Abstract
Objective
Our objective was to investigate associations between proton pump inhibitor (PPIs) use and infection-related hospitalizations among residents of long-term care facilities (LTCFs).
Methods
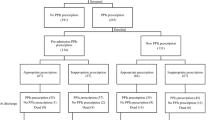
This was a case–control study of residents aged ≥ 65 years admitted to hospital between July 2013 and June 2015. Residents admitted for infections (cases) and falls or fall-related injuries (controls) were matched for age (± 2 years), sex, and index date of admission (± 6 months). Conditional logistic regression was used to estimate crude and adjusted odds ratios (aORs) and 95% confidence intervals (CIs) for associations between PPI use and infection-related hospitalizations. Analyses were adjusted for age, sex, polypharmacy, diabetes, heart failure, chronic obstructive pulmonary disease, myocardial infarction, cerebrovascular accident, and concomitant use of cancer and immunosuppressant medications. Subgroup analyses were performed for high- and low/moderate-intensity PPIs and for respiratory and non-respiratory infections. Logistic regression was used to compare the odds of infection-related hospitalizations among users of high- and low/moderate-intensity PPIs.
Results
Overall, 181 cases were matched to 354 controls. Preadmission PPI use was associated with infection-related hospitalizations (aOR 1.66; 95% CI 1.11–2.48). In subgroup analyses, the association was apparent only for respiratory infections (aOR 2.26; 95% CI 1.37–3.73) and high-intensity PPIs (aOR 1.93; 95% CI 1.23–3.04). However, the risk of infection-related hospitalization was not significantly higher among users of high- versus low/moderate-intensity PPIs (aOR 1.25; 95% CI 0.74–2.13).
Conclusion
Residents who use PPIs may be at increased risk of infection-related hospitalizations, particularly respiratory infections. Study findings provide further support for initiatives to minimize unnecessary PPI use in the LTCF setting.


Similar content being viewed by others
References
Kruger K, Jansen K, Grimsmo A, Eide GE, Geitung JT. Hospital admissions from nursing homes: rates and reasons. Nurs Res Pract. 2011;2011:247623. https://doi.org/10.1155/2011/247623.
Lalic S, Sluggett JK, Ilomäki J, Wimmer BC, Tan ECK, Robson L, et al. Polypharmacy and medication regimen complexity as risk factors for hospitalization among residents of long-term care facilities: a prospective cohort study. J Am Med Dir Assoc. 2016;17(11):1067. https://doi.org/10.1016/j.jamda.2016.08.019.
Wang HE, Shah MN, Allman RM, Kilgore M. Emergency department visits by nursing home residents in the United States. J Am Geriatr Soc. 2011;59(10):1864–72. https://doi.org/10.1111/j.1532-5415.2011.03587.x.
Strausbaugh LJ, Sukumar SR, Joseph CL, High KP. infectious disease outbreaks in nursing homes: an unappreciated hazard for frail elderly persons. Clin Infect Dis. 2003;36(7):870–6. https://doi.org/10.1086/368197.
Hospital-acquired Complications Curation Clinical Advisory Group. Hospital-acquired complications (HACs). Sydney: Australian Commission on Safety and Quality in Health Care; 2018.
Jokanovic N, Jamsen KM, Tan ECK, Dooley MJ, Kirkpatrick CM, Bell JS. Prevalence and variability in medications contributing to polypharmacy in long-term care facilities. Drugs Real World Outcomes. 2017;4(4):235–45. https://doi.org/10.1007/s40801-017-0121-x.
de Souto Barreto P, Lapeyre-Mestre M, Mathieu C, Piau C, Bouget C, Cayla F, et al. Prevalence and associations of the use of proton-pump inhibitors in nursing homes: a cross-sectional study. J Am Med Dir Assoc. 2013;14(4):265–9. https://doi.org/10.1016/j.jamda.2012.10.018.
Roughead EE, Ramsay EN, Barratt JD, Kalisch Ellett LM, Kerr M, Pratt NL, et al. Use of proton pump inhibitors among older Australians: national quality improvement programmes have led to sustained practice change. Int J Qual Health Care. 2016;29(1):75–82. https://doi.org/10.1093/intqhc/mzw138.
