Abstract
Purpose of Review
Fine particle (PM2.5) levels have been decreasing in the USA over the past decades. Our goal was to assess the current literature to characterize the association between PM2.5 and adverse health at low exposure levels.
Recent Findings
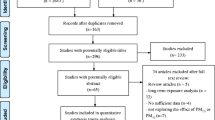
We reviewed 26 papers that examined the association between short- and long-term exposure to PM2.5 and cardio-respiratory morbidity and mortality. There is evidence suggesting that these associations are stronger at lower levels. However, there are certain methodological and interpretational limitations specific to studies of low PM2.5 levels, and further methodological development is warranted.
Summary
There is strong agreement across studies that air pollution effects on adverse health are still observable at low concentrations, even well below current US standards. These findings suggest that US standards need to be reevaluated, given that further improving air quality has the potential of benefiting public health.


Similar content being viewed by others
Abbreviations
- Tot m:
-
total mortality
- CVD m:
-
cardiovascular mortality
- CHF m:
-
Congestive Heart failure mortality
- IHD m:
-
Ischemic heart disease mortality
- Circul m:
-
Circulatory mortality
- Resp m:
-
Respiratory mortality
- COPD m:
-
COPD mortality
- Pneum m:
-
Pneumonia mortality
- CLRD m:
-
Chronic lower respiratory disease mortality
- Tot HA:
-
total hospital admissions
- CVD HA:
-
cardiovascular hospital admissions
- CVD EV:
-
cardiovascular Emergency Visits
- Resp EV:
-
Respiratory Emergency Visits
- Resp HA:
-
Respiratory hospital admissions
- Circul HA:
-
Circulatory hospital admissions
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Samet JM. The clean air act and health — a clearer view from 2011. N Engl J Med. 2011;365:198–201.
•• Di Q, Wang Y, Zanobetti A, Wang Y, Koutrakis P, Choirat C, et al. Air Pollution and Mortality in the Medicare Population. N Engl J Med [Internet]. Massachusetts Medical Society; 2017 [cited 2019 Jan 10];376:2513–22. Available from: http://www.nejm.org/doi/10.1056/NEJMoa1702747. Largest national study of the association between long-term PM 2.5 and mortality. Estimated both effects at low concentrations and the concentration-response function at low concentrations.
Di Q, Dai L, Wang Y, Zanobetti A, Choirat C, Schwartz JD, et al. Association of short-term exposure to air pollution with mortality in older adults. JAMA - J Am Med Assoc. 2017;318:2446–56.
Dominici F, Peng RD, Bell ML, Pham L, McDermott A, Zeger SL, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. JAMA. 2006;295(10):1127–34.
Hoek G, Krishnan RM, Beelen R, Peters A, Ostro B, Brunekreef B, et al. Long-term air pollution exposure and cardio- respiratory mortality: a review. Environ Health [Internet]. 2013;12:43. https://doi.org/10.1186/1476-069X-12-43.
Zanobetti A, Schwartz J. The effect of fine and coarse particulate air pollution on mortality: a national analysis. Environ Health Perspect [Internet]. 2009;117:898–903 Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19590680.
Crouse DL, Philip S, Van Donkelaar A, Martin RV, Jessiman B, Peters PA, et al. A new method to jointly estimate the mortality risk of long-term exposure to fine particulate matter and its components. Sci Rep. 2016;6:18916. https://doi.org/10.1038/srep18916
Weichenthal S, Pinault LL, Burnett RT. Impact of oxidant gases on the relationship between outdoor fine particulate air pollution and nonaccidental, cardiovascular, and respiratory mortality. Sci Rep. 2017;7(1):16401. https://doi.org/10.1038/s41598-017-16770-y
Jerrett M, Turner MC, Beckerman BS, Pope CA, van Donkelaar A, Martin RV, et al. Comparing the health effects of ambient particulate matter estimated using ground-based versus remote sensing exposure estimates. Environ Health Perspect. 2017;125:552–9.
Pun VC, Kazemiparkouhi F, Manjourides J, Suh HH. Long-Term PM2.5 Exposure and Respiratory, Cancer, and Cardiovascular Mortality in Older US Adults. Am J Epidemiol [Internet]. Oxford University Press; 2017 [cited 2019 Jan 5];186:961–9. Available from: https://academic.oup.com/aje/article/186/8/961/3852285.
Garcia CA, Yap PS, Park HY, Weller BL. Association of long-term PM2.5 exposure with mortality using different air pollution exposure models: impacts in rural and urban California. Int J Environ Health Res. 2016;26:145–57.
Schwartz J, Austin E, Bind MA, Zanobetti A, Koutrakis P. Estimating causal associations of fine particles with daily deaths in Boston. Am J Epidemiol. 2015;182:644–50.
Yoo EH, Brown P, Eum Y. Ambient air quality and spatio-temporal patterns of cardiovascular emergency department visits. Int J Health Geogr. 2018;17:18.
