Abstract
Background and Objectives
The efficacy of direct oral anticoagulants (DOACs) in the management of left ventricular (LV) thrombi remains to be determined, especially in patients with ischemic cardiomyopathy. This retrospective study sought to compare the efficacy of vitamin K antagonists (VKAs) and DOACs in patients with LV thrombi and evaluate the rate of LV thrombus resolution after adjusting anticoagulation.
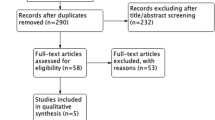
Methods
This observational retrospective study included patients admitted to our institution for LV thrombus between January 2010 and August 2019. The rate of LV thrombus resolution was compared between VKAs and DOACs. Patients without thrombus resolution with DOAC treatment were switched to VKA agents in order to obtain an international normalized ratio (INR) of 3–4.
Results
Between January 2010 and August 2019, 59 consecutive patients with LV thrombi detected by transthoracic echocardiography were included in the study. The mean age was 62 ± 14 years and 16.9% were women. The circumstances of LV thrombus discovery were as follows: acute myocardial infarction or ischemic myocardiopathy (n = 22), stroke (n = 6), chest pain (n = 7), heart failure (n = 11), transthoracic echocardiographic evaluation (n = 11), and ventricular arrhythmias (n = 2). The proportion of patients on DOACs was 28.8% (n = 17), while that of those on VKAs was 71.2% (n = 42). Thrombus resolution was obtained in 70.6% (12/17) of patients on DOACs and in 71.4% (30/42) of those on VKAs (p = 0.9). Patients who failed to respond to DOAC treatment were treated with VKAs, and following this treatment adjustment all LV thrombi were dissolved in the DOAC group (5/5). Five embolic events (8.4% of stroke) occurred before the treatment initiation and six with anticoagulants (2/17 with DOACs [11.8%] and 4/42 with VKAs [9.5%]; p = 0.8).
Conclusions
This retrospective observational study found a similar efficacy between DOAC and VKA agents in patients with LV thrombi (70.6% vs. 71.5%); however, when the thrombus remains, VKAs are still the standard of care as it is possible to control INR levels (3–4) with them.
Similar content being viewed by others
References
Solheim S, Seljeflot I, Lunde K, et al. Frequency of left ventricular thrombus in patients with anterior wall acute myocardial infarction treated with percutaneous coronary intervention and dual antiplatelet therapy. Am J Cardiol. 2010;106:1197–200.
Mao TF, Bajwa A, Muskula P, et al. Incidence of left ventricular thrombus in patients with acute ST-segment elevation myocardial infarction treated with percutaneous coronary intervention. Am J Cardiol. 2018;121(1):27–31.
Kupper AJ, Verheugt FW, Peels CH, Galema TW, Roos JP. Left ventricular thrombus incidence and behavior studied by serial two-dimensional echocardiography in acute anterior myocardial infarction: left ventricular wall motion, systemic embolism and oral anticoagulation. J Am Coll Cardiol. 1989;13:1514–20.
Gianstefani S, Douiri A, Delithanasis I, et al. Incidence and predictors of early left ventricular thrombus after ST-elevation myocardial infarction in the contemporary era of primary percutaneous coronary intervention. Am J Cardiol. 2014;113(7):1111–6.
Robinson AA, Jain A, Gentry M, McNamara RL. Left ventricular thrombi after STEMI in the primary PCI era: a systematic review and meta-analysis. Int J Cardiol. 2016;221:554–9.
Maniwa N, Fujino M, Nakai M, et al. Anticoagulation combined with antiplatelet therapy in patients with left ventricular thrombus after first acute myocardial infarction. Eur Heart J. 2018;39(3):201–8.
Vaitkus PT, Barnathan ES. Embolic potential, prevention and management of mural thrombus complicating anterior myocardial infarction: a meta-analysis. J Am Coll Cardiol. 1993;22(4):1004–9.
Steg PG, James SK, Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology (ESC), et al. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33(20):2569–619.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the Management of Acute Myocardial Infarction in Patients Presenting with ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–77.
Guyatt GH, Akl EA, Crowther M, Gutterman DD, Schuünemann HJ, American College of Chest Physicians Antithrombotic Therapy and Prevention of Thrombosis Panel. Executive summary: antithrombotic therapy and prevention of thrombosis, 9th edn: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 suppl):7S–47S.
Heidbuchel H, Verhamme P, Alings M, et al. European Heart Rhythm Association practical guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation. Europace. 2013;15(5):625–51.
Aydin F, Turgay Yildirim O, Huseyinoglu Aydin A, Dagtekin E, Aksit E. Is rivaroxaban a safe choice for apical thrombus in atrial fibrillation patients? A case report. J Stroke Cerebrovasc Dis. 2018;27(9):e203–5.
Noflatscher M, Moes N, Gassner EM, Marschang P. Dabigatran added to dual antiplatelet therapy to treat a left ventricular thrombus in an 87 year old patient with myocardial infarction and very high bleeding risk. Front Pharmacol. 2018;4(9):217.