Australian Medicines Handbook. Adelaide: Australian Medicines Handbook Pty Ltd; 2019.
Freedberg DE, Kim LS, Yang YX. The Risks and benefits of long-term use of proton pump inhibitors: expert review and best practice advice from the American gastroenterological association. Gastroenterology. 2017;152(4):706–15. https://doi.org/10.1053/j.gastro.2017.01.031.
Rane PP, Guha S, Chatterjee S, Aparasu RR. Prevalence and predictors of non-evidence based proton pump inhibitor use among elderly nursing home residents in the US. Res Social Adm Pharm. 2017;13(2):358–63. https://doi.org/10.1016/j.sapharm.2016.02.012.
Zirk-Sadowski J, Masoli JA, Delgado J, Hamilton W, Strain WD, Henley W, et al. Proton-pump inhibitors and long-term risk of community-acquired pneumonia in older adults. J Am Geriatr Soc. 2018;66(7):1332–8. https://doi.org/10.1111/jgs.15385.
Laheij RF, Sturkenboom MM, Hassing R, Dieleman J, Stricker BC, Jansen JJ. Risk of community-acquired pneumonia and use of gastric acid–suppressive drugs. JAMA. 2004;292(16):1955–60. https://doi.org/10.1001/jama.292.16.1955.
Chen Y, Liu B, Glass K, Du W, Banks E, Kirk M. Use of proton pump inhibitors and the risk of hospitalization for infectious gastroenteritis. PLoS One. 2016;11(12):e0168618. https://doi.org/10.1371/journal.pone.0168618.
Al-Tureihi FIJ, Hassoun A, Wolf-Klein G, Isenberg H. Albumin, length of stay, and proton pump inhibitors: key factors in Clostridium difficile-associated disease in nursing home patients. J Am Med Dir Assoc. 2005;6(2):105–8. https://doi.org/10.1016/j.jamda.2005.01.003.
Dial S, Delaney JC, Barkun AN, Suissa S. Use of gastric acid–suppressive agents and the risk of community-acquired Clostridium difficile–associated disease. J Am Med Assoc. 2005;294(23):2989–95. https://doi.org/10.1001/jama.294.23.2989.
Wang KN, Bell JS, Chen EYH, Gilmartin-Thomas JFM, Ilomaki J. Medications and prescribing patterns as factors associated with hospitalizations from long-term care facilities: a systematic review. Drugs Aging. 2018;35(5):423–57. https://doi.org/10.1007/s40266-018-0537-3.
Dublin S, Walker RL, Jackson ML, Nelson JC, Weiss NS, Jackson LA. Use of proton pump inhibitors and H2 blockers and risk of pneumonia in older adults: a population-based case-control study. Pharmacoepidemiol Drug Saf. 2010;19(8):792–802. https://doi.org/10.1002/pds.1978.
Sultan N, Nazareno J, Gregor J. Association between proton pump inhibitors and respiratory infections: a systematic review and meta-analysis of clinical trials. Can J Gastroenterol Journal canadien de gastroenterologie. 2008;22(9):761–6.
World Health Organization. International statistical classification of diseases and related health problems 10th Revision. 2016. http://apps.who.int/classifications/icd10/browse/2016/en. Accessed 12 June 2018.
Vaezi M, Yang Y, Howden CW. Complications of proton pump inhibitor therapy. Gastroenterology. 2017;153(1):35–48. https://doi.org/10.1053/j.gastro.2017.04.047.
Ngamruengphong S, Leontiadis GI, Radhi S, Dentino A, Nugent K. Proton pump inhibitors and risk of fracture: a systematic review and meta-analysis of observational studies. Am J Gastroenterol. 2011;106(7):1209–18. https://doi.org/10.1038/ajg.2011.113.
Pearce N, Vandenbroucke JP. Case–control studies: basic concepts. Int J Epidemiol. 2012;41(5):1480–9. https://doi.org/10.1093/ije/dys147.
