Abstract
Background:
Tissue defects in the annulus fibrosus (AF) due to intervertebral disc (IVD) degeneration or after nucleodiscectomy have little self-healing capacity. To prevent progressive degeneration of the IVD, the AF must be repaired. Biological closure has not yet been achieved and is a challenge for the research community. In this study, a scaffold made of absorbable poly (glycolic acid) (PGA) and hyaluronan (HA) that exhibit excellent biocompatibility and cell colonization properties was used to repair AF defects in an ovine model.
Methods:
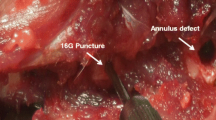
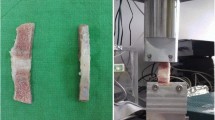
A partial resection was performed in AF in L3/4 or L4/5 of 10 sheep and PGA-HA scaffolds were implanted on the defects (n = 5), while defects in the control group were left untreated (n = 5). Three months post-operation, the lumbar discs were sectioned and stained with hematoxylin and eosin and safranin-O/fast-green. Histological features including proteoglycan content, annular structure, cellular morphology, blood vessel ingrowth and tear/cleft formation were scored using a modified scoring scheme by 3 investigators and evaluated by a pathologist independently.
Results:
The treated AF exhibited significantly enhanced repair tissue structure with signs of proteoglycan formation compared to the untreated group. The median scores were 4.3 for the treated and 9.8 for the untreated group. Cystic degeneration, perivascular infiltration, inflammation and necrosis were only present in the untreated group. Blood vessel ingrowth and tear/cleft formation were increased, though not significant, in the untreated group while cell morphology was comparable in both groups.
Conclusion:
PGA-HA scaffolds used for AF closure support repair tissue formation in an ovine lumbar disc defect model.






Similar content being viewed by others
References
Harmon MD, Ramos DM, Nithyadevi D, Bordett R, Rudraiah S, Nukavarapu SP, et al. Growing a backbone - functional biomaterials and structures for intervertebral disc (IVD) repair and regeneration: challenges, innovations, and future directions. Biomater Sci. 2020;8:1216–39.
Shu CC, Smith MM, Smith SM, Dart AJ, Little CB, Melrose J. A histopathological scheme for the quantitative scoring of intervertebral disc degeneration and the therapeutic utility of adult mesenchymal stem cells for intervertebral disc regeneration. Int J Mol Sci. 2017;18:1049.
Cabraja M, Endres M, Hegewald AA, Vetterlein S, Thomé C, Woiciechowsky C, et al. A 3D environment for anulus fibrosus regeneration. J Neurosurg Spine. 2012;17:177–83.
Sharifi S, Bulstra SK, Grijpma DW, Kuijer R. Treatment of the degenerated intervertebral disc; closure, repair and regeneration of the annulus fibrosus. J Tissue Eng Regen Med. 2015;9:1120–32.
Tavakoli J, Diwan AD, Tipper JL. Advanced strategies for the regeneration of lumbar disc annulus fibrosus. Int J Mol Sci. 2020;21:4889.
Alini M, Li W, Markovic P, Aebi M, Spiro RC, Roughley PJ. The potential and limitations of a cell-seeded collagen/hyaluronan scaffold to engineer an intervertebral disc-like matrix. Spine (Phila Pa 1976). 2003;28:446–53.
Park SH, Gil ES, Cho H, Mandal BB, Tien LW, Min BH, et al. Intervertebral disk tissue engineering using biphasic silk composite scaffolds. Tissue Eng Part A. 2012;18:447–58.
Shao X, Hunter CJ. Developing an alginate/chitosan hybrid fiber scaffold for annulus fibrosus cells. J Biomed Mater Res A. 2007;82:701–10.
Shen B, Wei A, Bhargav D, Kishen T, Diwan AD. Hyaluronan: its potential application in intervertebral disc regeneration. Orthop Res Rev. 2010;2:17–26.
Chou AI, Reza AT, Nicoll SB. Distinct intervertebral disc cell populations adopt similar phenotypes in three-dimensional culture. Tissue Eng Part A. 2008;14:2079–87.
Koepsell L, Remund T, Bao J, Neufeld D, Fong H, Deng Y. Tissue engineering of annulus fibrosus using electrospun fibrous scaffolds with aligned polycaprolactone fibers. J Biomed Mater Res Part A. 2011;99:564–75.