Hao Y, Balluz L, Strosnider H, Wen XJ, Li C, Qualters JR. Ozone, fine particulate matter, and chronic lower respiratory disease mortality in the United States. Am J Respir Crit Care Med. 2015;192:337–41.
Rodopoulou S, Samoli E, Chalbot MCG, Kavouras IG. Air pollution and cardiovascular and respiratory emergency visits in Central Arkansas: a time-series analysis. Sci Total Environ. 2015;536:872–9.
DeVries R, Kriebel D, Sama S. Low level air pollution and exacerbation of existing COPD: a case crossover analysis. Environ Health. 2016;15(1):98.
Makar M, Antonelli J, Di Q, Cutler D, Schwartz J, Dominici F. Estimating the causal effect of low levels of fine particulate matter on hospitalization. Epidemiology. 2017;28:627–34.
Wang Y, Shi L, Lee M, Liu P, Di Q, Zanobetti A, et al. Long-term exposure to PM 2.5 and mortality among older adults in the southeastern US. Epidemiology. 2017;28:207–14.
Schwartz J, Fong K, Zanobetti A. A national multicity analysis of the causal effect of local pollution, NO2, and PM2:5 on mortality. Environ Health Perspect. 2018;126:087004.
Schwartz J, Bind MA, Koutrakis P. Estimating causal effects of local air pollution on daily deaths: effect of low levels. Environ Health Perspect. 2017;125:23–9.
Lee M, Koutrakis P, Coull B, Kloog I, Schwartz J. Acute effect of fine particulate matter on mortality in three southeastern states from 2007-2011. J Expo Sci Environ Epidemiol. 2016;26:173–9.
•• Shi L, Zanobetti A, Kloog I, Coull BA, Koutrakis P, Melly SJ, et al. Low-concentration PM2.5and mortality: estimating acute and chronic effects in a population-based study. Environ Health Perspect. 2016;124:46–52 Estimated simultaneously the short- and long-term PM 2.5 effects on mortality. In addition, the authors estimated both the effects at low concentrations and the concentration-response function.
Crouse DL, Peters PA, Hystad P, Brook JR, van Donkelaar A, Martin RV, et al. Ambient PM2.5, O3, and NO2 exposures and associations with mortality over 16 years of follow-up in the Canadian census health and environment cohort (CanCHEC). Environ Health Perspect. 2015;123:1180–6.
Pinault L, Tjepkema M, Crouse DL, Weichenthal S, Van Donkelaar A, Martin RV, et al. Risk estimates of mortality attributed to low concentrations of ambient fine particulate matter in the Canadian community health survey cohort. Environ Health. 2016;15:18. https://doi.org/10.1186/s12940-016-0111-6.
Pinault LL, Weichenthal S, Crouse DL, Brauer M, Erickson A, van Donkelaar A, et al. Associations between fine particulate matter and mortality in the 2001 Canadian Census Health and Environment Cohort. Environ Res [Internet]. Academic Press; 2017 [cited 2019 Jan 5];159:406–15. Available from: https://www.sciencedirect.com/science/article/pii/S0013935117305480.
Weichenthal S, Kulka R, Lavigne E, van Rijswijk D, Brauer M, Villeneuve PJ, et al. Biomass burning as a source of ambient fine particulate air pollution and acute myocardial infarction. Epidemiology. 2017;28:329–37.
Villeneuve PJ, Weichenthal SA, Crouse D, Miller AB, To T, Martin RV, et al. Long-term exposure to fine particulate matter air pollution and mortality among Canadian women. Epidemiology. 2015;26:536–45.
Thurston GD, Ahn J, Cromar KR, Shao Y, Reynolds HR, Jerrett M, et al. Ambient particulate matter air pollution exposure and mortality in the NIH-AARP diet and health cohort. Environ Health Perspect. 2016;124:484–90.
Lim CC, Hayes RB, Ahn J, Shao Y, Silverman DT, Jones RR, Garcia C, Thurston GD Association between long-term exposure to ambient air pollution and diabetes mortality in the US. Environ Res [Internet]. 2018 [cited 2019 Feb 13];165:330–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29778967.
Hart JE, Liao X, Hong B, Puett RC, Yanosky JD, Suh H, et al. The association of long-term exposure to PM2.5 on all-cause mortality in the nurses’ health study and the impact of measurement-error correction. Environ Health. 2015;14:38. https://doi.org/10.1186/s12940-015-0027-6
US EPA O. Downscaler model for predicting daily air pollution. [cited 2019 Feb 13]; Available from: https://www.epa.gov/air-research/downscaler-model-predicting-daily-air-pollution..
Nasari MM, Szyszkowicz M, Chen H, Crouse D, Turner MC, Jerrett M, et al. A class of non-linear exposure-response models suitable for health impact assessment applicable to large cohort studies of ambient air pollution. Air Qual Atmos Heal [Internet]. Springer Netherlands; 2016 [cited 2019 Jan 5];9:961–72. Available from: http://link.springer.com/10.1007/s11869-016-0398-z.
