Abstract
Background
Identifying risk factors for prolonged recovery following concussion can assist clinicians with appropriate management strategies. It is thought that athletes who continue to participate following a hit to the head or body may take longer to recover following a concussion diagnosis.
Objective
To systematically review the body of literature regarding the effect of delayed reporting and delayed presentation to medical providers on concussion recovery times.
Design
Systematic review with meta-analysis.
Data Sources
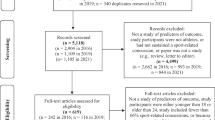
PubMed, Ovid Medline, SPORTDiscus, Cochrane Central Register of Controlled Trials and hand searches of reference lists. All the searches were performed in April 2020.
Eligibility criteria for selected studies
Studies included an investigation of immediate versus delayed reporting or early versus late presentation following a concussion, were published in the past ten years, and were level 4 evidence or higher.
Results
12 studies were included. Patients who continued play or delayed reporting their concussion had significantly longer recovery times (standardized mean difference = 0.36 days (95%CI 0.066, 0.662) than those who immediately reported or were removed from play (p = 0.017). Expressed in raw scores, those who immediately reported recovered in 5.4 days (95% CI − 10.14, − 0.75) fewer than delayed reporters. Comparable results were found for post-concussion symptom scores (p = 0.034) with immediate reporters demonstrating lower symptom severity scores. Our qualitative synthesis found patients who presented earlier to a concussion specialist tended to recover faster than those who presented later.
Conclusions
Patients who delayed reporting or continued play had longer recovery times compared to their immediately-reporting peers. Providers should ask concussion patients approximately how long they waited to report their injury, and also focus educational efforts on encouraging immediate reporting of concussion.


Similar content being viewed by others
Availability of data and material
The data that support the findings of this study are available on request from the corresponding author [TVM].
References
McCrea M, Broglio S, McAllister T, Zhou W, Zhao S, Katz B, et al. Return to play and risk of repeat concussion in collegiate football players: comparative analysis from the NCAA Concussion Study (1999–2001) and CARE Consortium (2014–2017). Br J Sports Med. 2019:bjsports-2019–100579. https://doi.org/10.1136/bjsports-2019-100579.
McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838. https://doi.org/10.1136/bjsports-2017-097699.
Makdissi M, Schneider KJ, Feddermann-Demont N, Guskiewicz KM, Hinds S, Leddy JJ, et al. Approach to investigation and treatment of persistent symptoms following sport-related concussion: a systematic review. Br J Sports Med. 2017;51(12):958–68. https://doi.org/10.1136/bjsports-2016-097470.
McCrea M, Guskiewicz K, Randolph C, Barr WB, Hammeke TA, Marshall SW, et al. Incidence, clinical course, and predictors of prolonged recovery time following sport-related concussion in high school and college athletes. J Int Neuropsychol Soc. 2013;19(1):22–33. https://doi.org/10.1017/S1355617712000872.
Asken BM, McCrea MA, Clugston JR, Snyder AR, Houck ZM, Bauer RM. “Playing through it”: delayed reporting and removal from athletic activity after concussion predicts prolonged recovery. J Athl Train. 2016;51(4):329–35. https://doi.org/10.4085/1062-6050-51.5.02.
Kontos AP, Elbin RJ, Sufrinko A, Marchetti G, Holland CL, Collins MW. Recovery following sport-related concussion: integrating pre-and postinjury factors into multidisciplinary care. J Head Trauma Rehabil. 2019;34(6):394–401.
Meehan WP 3rd, Mannix RC, O’Brien MJ, Collins MW. The prevalence of undiagnosed concussions in athletes. Clin J Sport Med. 2013;23(5):339–42. https://doi.org/10.1097/JSM.0b013e318291d3b3.
Iverson GL, Gardner AJ, Terry DP, Ponsford JL, Sills AK, Broshek DK, et al. Predictors of clinical recovery from concussion: a systematic review. Br J Sports Med. 2017;51(12):941–8. https://doi.org/10.1136/bjsports-2017-097729.
