tu S, Yan L, Zhao C, et al. Antibacterial hydrogels. Adv Sci (Weinh). 2018;5:1700527.
Mao C, Xiang Y, Liu X, Cui Z, Yang X, Li Z, et al. Repeatable photodynamic therapy with triggered signaling pathways of fibroblast cell proliferation and differentiation to promote bacteria-accompanied wound healing. ACS Nano. 2018;12:1747–59.
Acknowledgements
This work was supported by Shandong Provincial Natural Science Foundation of China (No. ZR2020MH070 and No. ZR2020MH078), Shandong Province Medicine and Health Science and Technology Development Plan Project (No. 2019WS368), and Research Support Foundation of Jining Medical University (No. JYFC2018FKJ009 and No. JYFC2018KJ004). Xinzhe Wang: Methodology, Investigation, Formal analysis, Writing-original draft. Siqi Li: Investigation, Data curation. Honglian Yu: Conceptualization, Formal analysis, Writing-review & editing, Supervision, Project administration. Jianzhi Lv: Validation, Data curation. Minglun Fan: Investigation. Ximing Wang: Validation. Xin Wang: Validation. Yanting Liang: Validation. Lingna Mao: Validation. Zhankui Zhao: Supervision, Writing—review & editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflicts of interest.
Ethical statement
All animal experiments were conducted in the Central Laboratory of Affiliated Hospital of Jining Medical University, according to the guidelines of the Institutional Animal Care and Use Committee and the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, X., Li, S., Yu, H. et al. The Biocompatibility of Multi-Source Stem Cells and Gelatin-Carboxymethyl Chitosan-Sodium Alginate Hybrid Biomaterials. Tissue Eng Regen Med 19, 491–503 (2022). https://doi.org/10.1007/s13770-021-00429-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13770-021-00429-x