Abstract
Background and Objective
Hypertension is the most prevalent chronic disease in older adults. Antihypertensive drug use increases with aging. In some studies, hypotension developing under antihypertensive medication use has been indicated as a potential risk factor for morbidity and mortality in older adults. Our objective was to assess the relationship between hypotension under antihypertensive treatment and incident hospitalization of nursing home residents.
Methods
We detailed blood pressure measurements of the previous 1-year period that were noted regularly at 2-week intervals and studied their mean values. The systolic blood pressure (SBP) and diastolic blood pressure (DBP) thresholds to define low SBP (≤ 110 mm Hg) and DBP (≤ 65 mm Hg) were derived from our previous study. We noted demographics, number of co-morbidities and regular medications, mobility status, and nutritional assessment via the Mini Nutritional Assessment Short Form.
Results
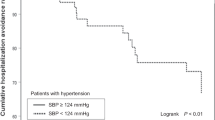
We included 253 participants (66% male, mean age 75.7 ± 8.7 years). The prevalence of low SBP (≤ 110 mmHg) and low DBP (≤ 65 mmHg) was 34.8% and 15.8%, respectively. Among residents, 4% were bedridden, 15.8% wheelchair bound, 14.5% needing assistance for reduced mobility, and 62.7% were ambulatory. At a median of 15 months of follow-up, hospitalization incidence from any cause was 50.8% (n = 134). Incident hospitalization was more common in the group that had low DBP (odds ratio = 3.06; 95% confidence interval 1.02–9.15; p = 0.04) after adjusting for age, number of comorbidities and medications, mobility status, and nutritional status. Low SBP was not associated with hospitalization.
Conclusions
The low DBP (≤ 65 mm Hg) during the previous year was associated with incident hospitalization of nursing home residents after adjustment for several factors. These findings indicate that lower DBP may be a causative factor for incident hospitalization. We need further studies to explore whether a correction of diastolic hypotension may decrease the hospitalization risk in this vulnerable population.
Similar content being viewed by others

References
Bahat G, Tufan F, Bahat Z, et al. Assessments of functional status, comorbidities, polypharmacy, nutritional status and sarcopenia in Turkish community-dwelling male elderly. Aging Male. 2013;16(2):67–72.
Bahat G, Tufan F, Bahat Z, et al. Comorbidities, polypharmacy, functionality and nutritional status in Turkish community-dwelling female elderly. Aging Clin Exp Res. 2014;26(3):255–9.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957–80.
Briasoulis A, Agarwal V, Tousoulis D, Stefanadis C. Effects of antihypertensive treatment in patients over 65 years of age: a meta-analysis of randomised controlled studies. Heart. 2014;100(4):317–23.
Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥ 75 years: a randomized clinical trial. JAMA. 2016;315(24):2673–82.
Charlesworth CJ, Smit E, Lee DS, Alramadhan F, Odden MC. Polypharmacy among adults aged 65 years and older in the United States: 1988–2010. J Geront A Biol Sci Med Sci. 2015;70(8):989–95.
Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–337.
Bahat G, Tufan A, Karan MA. Under-representation of frail or medically compromised hypertensive older people. Heart. 2014;100(11):894.
Peralta CA, Katz R, Newman AB, Psaty BM, Odden MC. Systolic and diastolic blood pressure, incident cardiovascular events, and death in elderly persons: the role of functional limitation in the Cardiovascular Health Study. Hypertension. 2014;64(3):472–80.
Odden MC, Peralta CA, Haan MN, Covinsky KE. Rethinking the association of high blood pressure with mortality in elderly adults: the impact of frailty. Arch Intern Med. 2012;172(15):1162–8.
Odden MC, Covinsky KE, Neuhaus JM, Mayeda ER, Peralta CA, Haan MN. The association of blood pressure and mortality differs by self-reported walking speed in older Latinos. J Gerontol A Biol Sci Med Sci. 2012;67(9):977–83.
Tinetti ME, Han L, Lee DS, et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174(4):588–95.
Charlesworth CJ, Peralta CA, Odden MC. Functional status and antihypertensive therapy in older adults: a new perspective on old data. Am J Hypertens. 2016;29(6):690–5.
Gutierrez-Misis A, Sanchez-Santos MT, Banegas JR, Castell MV, Gonzalez-Montalvo JI, Otero A. Walking speed and high blood pressure mortality risk in a Spanish elderly population. J Hum Hypertens. 2015;29(9):566–72.
Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16.
Bahat G, İlhan B, Tufan A, Karan MA. Blood pressure goals in functionally limited elderly patients. Am J Med. 2017;130(7):e319–20.