Elikowski W, Małek-Elikowska M, Fertała N, Zawodna M, Kruzel K. Fast apixaban-related resolution of left ventricular thrombi in a patient with dilated cardiomyopathy. Pol Merkur Lekarski. 2018;44(259):19–22.
Sun H, Zhao Q, Wang Y, et al. Daily 10 mg rivaroxaban as a therapy for ventricular thrombus related to left ventricular non-compaction cardiomyopathy: a case report. Medicine (Baltimore). 2018;97(4):e9670.
Adar A, Onalan O, Cakan F. Newly developed left ventricular apical thrombus under dabigatran treatment. Blood Coagul Fibrinol. 2018;29(1):126–8.
Smetana KS, Dunne J, Parrott K, et al. Oral factor Xa inhibitors for the treatment of left ventricular thrombus: a case series. J Thromb Thromb. 2017;44(4):519–24.
Seecheran R, Seecheran V, Persad S, Seecheran NA. Rivaroxaban as an antithrombotic agent in a patient with ST-segment elevation myocardial and left ventricular thrombus: a case report. J Investig Med High Impact Case Rep. 2017;5(1):2324709617697991.
Elikowski W, Małek-Elikowska M, Słomczyński M, Ganowicz-Kaatz T, Bolewski A, Skrzywanek P. Rivaroxaban-resistant right ventricular thrombus, successfully treated with vitamin K antagonist in a patient with dilated cardiomyopathy. Pol Merkur Lekarski. 2016;41(245):238–42.
Makrides CA. Resolution of left ventricular postinfarction thrombi in patients undergoing percutaneous coronary intervention using rivaroxaban in addition to dual antiplatelet therapy. BMJ Case Rep. 2016;2016:bcr2016217843.
Kaya A, Hayıroğlu Mİ, Keskin M, Tekkeşin Aİ, Alper AT. Resolution of left ventricular thrombus with apixaban in a patient with hypertrophic cardiomyopathy. Turk Kardiyol Dern Ars. 2016;44(4):335–7.
Kolekar S, Munjewar C, Sharma S. Dabigatran for left ventricular thrombus. Indian Heart J. 2015;67(5):495–6.
Ohashi N, Okada T, Uchida M, Amioka M, Fujiwara M, Kaseda S. effects of dabigatran on the resolution of left ventricular thrombus after acute myocardial infarction. Intern Med. 2015;54(14):1761–3.
Mano Y, Koide K, Sukegawa H, Kodaira M, Ohki T. Successful resolution of a left ventricular thrombus with apixaban treatment following acute myocardial infarction. Heart Vessels. 2016;31(1):118–23.
Padilla Pérez M, Salas Bravo D, Garcelán Trigo JA, et al. Resolution of left ventricular thrombus by rivaroxaban. Future Cardiol. 2014;10(3):333–6.
Nagamoto Y, Shiomi T, Matsuura T, et al. Resolution of a left ventricular thrombus by the thrombolytic action of dabigatran. Heart Vessels. 2014;29(4):560–2.
Kaku B. Intra-cardiac thrombus resolution after anti-coagulation therapy with dabigatran in a patient with mid-ventricular obstructive hypertrophic cardiomyopathy: a case report. J Med Case Rep. 2013;7:238.
Chung K, Paek YM, Lee HJ, Hong K-S. Dabigatran effect on left ventricular thrombus in a patient with acute ischemic stroke. J Stroke. 2015;17(3):366–8.
Nakasuka K, Ito S, Noda T, et al. Resolution of left ventricular thrombus secondary to tachycardia-induced heart failure with rivaroxaban. Case Rep Med. 2014;2014:814524.
Cross P, Stewart R. Left ventricular mural thrombus treated with dabigatran. J Case Rep Stud. 2014;2(4):402.
Berry A, Brancheau D, Zughaib M. Rapid resolution of left ventricular thrombus with apixaban therapy. SAGE Open Med Case Rep. 2017;5:2050313X17745211.
Abubakar H, Yassin AS, Shokr M. Rivaroxaban used for treatment of a left ventricular thrombus in a patient with nonischemic cardiomyopathy. Am J Ther. 2018;25(6):e706–9.
Da Costa A, Delolme C, Guichard JB, et al. Comparison of prevalence and management of left atrial appendage thrombi under old and new anticoagulants prior to left atrial catheter ablation. Am Heart J. 2017;193:8–15.
Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1–39.
Weinsaft JW, Kim HW, Crowley AL, et al. LV thrombus detection by routine echocardiography: insights into performance characteristics using delayed enhancement CMR. JACC Cardiovasc Imaging. 2011;4(7):702–12.
Pöss J, Desch S, Eitel C, de Waha S, Thiele H, Eitel I. Left ventricular thrombus formation after ST-segment-elevation myocardial infarction: insights from a cardiac magnetic resonance multicenter study. Circ Cardiovasc Imaging. 2015;8(10):e003417.
