Abstract
Background
According to previous epidemiological studies, there are pros and cons for the relationship between running regularly and changes in resting blood pressure (RBP), and the changes may depend on the form of exercise.
Objective
The aims of the current systematic review were to summarize the effects of running regularly on RBP and to investigate the most efficacious form of running in reducing RBP for this purpose.
Methods
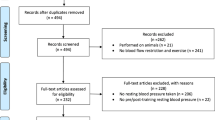
The inclusion criteria were: randomized controlled trials, involving healthy adults or adults with hypertension, the exercise group only performed regular running and the control group did not exercise, and the study reported the mean resting systolic blood pressure (RSBP) and/or diastolic blood pressure (RDBP). The mean difference (MD) in RBP in each trial was defined as follows: (mean value at post-intervention in the exercise group − mean value at baseline in the exercise group) − (mean value at post-intervention in the control group − mean value at baseline in the control group) and was calculated. The weighted MD (WMD) was defined as the synthesis of all MD. A linear meta-regression analysis, exercise intensity [the percentage of maximum heart rate] (%) and total exercise time throughout the intervention (hours) were selected as explanatory variables and the MD in RBP served as the objective variable.
Results
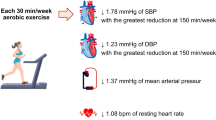
Twenty-two trials (736 subjects) were analyzed. When trials were limited to those involving healthy subjects, the WMD in RBP decreased significantly [RSBP: − 4.2 mmHg (95% confidence intervals (95% CI) − 5.9 to − 2.4); RDBP: − 2.7 mmHg (95% CI − 4.2 to − 1.1)] and did not contain significant heterogeneity (RSBP: P = 0.67, I2 = 0.0%; DBP: P = 0.38, I2 = 7.2%). When trials were limited to those involving subjects with hypertension, the WMD in RBP decreased significantly [RSBP: − 5.6 mmHg (95% CI − 9.1 to − 2.1); RDBP: − 5.2 mmHg (95% CI − 9.0 to − 1.4)] but contained significant heterogeneity (RSBP: P = 0.01, I2 = 62.2%; DBP: P < 0.01, I2 = 87.7) and a meta-regression analysis showed that the percentage of maximum heart rate was significantly associated with the WMD in RSBP [slope: 0.56 (95% CI 0.21 to 0.92), intercept: − 48.76 (95% CI − 76.30 to − 21.22), R2 = 0.88] and RDBP [slope: 0.45 (95% CI 0.01 to 0.87), intercept: − 38.06 (95% CI − 72.30 to − 4.08), R2 = 0.41]. When trials were limited to those involving subjects with hypertension and a mean age ≥ 40 years, a meta-regression analysis showed that total exercise time throughout the intervention was significantly associated with the WMD in RDBP [slope: 0.82 (95% CI 0.54 to 1.09), intercept: − 22.90 (95% CI − 29.04 to − 16.77), R2 = 0.99].
Conclusions
Running regularly decreases RBP, but the changes in subjects with hypertension may differ depending on exercise intensity or total exercise time. Therefore, running regularly at moderate intensity and at a restrained volume is recommended to lower RBP in subjects with hypertension.




Similar content being viewed by others
Data Availability Statement
All data are available in submitted manuscript or as electronic supplementary material.
References
Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief. 2013;133:1–8.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
Kokubo Y. Prevention of hypertension and cardiovascular diseases: a comparison of lifestyle factors in Westerners and East Asians. Hypertension. 2014;63:655–60.
Carey RM, Muntner P, Bosworth HB, Whelton PK. Prevention and control of hypertension: JACC Health Promotion Series. J Am Coll Cardiol. 2018;72:1278–93.
Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–33.
Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2001;38:1112–7.
Graudal NA, Hubeck-Graudal T, Jürgens G. Effects of low-sodium diet vs. high-sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride (cochrane review). Am J Hypertens. 2012;25:1–15.
Murtagh EM, Nichols L, Mohammed MA, Holder R, Nevill AM, Murphy MH. The effect of walking on risk factors for cardiovascular disease: an updated systematic review and meta-analysis of randomised control trials. Prev Med. 2015;72:34–43.
Igarashi Y, Akazawa N, Maeda S. The required step count for a reduction in blood pressure: a systematic review and meta-analysis. J Hum Hypertens. 2018;32:814–24.
Oja P, Kelly P, Murtagh EM, Murphy MH, Foster C, Titze S. Effects of frequency, intensity, duration and volume of walking interventions on CVD risk factors: a systematic review and meta-regression analysis of randomised controlled trials among inactive healthy adults. Br J Sports Med. 2018;52:769–75.
Cornelissen VA, Fagard RH, Coeckelberghs E, Vanhees L. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension. 2011;58:950–8.