Zemek R, Barrowman N, Freedman SB, Gravel J, Gagnon I, McGahern C, et al. Clinical risk score for persistent postconcussion symptoms among children with acute concussion in the ED. JAMA. 2016;315(10):1014–25. https://doi.org/10.1001/jama.2016.1203.
Asken BM, Bauer RM, Guskiewicz KM, McCrea MA, Schmidt JD, Giza CC, et al. Immediate removal from activity after sport-related concussion is associated with shorter clinical recovery and less severe symptoms in collegiate student-athletes. Am J Sports Med. 2018;46(6):1465–74. https://doi.org/10.1177/0363546518757984.
Charek DB, Elbin RJ, Sufrinko A, Schatz P, D’Amico NR, Collins MW, et al. Preliminary evidence of a dose-response for continuing to play on recovery time after concussion. J Head Trauma Rehabil. 2020;35(2):85–91.
Elbin RJ, Sufrinko A, Schatz P, French J, Henry L, Burkhart S, et al. Removal from play after concussion and recovery time. Pediatrics. 2016;138(3):1–8. https://doi.org/10.1542/peds.2016-0910.
Heyer GL, Schaffer CE, Rose SC, Young JA, McNally KA, Fischer AN. Specific factors influence postconcussion symptom duration among youth referred to a sports concussion clinic. J Pediatr. 2016;174:33–8.
Howell DR, OBrien MJ, Fraser J, Meehan WP. Continuing play, symptom severity, and symptom duration after concussion in youth athletes. Clin J Sport Med. 2020;30(1):42–6. https://doi.org/10.1097/JSM.0000000000000570.
Kontos AP, Jorgensen-Wagers K, Trbovich AM, Ernst N, Emami K, Gillie B, et al. Association of time since injury to the first clinic visit with recovery following concussion. JAMA Neurol. 2020;77(4):435–40.
Bookbinder HA, Houston MN, Peck KY, Habecker S, Colsant BJ, Kelly TF, et al. Factors associated with delayed concussion reporting by United States Service Academy cadets. J Athl Train. 2020. https://doi.org/10.4085/1062-6050-362-19.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. https://doi.org/10.1136/bmj.b2700.
OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine (OCEBM): University of Oxford; 2011
Stang A. Critial evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Zynda AJ, Sabatino MJ, Ellis HB, Miller SM. Continued play following sport-related concussion in United States youth soccer. Intl J Exerc Sci. 2020;13(6):87–100.
Bock S, Grim R, Barron TF, Wagenheim A, Hu YE, Hendell M, et al. Factors associated with delayed recovery in athletes with concussion treated at a pediatric neurology concussion clinic. Childs Nerv Syst. 2015;31(11):2111–6. https://doi.org/10.1007/s00381-015-2846-8.
Desai N, Wiebe DJ, Corwin DJ, Lockyer JE, Grady MF, Master CL. Factors affecting recovery trajectories in pediatric female concussion. Clin J Sport Med. 2019;29(5):361–7.
Eagle SR, Puligilla A, Fazio-Sumrok V, Kegel N, Collins MW, Kontos AP. Association of time to initial clinic visit with prolonged recovery in pediatric patients with concussion. J Neurosurg Pediatr. 2020;1:1–6. https://doi.org/10.3171/2020.2.Peds2025.
Kara S, Crosswell H, Forch K, Cavadino A, McGeown J, Fulcher M. Less than half of patients recover within 2 weeks of injury after a sports-related mild traumatic brain injury: a 2-year prospective study. Clin J Sport Med. 2020;30(2).
McCrea M, Guskiewicz KM, Marshall SW, Barr W, Randolph C, Cantu RC, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2556–63. https://doi.org/10.1001/jama.290.19.2556.
Register-Mihalik J, Baugh C, Kroshus E, Z YK, Valovich McLeod TC. A multifactorial approach to sport-related concussion prevention and education: application of the socioecological framework. J Athl Train. 2017;52(3):195–205. https://doi.org/10.4085/1062-6050-51.12.02.
Chrisman SP, Quitiquit C, Rivara FP. Qualitative study of barriers to concussive symptom reporting in high school athletics. J Adol Health. 2013;52(3):330–5.