Phan J, Nguyen T, French J, et al. Incidence and predictors of left ventricular thrombus formation following acute ST-segment elevation myocardial infarction: a serial cardiac MRI study. Int J Cardiol Heart Vasc. 2019;24:100395.
Merkler AE, Alakbarli J, Gialdini G, et al. Short-term risk of ischemic stroke after detection of left ventricular thrombus on cardiac magnetic resonance imaging. J Stroke Cerebrovasc Dis. 2019;28(4):1027–31.
Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack. Stroke. 2014;45(7):2160–236.
Dewilde WJM, Oirbans T, Verheugt FWA, WOEST Study Investigators, et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet. 2013;381(9872):1107–15.
Bulluck H, Chan MHH, Paradies V, et al. Incidence and predictors of left ventricular thrombus by cardiovascular magnetic resonance in acute ST-segment elevation myocardial infarction treated by primary percutaneous coronary intervention: a meta-analysis. J Cardiovasc Magn Reson. 2018;20(1):72.
Fleddermann AM, Hayes CH, Magalski A, Main ML. Efficacy of direct acting oral anticoagulants in treatment of left ventricular thrombus. Am J Cardiol. 2019;124(3):367–72.
Bahmaid RA, Ammar S, Al-Subaie S, Soofi MA, Mhish H, Yahia MA. Efficacy of direct oral anticoagulants on the resolution of left ventricular thrombus-a case series and literature review. JRSM Cardiovasc Dis. 2019;8:2048004019839548.
Yildirim E, Kalkan K, Ipek E, Demirelli S, Ermiş E. Successful resolution of left ventricular thrombus with apixaban treatment. Int J Cardiovasc Acad. 2016;2:57–8.
Azizi A, Puricel S, Cook S, Brugger N. Rivaroxaban dissolves postinfarction left ventricular thrombus. Cardiovasc Med. 2016;19:25–7.
Shokr M, Ahmed A, Abubakar H, et al. Use of direct oral anticoagulants in the treatment of left ventricular thrombi: a tertiary center experience and review of the literature. Clin Case Rep. 2019;7(1):135–42.
Cheong K-I, Chuang W-P, Wu Y-W, Huang S-H. Successful resolution of left ventricular thrombus after ST-elevation myocardial infarction by edoxaban in a patient with high bleeding risk. Acta Cardiol Sin. 2019;35(1):85–8.
Abdelnaby M, Almaghraby A, Abdelkarim O, Saleh Y, Hammad B, Badran H. The role of rivaroxaban in left ventricular thrombi. Anatol J Cardiol. 2019;21(1):47–50.
Yamamoto T, Konishi T, Funayama N, Kikuchi B, Hotta D, Ohori K. Resolution of left ventricular thrombus after dabigatran therapy in two patients with old anteroseptal myocardial infarction. Cardiol Pharmacol. 2015;4:152.
Elikowski W, Małek-Elikowska M, Wróblewski D, et al. Apixaban in left ventricular thrombi treatment—a report of seven cases. Pol Merkur Lekarski. 2018;44(264):276–9.
Kao P-H, Chou P-Y, Hsu P-C, Huang T-C. Resolution of left ventricular thrombus by edoxaban after failed treatment with warfarin overdose: a case report. Medicine (Baltimore). 2019;98(2):e14065.
Huang L-Y, Chang T-H, Wu C-H, Tsai T-N. Warfarin-resistant left ventricular thrombus completely dissolved by rivaroxaban. Br J Hosp Med (Lond). 2018;79(11):648–9.
Bennett S, Satchithananda D, Law G. The use of apixaban for the treatment of an LV thrombus. Echo Res Pract. 2018;5(4):K63–6.
Nafee T, Aslam A, Chi G, et al. Andexanet alfa for the reversal of anticoagulant activity in patients treated with direct and indirect factor Xa inhibitors. Expert Rev Cardiovasc Ther. 2017;15(4):237–45.
Lip G, Hammerstingl C, Marin F, X-TRA Study and CLOT-AF Registry Investigators, et al. Left atrial thrombus resolution in atrial fibrillation or flutter: results of a prospective study with rivaroxaban (X-TRA) and a retrospective observational registry providing baseline data (CLOT-AF). Am Heart J. 2016;178:126–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
Jessica Daher, Antoine Da Costa, Christophe Hilaire, Thomas Ferreira, Romain Pierrard, Jean Baptiste Guichard, Cécile Romeyer, and Karl Isaaz have no conflicts of interest related to this study.
Ethical Approval
All procedures in this study were in accordance with the 1964 Helsinki Declaration (and its amendments). No approval was required for this study due to its retrospective design.
Informed Consent
Informed written consent was obtained from patients in order to use their medical information.
Rights and permissions
About this article
Cite this article
Daher, J., Da Costa, A., Hilaire, C. et al. Management of Left Ventricular Thrombi with Direct Oral Anticoagulants: Retrospective Comparative Study with Vitamin K Antagonists. Clin Drug Investig 40, 343–353 (2020). https://doi.org/10.1007/s40261-020-00898-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-020-00898-3