Igarashi Y, Nogami Y. The effect of regular aquatic exercise on blood pressure: a meta-analysis of randomized controlled trials. Eur J Prev Cardiol. 2018;25:190–9.
Igarashi Y, Akazawa N, Maeda S. Regular aerobic exercise and blood pressure in East Asians: a meta-analysis of randomized controlled trials. Clin Exp Hypertens. 2018;40:378–89.
Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503.
Manfredini F, Malagoni AM, Mandini S, Boari B, Felisatti M, et al. Sport therapy for hypertension: why, how, and how much? Angiology. 2009;60:207–16.
Ainsworth BE, Haskell WL, Herrmann SD, Meckes N, Bassett DR Jr, et al. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–81.
Stamatakis E, Chaudhury M. Temporal trends in adults’ sports participation patterns in England between 1997 and 2006: the Health Survey for England. Br J Sports Med. 2008;42:901–8.
Juraschek SP, Blaha MJ, Whelton SP, Blumenthal R, Jones SR, et al. Physical fitness and hypertension in a population at risk for cardiovascular disease: the Henry Ford ExercIse Testing (FIT) Project. J Am Heart Assoc. 2014. https://doi.org/10.1161/JAHA.114.001268.
Williams PT, Thompson PD. Walking versus running for hypertension, cholesterol, and diabetes mellitus risk reduction. Arterioscler Thromb Vasc Biol. 2013;33:1085–91.
Pressler A, Suchy C, Friedrichs T, Dallinger S, Grabs V, et al. Running multiple marathons is not a risk factor for premature subclinical vascular impairment. Eur J Prev Cardiol. 2017;24:1328–35.
Morrison BN, McKinney J, Isserow S, Lithwick D, Taunton J, et al. Assessment of cardiovascular risk and preparticipation screening protocols in masters athletes: the Master Athlete Screening Study (MASS): a cross-sectional study. BMJ Open Sport Exerc Med. 2018. https://doi.org/10.1136/bmjsem-2018-000370.
Schnohr P, O’Keefe JH, Marott JL, Lange P, Jensen GB. Dose of jogging and long-term mortality: the Copenhagen City Heart Study. J Am Coll Cardiol. 2015;65:411–9.
Lee DC, Pate RR, Lavie CJ, Sui X, Church TS, Blair SN. Leisure-time running reduces all-cause and cardiovascular mortality risk. J Am Coll Cardiol. 2014;64:472–81.
Kikuchi H, Inoue S, Lee IM, Odagiri Y, Sawada N, et al. Impact of moderate-intensity and vigorous-intensity physical activity on mortality. Med Sci Sports Exerc. 2018;50:715–21.
Lavie CJ, Lee DC, Sui X, Arena R, O’Keefe JH, et al. Effects of running on chronic diseases and cardiovascular and all-cause mortality. Mayo Clin Proc. 2015;90:1541–52.
Lee DC, Brellenthin AG, Thompson PD, Sui X, Lee IM, Lavie CJ. Running as a key lifestyle medicine for longevity. Prog Cardiovasc Dis. 2017;60:45–55.
Hespanhol Junior LC, Pillay JD, van Mechelen W, Verhagen E. Meta-analyses of the effects of habitual running on indices of health in physically inactive adults. Sports Med. 2015;45:1455–68.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647.
University of York, Centre for reviews and dissemination. PROSPERO: international prospective register of systematic reviews. 2011. https://www.crd.york.ac.uk/prospero/. Accessed 25 Jan 2019.
Cochrane Skin Group. Data collection forms for intervention reviews: RCTs only, version 3. 2014. https://skin.cochrane.org/resources. Accessed 15 May 2019.
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011. http://handbook.cochrane.org/. Accessed 25 Jan 2019.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol. 1992;45:769–73.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Londeree BR, Ames SA. Trend analysis of the % VO2 max-HR regression. Med Sci Sports. 1976;8:123–5.
Kelley GA, Kelley KS. Statistical models for meta-analysis: a brief tutorial. World J Methodol. 2012;2:27–32.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63.
Mathur DN, Toriola AL. Twelve weeks jogging effects on selected cardiovascular risk factors in untrained healthy males. J Sports Med Phys Fitness. 1984;24:259–62.
Duncan JJ, Farr JE, Upton SJ, Hagan RD, Oglesby ME, Blair SN. The effects of aerobic exercise on plasma catecholamines and blood pressure in patients with mild essential hypertension. JAMA. 1985;254(18):2609–13.
Suter E, Marti B, Tschopp A, Wanner HU, Wenk C, Gutzwiller F. Effects of self-monitored jogging on physical fitness, blood pressure and serum lipids: a controlled study in sedentary middle-aged men. Int J Sports Med. 1990;11:425–32.