Lei Z, Song Z, Bao-chang C. Actuality and challenge of biomaterials in annulus fibrosus repair. Chin J Tissue Eng Res. 2018;22:958–63.
Moran JM, Pazzano D, Bonassar LJ. Characterization of polylactic acid–polyglycolic acid composites for cartilage tissue engineering. Tissue Eng. 2003;9:63–70.
Abbushi A, Endres M, Cabraja M, Kroppenstedt SN, Thomale UW, Sittinger M, et al. Regeneration of intervertebral disc tissue by resorbable cell-free polyglycolic acid-based implants in a rabbit model of disc degeneration. Spine (Phila Pa 1976). 2008;33:1527–32.
Endres M, Abbushi A, Thomale UW, Cabraja M, Kroppenstedt SN, Morawietz L, et al. Intervertebral disc regeneration after implantation of a cell-free bioresorbable implant in a rabbit disc degeneration model. Biomaterials. 2010;31:5836–41.
Hegewald AA, Medved F, Feng D, Tsagogiorgas C, Beierfuß A, Schindler GAK, et al. Enhancing tissue repair in annulus fibrosus defects of the intervertebral disc: analysis of a bio-integrative annulus implant in an in-vivo ovine model. J Tissue Eng Regen Med. 2015;9:405–14.
Hegewald AA, Enz A, Endres M, Sittinger M, Woiciechowsky C, Thomé C, et al. Engineering of polymer-based grafts with cells derived from human nucleus pulposus tissue of the lumbar spine. J Tissue Eng Regen Med. 2011;5:275–82.
Siclari A, Mascaro G, Kaps C, Boux E. A 5-year follow-up after cartilage repair in the knee using a platelet-rich plasma-immersed polymer-based implant. Open Orthop J. 2014;8:346–54.
Bergmanna A, Hans Peter Abt. 7 months clinical follow-up after arthrotomic implantation of chondrotissue in a cartilage lesion of the lateral talus. Fuß & Sprunggelenk. 2009;8:264–7.
Woiciechowsky C, Abbushi A, Zenclussen ML, Casalis P, Krüger JP, Freymann U, et al. Regeneration of nucleus pulposus tissue in an ovine intervertebral disc degeneration model by cell-free resorbable polymer scaffolds. J Tissue Eng Regen Med. 2014;8:811–20.
Hondke S, Cabraja M, Krüger JP, Stich S, Hartwig T, Sittinger M, et al. Proliferation, migration, and ECM formation potential of human annulus fibrosus cells is independent of degeneration status. Cartilage. 2020;11:192–202.
Boos N, Weissbach S, Rohrbach H, Weiler C, Spratt KF, Nerlich AG. Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo Award in basic science. Spine (Phila Pa 1976). 2002;27:2631–44.
Rutges JP, Duit RA, Kummer JA, Bekkers JE, Oner FC, Castelein RM, et al. A validated new histological classification for intervertebral disc degeneration. Osteoarthritis Cartilage. 2013;21:2039–47.
Ostach PKS. Model for the implantation of implants stimulating the body’s own mechanisms for repair and regeneration of ovine annulus fibrosus defects. [Doctoral dissertation]. Free University Berlin; 2019.
Koo TK, Li MY. Cracking the code: providing insight into the fundamentals of research and evidence-based practice a guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63.
Lee SH, Kim BS, Kim SH, Choi SW, Jeong SI, Kwon IK, et al. Elastic biodegradable poly(glycolide-co-caprolactone) scaffold for tissue engineering. J Biomed Mater Res A. 2003;66:29–37.
Lyons G, Eisenstein SM, Sweet MB. Biochemical changes in intervertebral disc degeneration. Biochim Biophys Acta. 1981;673:443–53.
Papakonstantinou E, Roth M, Karakiulakis G. Hyaluronic acid: A key molecule in skin aging. Dermatoendocrinol. 2012;4:253–8.
Urban JP, Smith S, Fairbank JC. Nutrition of the Intervertebral disc. Spine (Phila Pa 1976). 2004;29:2700–9.
Sharp CA, Roberts S, Evans H, Brown SJ. Disc cell clusters in pathological human intervertebral discs are associated with increased stress protein immunostaining. Eur Spine J. 2009;18:1587–94.