ATC/DDD Index 2017. WHO Collaborating centre for drug statistics methodology, Oslo. 2017. https://www.whocc.no/atc_ddd_index/. Accessed 01 Aug 2017.
Dosage information on proton pump inhibitors. In: Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management. National Institute for Health and Care Excellence, United Kingdom. 2014. https://www.nice.org.uk/guidance/cg184/chapter/Appendix-A-Dosage-information-on-proton-pump-inhibitors. Accessed 09 Aug 2017.
Alon D, Stein GY, Korenfeld R, Fuchs S. Predictors and outcomes of infection-related hospital admissions of heart failure patients. PLoS One. 2013;8(8):e72476. https://doi.org/10.1371/journal.pone.0072476.
Dalrymple LS, Mu Y, Nguyen DV, Romano PS, Chertow GM, Grimes B, et al. Risk factors for infection-related hospitalization in in-center hemodialysis. Clin J Am Soc Nephrol. 2015;10(12):2170–80. https://doi.org/10.2215/CJN.03050315.
Dalrymple LS, Johansen KL, Chertow GM, Cheng S-C, Grimes B, Gold EB, et al. Infection-related hospitalizations in older patients with end-stage renal disease. Am J Kidney Dis. 2010;56(3):522–30. https://doi.org/10.1053/j.ajkd.2010.04.016.
Jokanovic N, Tan ECK, Dooley MJ, Kirkpatrick CM, Bell JS. Prevalence and factors associated with polypharmacy in long-term care facilities: a systematic review. J Am Med Dir Assoc. 2015;16(6):535. https://doi.org/10.1016/j.jamda.2015.03.003.
Orlicka K, Barnes E, Culver EL. Prevention of infection caused by immunosuppressive drugs in gastroenterology. Ther Adv Chronic Dis. 2013;4(4):167–85. https://doi.org/10.1177/2040622313485275.
Vento S, Cainelli F. Infections in patients with cancer undergoing chemotherapy: aetiology, prevention, and treatment. Lancet Oncol. 2003;4(10):595–604. https://doi.org/10.1016/S1470-2045(03)01218-X.
Rolston KVI. Infections in cancer patients with solid tumors: a review. Infect Dis Ther. 2017;6(1):69–83. https://doi.org/10.1007/s40121-017-0146-1.
Sloan KL, Sales AE, Liu CF, Fishman P, Nichol P, Suzuki NT, et al. Construction and characteristics of the RxRisk-V: a VA-adapted pharmacy-based case-mix instrument. Med Care. 2003;41(6):761–74. https://doi.org/10.1097/01.mlr.0000064641.84967.b7.
Lalic S, Gisev N, Bell JS, Korhonen MJ, Ilomäki J. Predictors of persistent prescription opioid analgesic use among people without cancer in Australia. Br J Clin Pharmacol. 2018;84(6):1267–78. https://doi.org/10.1111/bcp.13556.
Dean AG, Sullivan KM, MM. S. Open source epidemiologic statistics for public health. 2006. http://www.OpenEpi.com. Accessed 12 May 18.
Eom C-S, Jeon CY, Lim J-W, Cho E-G, Park SM, Lee K-S. Use of acid-suppressive drugs and risk of pneumonia: a systematic review and meta-analysis. CMAJ Can Med Assoc J. 2011;183(3):310–9. https://doi.org/10.1503/cmaj.092129.
Wang CH, Li CH, Hsieh R, Fan CY, Hsu TC, Chang WC, et al. Proton pump inhibitors therapy and the risk of pneumonia: a systematic review and meta-analysis of randomized controlled trials and observational studies. Expert Opin Drug Saf. 2019. https://doi.org/10.1080/14740338.2019.1577820.
Theisen J, Nehra D, Citron D, Johansson J, Hagen JA, Crookes PF, et al. Suppression of gastric acid secretion in patients with gastroesophageal reflux disease results in gastric bacterial overgrowth and deconjugation of bile acids. J Gastrointest Surg. 2000;4(1):50–4.