Papadogeorgou G, Dominici F. A causal exposure response function with local adjustment for confounding: a study of the health effects of long-term exposure to low levels of fine particulate matter. 2018 [cited 2019 Apr 9]; Available from: http://arxiv.org/abs/1806.00928.
Kioumourtzoglou M-A, Austin E, Koutrakis P, Dominici F, Schwartz J, Zanobetti A. PM2.5 and survival among older adults: effect modification by particulate composition. Epidemiology [internet]. 2015 [cited 2015 Apr 1]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/25738903.
Dai L, Zanobetti A, Koutrakis P, Schwartz JD. Associations of fine particulate matter species with mortality in the United States: a multicity time-series analysis. Environ Health Perspect. 2014;122:837–42.
Austin E, Coull BA, Zanobetti A, Koutrakis P. A framework to spatially cluster air pollution monitoring sites in US based on the PM2.5 composition. Environ Int [Internet]. 2013 [cited 2013 Sep 16];59:244–54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23850585.
Wu X, Braun D, Kioumourtzoglou M-A, Choirat C, Di Q, Dominici F. Causal inference in the context of an error prone exposure: air pollution and mortality. Ann Appl Stat. 2019;13(1):520–47
Zeger SL, Thomas D, Dominici F, Samet JM, Schwartz J, Dockery D, et al. Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect. 2000;108:419–26.
Kioumourtzoglou MA, Spiegelman D, Szpiro AA, Sheppard L, Kaufman JD, Yanosky JD, et al. Exposure measurement error in PM2.5 health effects studies: a pooled analysis of eight personal exposure validation studies. Environ Health. 2014;13(1):2. https://doi.org/10.1186/1476-069X-13-2.
Szpiro AA, Paciorek CJ. Measurement error in two-stage analyses, with application to air pollution epidemiology. Environmetrics. 2013;24:501–17.
Gryparis A, Paciorek CJ, Zeka A, Schwartz J, Coull BA. Measurement error caused by spatial misalignment in environmental epidemiology. Biostatistics. 2009;10:258–74.
Pope CA, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manage Assoc. 2006;56:709–42.
Schwartz J, Laden F, Zanobetti A. The concentration-response relation between PM2.5and daily deaths. Environ Health Perspect. 2002;110:1025–9.
Pope CA. Invited commentary: particulate matter-mortality exposure-response relations and threshold. Am J Epidemiol. 2000;152:407–12.
Bell ML, Ebisu K. Environmental inequality in exposures to airborne particulate matter components in the United States. Environ Health Perspect [Internet]. 2012 [cited 2018 May 27];120:1699–704. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22889745.
Kioumourtzoglou MA, Schwartz J, James P, Dominici F, Zanobetti A. PM2.5 and mortality in 207 US cities: modification by temperature and city characteristics. Epidemiology. 2016;27(2):221–7. https://doi.org/10.1097/EDE.0000000000000422
Bell ML, Zanobetti A, Dominici F. Evidence on Vulnerability and Susceptibility to Health Risks Associated With Short-Term Exposure to Particulate Matter: A Systematic Review and Meta-Analysis. Am J Epidemiol [Internet]. 2013 [cited 2013 Sep 16];178:865–76. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23887042.
Burnett RT, Pope CA, Ezzati M, Olives C, Lim SS, Mehta S, et al. An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environ Health Perspect [Internet]. National Institute of Environmental Health Science; 2014 [cited 2019 Feb 13];122:397–403. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24518036.
Pope CA, Cohen AJ, Burnett RT. Cardiovascular disease and fine particulate matter lessons and limitations of an integrated exposure-response approach. Circ Res. 2018;122:1645–7.
Burnett R, Chen H, Szyszkowicz M, Fann N, Hubbell B, Pope CA, et al. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc Natl Acad Sci U S A [Internet]. National Academy of Sciences; 2018 [cited 2019 Feb 13];115:9592–7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30181279.
Vodonos A, Awad YA, Schwartz J. The concentration-response between long-term PM2.5 exposure and mortality; a meta-regression approach. Environ Res. 2018;166:677–89.
Funding
National Institutes of Health NIH/NIEHS grants P30 ES000002, P30 ES009089, and R01 ES024332; HEI grant 4953-RFA14-3/16-4. Research described in this article was conducted under contract to the Health Effects Institute (HEI), an organization jointly funded by the United States Environmental Protection Agency (EPA) (Assistance Award No.CR-83467701) and certain motor vehicle and engine manufacturers. The contents of this article do not necessarily reflect the views of HEI, or its sponsors, nor do they necessarily reflect the views and policies of the EPA or motor vehicle and engine manufacturers.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Air Pollution and Health
Rights and permissions
About this article
Cite this article
Papadogeorgou, G., Kioumourtzoglou, MA., Braun, D. et al. Low Levels of Air Pollution and Health: Effect Estimates, Methodological Challenges, and Future Directions. Curr Envir Health Rpt 6, 105–115 (2019). https://doi.org/10.1007/s40572-019-00235-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-019-00235-7