Blumenthal JA, Siegel WC, Appelbaum M. Failure of exercise to reduce blood pressure in patients with mild hypertension Results of a randomized controlled trial. JAMA. 1991;266:2098–104.
Albright CL, King AC, Taylor CB, Haskell WL. Effect of a six-month aerobic exercise training program on cardiovascular responsivity in healthy middle-aged adults. J Psychosom Res. 1992;36:25–36.
Rogers MW, Probst MM, Gruber JJ, Berger R, Boone JB Jr. Differential effects of exercise training intensity on blood pressure and cardiovascular responses to stress in borderline hypertensive humans. J Hypertens. 1996;14:1369–75.
Tsai JC, Chang WY, Kao CC, Lu MS, Chen YJ, Chan P. Beneficial effect on blood pressure and lipid profile by programmed exercise training in Taiwanese patients with mild hypertension. Clin Exp Hypertens. 2002;24:315–24.
Tsai JC, Liu JC, Kao CC, Tomlinson B, Kao PF, et al. Beneficial effects on blood pressure and lipid profile of programmed exercise training in subjects with white coat hypertension. Am J Hypertens. 2002;15:571–6.
Tsai JC, Yang HY, Wang WH, Hsieh MH, Chen PT, et al. The beneficial effect of regular endurance exercise training on blood pressure and quality of life in patients with hypertension. Clin Exp Hypertens. 2004;26:255–65.
Krustrup P, Nielsen JJ, Krustrup BR, Christensen JF, Pedersen H, et al. Recreational soccer is an effective health-promoting activity for untrained men. Br J Sports Med. 2009;43:825–31.
Knoepfli-Lenzin C, Sennhauser C, Toigo M, Boutellier U, Bangsbo J, et al. Effects of a 12-week intervention period with football and running for habitually active men with mild hypertension. Scand J Med Sci Sports. 2010;20:72–9.
Krustrup P, Hansen PR, Andersen LJ, Jakobsen MD, Sundstrup E, et al. Long-term musculoskeletal and cardiac health effects of recreational football and running for premenopausal women. Scand J Med Sci Sports. 2010;20(Suppl 1):58–71.
Amin-Shokravi F, Rajabi R, Ziaee N. Exercise effects on risk of cardiovascular disease among Iranian women. Asian J Sports Med. 2011;2:37–43.
Beck DT, Martin JS, Casey DP, Braith RW. Exercise training reduces peripheral arterial stiffness and myocardial oxygen demand in young prehypertensive subjects. Am J Hypertens. 2013;26:1093–102.
Foulds HJ, Bredin SS, Charlesworth SA, Ivey AC, Warburton DE. Exercise volume and intensity: a dose-response relationship with health benefits. Eur J Appl Physiol. 2014;114:1563–71.
Hur S, Kim SR. The effects of exercise therapy on CVD risk factors in women. J Phys Ther Sci. 2014;26:1367–70.
Patterson S, Pattison J, Legg H, Gibson AM, Brown N. The impact of badminton on health markers in untrained females. J Sports Sci. 2017;35:1098–106.
Jamnik VK, Warburton DE, Makarski J, McKenzie DC, Shephard RJ, et al. Enhancing the effectiveness of clearance for physical activity participation: background and overall process. Appl Physiol Nutr Metab. 2011;36(Suppl 1):S3–13.
Boutcher YN, Boutcher SH. Exercise intensity and hypertension: what’s new? J Hum Hypertens. 2017;31:157–64.
Annuk M, Zilmer M, Fellström B. Endothelium-dependent vasodilation and oxidative stress in chronic renal failure: impact on cardiovascular disease. Kidney Int Suppl. 2003;63:S50–3.
Korsager LM, Matchkov VV. Hypertension and physical exercise: The role of oxidative stress. Medicina (Kaunas). 2016;52:19–27.
Sachdev S, Davies KJ. Production, detection, and adaptive responses to free radicals in exercise. Free Radic Biol Med. 2008;44:215–23.
Arakawa K. Antihypertensive mechanism of exercise. J Hypertens. 1993;11:223–9.
Acknowledgements
The authors wish to sincerely thank the staff of Osaka University of Health and Sports Sciences Library for collecting the articles used in this analysis and to thank the staff of International Studies Library in Osaka University, National Institute of Public Health, and Chukyo University Library for facilitating a search of the literature in electronic databases.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of interest
Yutaka Igarashi and Yoshie Nogami have no conflicts of interest relevant to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Igarashi, Y., Nogami, Y. Running to Lower Resting Blood Pressure: A Systematic Review and Meta-analysis. Sports Med 50, 531–541 (2020). https://doi.org/10.1007/s40279-019-01209-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-019-01209-3