Abstract
Objective
To evaluate the performance of a disproportionality design, commonly used for analysis of spontaneous reports data such as the FDA Adverse Event Reporting System database, as a potential analytical method for an adverse drug reaction risk identification system using healthcare data.
Research Design
We tested the disproportionality design in 5 real observational healthcare databases and 6 simulated datasets, retrospectively studying the predictive accuracy of the method when applied to a collection of 165 positive controls and 234 negative controls across 4 outcomes: acute liver injury, acute myocardial infarction, acute kidney injury, and upper gastrointestinal bleeding.
Measures
We estimate how well the method can be expected to identify true effects and discriminate from false findings and explore the statistical properties of the estimates the design generates. The primary measure was the area under the curve (AUC) of the receiver operating characteristic (ROC) curve.
Results
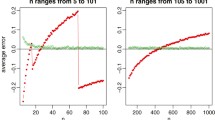
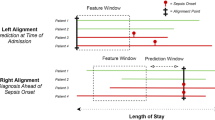
For each combination of 4 outcomes and 5 databases, 48 versions of disproportionality analysis (DPA) were carried out and the AUC computed. The majority of the AUC values were in the range of 0.35 < AUC < 0.6, which is considered to be poor predictive accuracy, since the value AUC = 0.5 would be expected from mere random assignment. Several DPA versions achieved AUC of about 0.7 for the outcome Acute Renal Failure within the GE database. The overall highest DPA version across all 20 outcome-database combinations was the Bayesian Information Component method with no stratification by age and gender, using first occurrence of outcome and with assumed time-at-risk equal to duration of exposure + 30d, but none were uniformly optimal. The relative risk estimates for the negative control drug-event combinations were very often biased either upward or downward by a factor of 2 or more. Coverage probabilities of confidence intervals from all methods were far below nominal.
Conclusions
The disproportionality methods that we evaluated did not discriminate true positives from true negatives using healthcare data as they seem to do using spontaneous report data.





Similar content being viewed by others
References
Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22(4):719–48.
Almenoff JS, Pattishall EN, Gibbs TG, DuMouchel W, Evans SJ, Yuen N. Novel statistical tools for monitoring the safety of marketed drugs. Clin Pharmacol Ther. 2007;82(2):157–66.
DuMouchel W, Pregibon D. Empirical Bayes screening for multi-item associations. In: Proceedings of the seventh ACM SIGKDD international conference on Knowledge discovery and data mining. San Francisco: ACM; 2001. p. 67–76.
Dumouchel W. Bayesian data mining in large frequency tables, with an application to the FDA spontaneous reporting system. Am Stat. 1999;53(3):177–90.
Norén GN, Hopstadius J, Bate A. Shrinkage observed-to-expected ratios for robust and transparent large-scale pattern discovery. Stat Methods Med Res 2013;22(1):57–69.
Hauben M, Madigan D, Gerrits CM, Walsh L, Van Puijenbroek EP. The role of data mining in pharmacovigilance. Expert Opin Drug Saf. 2005;4(5):929–48.
Hauben M, Reich L. Safety related drug-labelling changes: findings from two data mining algorithms. Drug Saf. 2004;27(10):735–44.
Szarfman A, Machado SG, O’Neill RT. Use of screening algorithms and computer systems to efficiently signal higher-than-expected combinations of drugs and events in the US FDA’s spontaneous reports database. Drug Saf. 2002;25(6):381–92.
Zorych I, Madigan D, Ryan P, Bate A. Disproportionality methods for pharmacovigilance in longitudinal observational databases. Stat Methods Med Res. 2013;22(1):39–56.
Evans SJ, Waller PC, Davis S. Use of proportional reporting ratios (PRRs) for signal generation from spontaneous adverse drug reaction reports. Pharmacoepidemiol Drug Saf. 2001;10(6):483–6.
Bate A, Lindquist M, Edwards IR, Olsson S, Orre R, Lansner A, et al. A Bayesian neural network method for adverse drug reaction signal generation. Eur J Clin Pharmacol. 1998;54(4):315–21.
Ryan PB, Schuemie M. Evaluating performance of risk identification methods through a large-scale simulation of observational data. Drug Saf. 2013 (in this supplement issue). doi:10.1007/s40264-013-0110-2.
Overhage JM, Ryan PB, Schuemie MJ, Stang PE. Desideratum for evidence based epidemiology. Drug Saf. 2013 (in this supplement issue). doi:10.1007/s40264-013-0102-2.
Hartzema AG, Reich CG, Ryan PB, Stang PE, Madigan D, Welebob E, et al. Managing data quality for a drug safety surveillance system. Drug Saf. 2013 (in this supplement issue). doi:10.1007/s40264-013-0098-7.
Cantor SB, Kattan MW. Determining the area under the ROC curve for a binary diagnostic test. Med Decis Making. 2000;20(4):468–70.