Trifan A, Stanciu C, Girleanu I, Stoica OC, Singeap AM, Maxim R, et al. Proton pump inhibitors therapy and risk of Clostridium difficile infection: systematic review and meta-analysis. World J Gastroenterol. 2017;23(35):6500–15. https://doi.org/10.3748/wjg.v23.i35.6500.
Hegarty JP, Sangster W, Harris LR 3rd, Stewart DB. Proton pump inhibitors induce changes in colonocyte gene expression that may affect Clostridium difficile infection. Surgery. 2014;156(4):972–8. https://doi.org/10.1016/j.surg.2014.06.074.
Seto CT, Jeraldo P, Orenstein R, Chia N, DiBaise JK. Prolonged use of a proton pump inhibitor reduces microbial diversity: implications for Clostridium difficile susceptibility. Microbiome. 2014;2:42. https://doi.org/10.1186/2049-2618-2-42.
Jena AB, Sun E, Goldman DP. Confounding in the association of proton pump inhibitor use with risk of community-acquired pneumonia. J Gen Intern Med. 2013;28(2):223–30. https://doi.org/10.1007/s11606-012-2211-5.
Kinoshita Y, Ishimura N, Ishihara S. Advantages and disadvantages of long-term proton pump inhibitor use. J Neurogastroenterol Motil. 2018;24(2):182–96. https://doi.org/10.5056/jnm18001.
Nochaiwong S, Ruengorn C, Awiphan R, Koyratkoson K, Chaisai C, Noppakun K, et al. The association between proton pump inhibitor use and the risk of adverse kidney outcomes: a systematic review and meta-analysis. Nephrol Dial Transplant. 2018;33(2):331–42. https://doi.org/10.1093/ndt/gfw470.
Naqvi SB, Collins AJ. Infectious complications in chronic kidney disease. Adv Chronic Kidney Dis. 2006;13(3):199–204. https://doi.org/10.1053/j.ackd.2006.04.004.
Genao L, Buhr GT. Urinary tract infections in older adults residing in long-term care facilities. Ann Long-Term Care. 2012;20(4):33–8.
Qiu Z, Liu H, He L, Ma Y, Song H, Bai W, et al. Proton pump inhibitor-induced exfoliative dermatitis: a case report. Exp Ther Med. 2016;11(2):543–6. https://doi.org/10.3892/etm.2015.2926.
Karakayli G, Beckham G, Orengo I, Rosen T. Exfoliative dermatitis. Am Fam Physician. 1999;59(3):625–30.
Rose S, Laan MJVD. Why match? Investigating matched case–control study designs with causal effect estimation. Int J Biostat. 2009;5(1):1. https://doi.org/10.2202/1557-4679.1127.
Hendrix I, Page AT, Korhonen MJ, Bell JS, Tan ECK, Visvanathan R, et al. Patterns of high-dose and long-term proton pump inhibitor use: a cross-sectional study in six south australian residential aged care services. Drugs Real World Outcomes. 2019. https://doi.org/10.1007/s40801-019-0157-1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
KW is supported through an Australian Government Research Training Program Scholarship. JSB is supported by a National Health and Medical Research Council (NHMRC) Dementia Leadership Fellowship (#1140298). JG-T and ET are NHMRC-Australian Research Council (ARC) Dementia Research Development Fellows (APP1107476 and APP1107381). JI is supported by an NHMRC Early Career Research Fellowship (#1072137).
Conflict of interest
KW and MD are both currently employed by Alfred Health. JSB, ECKT, JFMG-T, and JI have no conflicts of interest that are directly relevant to the content of this article.
Informed consent
All participant details were deidentified and anonymous.
Rights and permissions
About this article
Cite this article
Wang, K.N., Bell, J.S., Tan, E.C.K. et al. Proton Pump Inhibitors and Infection-Related Hospitalizations Among Residents of Long-Term Care Facilities: A Case–Control Study. Drugs Aging 36, 1027–1034 (2019). https://doi.org/10.1007/s40266-019-00704-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-019-00704-6