Bahat G, Ilhan B, Tufan A, Karan MA. Intensive blood pressure treatment in adults aged 60 years or older. Ann Intern Med. 2017;167(4):288.
Bahat G, Ilhan B, Tufan A, et al. Hypotension in nursing home residents on antihypertensive treatment: is it associated with mortality? J Am Med Dir Assoc. 2021;22(11):2319-24.e4.
Benetos A, Labat C, Rossignol P, et al. Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: the PARTAGE study. JAMA Intern Med. 2015;175(6):989–95.
Benetos A, Petrovic M, Strandberg T. Hypertension management in older and frail older patients. Circ Res. 2019;124(7):1045–60.
Boockvar KS, Song W, Lee S, Intrator O. Hypertension treatment in US long-term nursing home residents with and without dementia. J Am Geriatr Soc. 2019;67(10):2058–64.
Mallet L, Spinewine A, Huang A. The challenge of managing drug interactions in elderly people. Lancet. 2007;370(9582):185–91.
Kojima G, Liljas AEM, Iliffe S. Frailty syndrome: implications and challenges for health care policy. Risk Manag Healthc Policy. 2019;12:23–30.
Benetos A, Bulpitt CJ, Petrovic M, et al. An expert opinion from the European Society of Hypertension-European Union Geriatric Medicine Society Working Group on the management of hypertension in very old, frail subjects. Hypertension. 2016;67(5):820–5.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2018;138(17):e426–83.
Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–104.
Warwick J, Falaschetti E, Rockwood K, et al. No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: an investigation of the impact of frailty upon treatment effect in the HYpertension in the Very Elderly Trial (HYVET) study, a double-blind, placebo-controlled study of antihypertensives in people with hypertension aged 80 and over. BMC Med. 2015;13(1):78.
Cesari M, Gambassi G, Abellan van Kan G, Vellas B. The frailty phenotype and the frailty index: different instruments for different purposes. Age Ageing. 2013;43(1):10–2.
Streit S, Poortvliet RKE, Gussekloo J. Lower blood pressure during antihypertensive treatment is associated with higher all-cause mortality and accelerated cognitive decline in the oldest-old: data from the Leiden 85-plus Study. Age Ageing. 2018;47(4):545–50.
Anderson TS, Jing B, Auerbach A, et al. Clinical outcomes after intensifying antihypertensive medication regimens among older adults at hospital discharge. JAMA Intern Med. 2019;179(11):1528–36.
Albasri A, Hattle M, Koshiaris C, et al. Association between antihypertensive treatment and adverse events: systematic review and meta-analysis. BMJ. 2021;372: n189.
Vu M, Schleiden LJ, Harlan ML, Thorpe CT. Hypertension management in nursing homes: review of evidence and considerations for care. Curr Hypertens Rep. 2020;22(1):8.
Mangin D, Bahat G, Golomb BA, Mallery LH, Moorhouse P, Onder G, et al. International Group for Reducing Inappropriate Medication Use and Polypharmacy (IGRIMUP): position statement and 10 recommendations for action. Drugs Aging. 2018;35:575–87.
Garfinkel D, Ilhan B, Bahat G. Routine deprescribing of chronic medications to combat polypharmacy. Ther Adv Drug Saf. 2015;6:212–33.
Benetos A. How to obtain more evidence for the management of hypertension in frail patients over 80 years old? Eur Geriatr Med. 2018;9:137–40.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this article or the conduct of this study.
Conflicts of interest/competing interests
GB, BI, AT, CK, MAK, and MP have no conflicts of interest that are directly relevant to the contents of this study.
Ethics approval
This study was approved by the ethical committees at all participating sites and was conducted in accordance with the
Declaration of Helsinki.
Consent to participate
Informed consent was obtained from every patient and/or their parent or legal representative.
Consent for publication
Not applicable.
Availability of data and material
Anonymized data will be shared at the request of any qualified investigator.
Code availability
Not applicable.
Authors’ contributions
GB designed and conceptualized the study, coordinated and supervised the data collection, carried out the data analyses, and drafted the manuscript. AT, BI, CK,MAK, and MP designed and conceptualized the study, and coordinated and supervised the data collection. GB, AT, BI, CK, MAK, and MP were involved in the acquisition of data. All authors critically revised the manuscript for important intellectual content. All authors approved the final manuscript for submission and agree to be accountable for all aspects of the work.
Rights and permissions
About this article
Cite this article
Bahat, G., İlhan, B., Tufan, A. et al. Hypotension Under Antihypertensive Treatment and Incident Hospitalizations of Nursing Home Residents. Drugs Aging 39, 477–484 (2022). https://doi.org/10.1007/s40266-022-00951-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-022-00951-0