Baugh CM, Kroshus E, Daneshvar DH, Stern RA. Perceived coach support and concussion symptom-reporting: differences between freshmen and non-freshmen college football players. J Law Med Ethics. 2014;42(3):314–22. https://doi.org/10.1111/jlme.12148.
Register-Mihalik JK, Williams RM, Marshall SW, Linnan LA, Mihalik JP, Guskiewicz KM, et al. Demographic, parental, and personal factors and youth athletes’ concussion-related knowledge and beliefs. J Athl Train. 2018;53(8):768–75.
Wayment HA, Huffman AH. The indirect influence of organizational safety climate on football players’ concussion reporting intentions. Health Ed Behav. 2020;47(1):91–100. https://doi.org/10.1177/1090198119879216.
Warmath D, Winterstein AP. Reporting Skill: the missing ingredient in concussion reporting intention assessment. Sports Health. 2019;11(5):416–24. https://doi.org/10.1177/1941738119856609.
Weber Rawlins ML, Johnson BR, Register-Mihalik JK, DeAngelis K, Schmidt JD, D’Lauro CJ. United States Air Force Academy cadets’ perceived costs of concussion disclosure. Mil Med. 2019. https://doi.org/10.1093/milmed/usz162.
Kroshus E, Cameron KL, Coatsworth JD, D’Lauro C, Kim E, Lee K, et al. Improving concussion education: consensus from the NCAA-Department of Defense Mind Matters Research & Education Grand Challenge. Br J Sports Med. 2020;54(22):1314–20. https://doi.org/10.1136/bjsports-2020-102185.
Shahab I, Meili R. Examining non-attendance of doctor’s appointments at a community clinic in Saskatoon. Can Fam Phys. 2019;65(6):e264–8.
Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611–20. https://doi.org/10.1016/j.puhe.2015.04.001.
Leddy JJ, Haider MN, Hinds AL, Darling S, Willer BS. A preliminary study of the effect of early aerobic exercise treatment for sport-related concussion in males. Clin J Sport Med. 2019;29(5)
Leddy JJ, Haider MN, Ellis MJ, Mannix R, Darling SR, Freitas MS, et al. Early subthreshold aerobic exercise for sport-related concussion: a randomized clinical trial. JAMA Pediatr. 2019;173(4):319–25. https://doi.org/10.1001/jamapediatrics.2018.4397.
Micay R, Richards D, Hutchison MG. Feasibility of a postacute structured aerobic exercise intervention following sport concussion in symptomatic adolescents: a randomised controlled study. BMJ Open Sport Exerc Med. 2018;4(1):e000404. https://doi.org/10.1136/bmjsem-2018-000404.
Langevin P, Frémont P, Fait P, Dubé MO, Bertrand-Charette M, Roy JS. Aerobic exercise for sport-related concussion: a systematic review and meta-analysis. Med Sci Sports Exerc. 2020. https://doi.org/10.1249/mss.0000000000002402.
Willer BS, Haider MN, Bezherano I, Wilber CG, Mannix R, Kozlowski K, et al. Comparison of rest to aerobic exercise and placebo-like treatment of acute sport-related concussion in male and female adolescents. Arch Phys Med Rehabil. 2019;100(12):2267–75. https://doi.org/10.1016/j.apmr.2019.07.003.
Author information
Authors and Affiliations
Contributions
MB and TVM contributed to the conception and design, search strategy and data extraction, and wrote the first draft of the manuscript. CB analyzed and interpreted the meta-analyses. CB and TVM revised the original manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of interest
Mitchell Barnhart, R. Curtis Bay and Tamara C. Valovich McLeod declare that they have no conflicts of interest relevant to the content of this review.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The data that support the findings of this study are available on request from the corresponding author [TVM].
Code availability
Not applicable.
Rights and permissions
About this article
Cite this article
Barnhart, M., Bay, R.C. & Valovich McLeod, T.C. The Influence of Timing of Reporting and Clinic Presentation on Concussion Recovery Outcomes: A Systematic Review and Meta-Analysis. Sports Med 51, 1491–1508 (2021). https://doi.org/10.1007/s40279-021-01444-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-021-01444-7