Melrose J, Roberts S, Smith S, Menage J, Ghosh P. Increased nerve and blood vessel ingrowth associated with proteoglycan depletion in an ovine anular lesion model of experimental disc degeneration. Spine (Phila Pa 1976). 2002;27:1278–85.
Melrose J. Repair of annular disc lesions: spatial and temporal localisation of TGF-beta, SPARC (osteonectin/BM-40) and FGF-2 are early responses in experimentally injured ovine discs. Trans Orthop Res Soc. 2001;26:896.
Sartoretto SC, Uzeda MJ, Miguel FB, Nascimento JR, Ascoli F, Calasans-Maia MD. Sheep as an experimental model for biomaterial implant evaluation. Acta Ortop Bras. 2016;24:262–6.
Smit TH. The use of a quadruped as an in vivo model for the study of the spine - biomechanical considerations. Eur Spine J. 2002;11:137–44.
Bailey AS, Adler F, Min Lai S, Asher MA. A comparison between bipedal and quadrupedal rats: do bipedal rats actually assume an upright posture? Spine (Phila Pa 1976). 2001;26:308–13.
Alini M, Eisenstein SM, Ito K, Little C, Kettler AA, Masuda K, et al. Are animal models useful for studying human disc disorders/degeneration? Eur Spine J. 2008;17:2–19.
Bouhsina N, Decante C, Hardel J, B, Madec S, Abadie J, Hamel A, et al. Correlation between magnetic resonance, X-ray imaging alterations and histological changes in an ovine model of age-related disc degeneration. Eur Cells Mater. 2021;42:166–78.
Kruger JP, Ketzmar AK, Endres M, Pruss A, Siclari A, Kaps C. Human platelet-rich plasma induces chondrogenic differentiation of subchondral progenitor cells in polyglycolic acid-hyaluronan scaffolds. J Biomed Mater Res Part B Appl Biomater. 2014;102:681–92.
Yang D, Lu X, Hong Y, Xi T, Zhang D. The molecular mechanism of mediation of adsorbed serum proteins to endothelial cells adhesion and growth on biomaterials. Biomaterials. 2013;34:5747–58.
Wilson CJ, Clegg RE, Leavesley DI, Pearcy MJ. Mediation of biomaterial-cell interactions by adsorbed proteins: a review. Tissue Eng. 2005;11:1–18.
Allen LT, Tosetto M, Miller IS, O’Connor DP, Penney SC, Lynch I, et al. Surface-induced changes in protein adsorption and implications for cellular phenotypic responses to surface interaction. Biomaterials. 2006;27:3096–108.
Kalwitz G, Andreas K, Endres M, Neumann K, Notter M, Ringe J, et al. Chemokine profile of human serum from whole blood: migratory effects of CXCL-10 and CXCL-11 on human mesenchymal stem cells. Connect Tissue Res. 2010;51:113–22.
Hegewald AA, Knecht S, Baumgartner D, Gerber H, Endres M, Kaps C, et al. Biomechanical testing of a polymer-based biomaterial for the restoration of spinal stability after nucleotomy. J Orthop Surg Res. 2009;4:25.
Acknowledgements
The authors thank Dr. Katja Reiter, Dr. Pia Ostach and Prof. Dr. Christian Große-Siestrup for animal surgery. We also like to thank the Research facilities for experimental medicine (FEM) and the animal holding unit of the Charité-Universitaetsmedizin Berlin for animal care. Grateful thanks to Samuel Vetterlein and Anja Wachtel for technical support of sample preparation and histochemical staining. The research leading to these results received funding from Federal Ministry of Education and Research (BMBF) grant no. 13N13435 and 13N13437.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MRSF, JPK, PB and ME are employees of the research company TransTissue Technologies GmbH and receive salaries from the company. All other declare no conflict of interest.
Ethical statement
All procedures performed in this study involving animals were approved by the State Office for Health and Social Affairs in Berlin, Germany (LaGeSo No. G 0093/16). The study was performed under German Animal Welfare Act (§ 8.1 and § 7.2).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saghari Fard, M.R., Krueger, J.P., Stich, S. et al. A Biodegradable Polymeric Matrix for the Repair of Annulus Fibrosus Defects in Intervertebral Discs. Tissue Eng Regen Med 19, 1311–1320 (2022). https://doi.org/10.1007/s13770-022-00466-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13770-022-00466-0