Fram DM, Almenoff JS, DuMouchel W. Empirical Bayesian data mining for discovering patterns in post-marketing drug safety. In: Proceedings of the Ninth ACM SIGKDD International Conference on Knowledge Discovery and Data Mining. Washington, DC: ACM; 2003. p. 359–68.
Almenoff JS, DuMouchel W, Kindman LA, Yang X, Fram D. Disproportionality analysis using empirical Bayes data mining: a tool for the evaluation of drug interactions in the post-marketing setting. Pharmacoepidemiol Drug Saf. 2003;12(6):517–21.
DuMouchel W, Smith ET, Beasley R, Nelson H, Yang X, Fram D, et al. Association of asthma therapy and Churg-Strauss syndrome: an analysis of postmarketing surveillance data. Clin Ther. 2004;26(7):1092–104.
Almenoff JS, LaCroix KK, Yuen NA, Fram D, DuMouchel W. Comparative performance of two quantitative safety signalling methods: implications for use in a pharmacovigilance department. Drug Saf. 2006;29(10):875–87.
Solomon R, Dumouchel W. Contrast media and nephropathy: findings from systematic analysis and Food and Drug Administration reports of adverse effects. Invest Radiol. 2006;41(8):651–60.
DuMouchel W, Fram D, Yang X, Mahmoud RA, Grogg AL, Engelhart L, et al. Antipsychotics, glycemic disorders, and life-threatening diabetic events: a Bayesian data-mining analysis of the FDA adverse event reporting system (1968-2004). Ann Clin Psychiatry. 2008;20(1):21–31.
Harpaz R, DuMouchel W, LePendu P, Bauer-Mehren A, Ryan P, Shah NH. Performance of pharmacovigilance signal-detection algorithms for the FDA adverse event reporting system. Clin Pharmacol Ther. 2013;93(6):539–46.
Schuemie MJ, Coloma PM, Straatman H, et al. Using electronic healthcare records for drug safety signal detection; a comparative evaluation of statistical methods. Med Care. 2012;50(10):890–7.
Acknowledgments
The Observational Medical Outcomes Partnership is funded by the Foundation for the National Institutes of Health (FNIH) through generous contributions from the following: Abbott, Amgen Inc., AstraZeneca, Bayer Healthcare Pharmaceuticals, Inc., Biogen Idec, Bristol-Myers Squibb, Eli Lilly & Company, GlaxoSmithKline, Janssen Research and Development, Lundbeck, Inc., Merck & Co., Inc., Novartis Pharmaceuticals Corporation, Pfizer Inc, Pharmaceutical Research Manufacturers of America (PhRMA), Roche, Sanofi-aventis, Schering-Plough Corporation, and Takeda. Dr. DuMouchel is an employee of Oracle Health Sciences. Drs. Ryan and Schuemie are employees of Janssen Research and Development. Dr. Schuemie received a fellowship from the Office of Medical Policy, Center for Drug Evaluation and Research, Food and Drug Administration. Drs. Schuemie and Madigan have received grants from FNIH.
This article was published in a supplement sponsored by the Foundation for the National Institutes of Health (FNIH). The supplement was guest edited by Stephen J.W. Evans. It was peer reviewed by Olaf H. Klungel who received a small honorarium to cover out-of-pocket expenses. S.J.W.E has received travel funding from the FNIH to travel to the OMOP symposium and received a fee from FNIH for the review of a protocol for OMOP. O.H.K has received funding for the IMI-PROTECT project.from the Innovative Medicines Initiative Joint Undertaking (http://www.imi.europa.eu) under Grant Agreement no 115004, resources of which are composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies’ in kind contribution.
Author information
Authors and Affiliations
Corresponding author
Additional information
The OMOP research used data from Truven Health Analytics (formerly the Health Business of Thomson Reuters), and includes MarketScan® Research Databases, represented with MarketScan Lab Supplemental (MSLR, 1.2 m persons), MarketScan Medicare Supplemental Beneficiaries (MDCR, 4.6 m persons), MarketScan Multi-State Medicaid (MDCD, 10.8 m persons), MarketScan Commercial Claims and Encounters (CCAE, 46.5 m persons). Data also provided by Quintiles® Practice Research Database (formerly General Electric’s Electronic Health Record, 11.2 m persons) database. GE is an electronic health record database while the other four databases contain administrative claims data.
Appendix
Appendix

Disproportionality estimates for all test cases, by database. MSLR MarketScan Lab Supplemental, MDCD MarketScan Multi‐state Medicaid, MDCR MarketScan Medicare Supplemental Beneficiaries, CCAE MarketScan Commercial Claims and Encounters, GE GE centricity. Blue negative controls, Orange positive controls; each line represents point estimate and 95 %
Rights and permissions
About this article
Cite this article
DuMouchel, W., Ryan, P.B., Schuemie, M.J. et al. Evaluation of Disproportionality Safety Signaling Applied to Healthcare Databases. Drug Saf 36 (Suppl 1), 123–132 (2013). https://doi.org/10.1007/s40264-013-0106-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-013-0106-y