Abstract
Purpose
Correct resection of the tibial bone in total ankle replacement (TAR) procedure is crucial for accurate TAR implant positioning and the avoidance of post-operative complications. However, the biomechanical influence of the resection depth of tibial bone for TAR is not clearly understood. Therefore, the objective of this study is to investigate the biomechanical characteristics of the distal tibia with different resection depths after primary TAR.
Methods
Tibial bone models of eight healthy volunteers (age 27 ± 3.83 years old, 5 Males and 3 females) were constructed and 6 to 16 mm resection depths of each bone were performed under the guidance of senior foot and ankle surgeons. A 4 mm tibial plate was reversed engineering to completely cover the bone resection surface. And finite element analyses were performed to evaluate the biomechanical behavior of these models. 5.2 times of body weight was applied as a worst-case scenario loading condition and element-based material assignment was used for the tibial bone. The resection surface area, resection volume, von Mises stress, and strain at each resection surface were analyzed.
Results
As bone resection depth increased from 6 to 16 mm, the resection surface area decreased from 1125.25\(\pm\)99.76 \({\text{m}\text{m}}^{2}\)to 889.27\(\pm\)101.08 \({\text{m}\text{m}}^{2}\), while the resection volume increased from 14701\(\pm\)4376.30 \({\text{m}\text{m}}^{3}\) to 25116\(\pm\)3354.27 \({\text{m}\text{m}}^{3}\). The biomechanical simulation results showed average von Mises stress increased from 3.46\(\pm\)1.06 MPa to 3.85\(\pm\)0.43 MPa. The average strain increased with the resection depth, from 5.11\(\pm\)1.577 microstrain to 5.68\(\pm\)1.87 microstrain (reach the highest points at 8 to 10 mm resection depth), then decreased to 4.62\(\pm\)1.26 microstrain. Both the stress and strain were mainly distributed peripherally.
Conclusion
As the resection depth was increased in the tibia during TAR, the resection surface area decreased but the resection volume and stress at the surface increased. The strain at the resection surface increased first and then decreased which reached a plateau at 8 to 10 mm resection depth. The 8 to 10 mm above the tibial plafond may be the weakest region of bone support in the distal tibia, which should be avoided in the design tibial component for TAR.






Similar content being viewed by others
Data Availability
The datasets supporting the conclusions of this article are included within the article and its Supplementary Material.
Abbreviations
- TAR:
-
Total Ankle Replacement.
- CT:
-
CT:Computed Tomography.
- MPa:
-
Megapascals.
- STL:
-
Stereolithography.
- FDA:
-
Food and Drug Administration.
- 3D:
-
Three-dimensional.
References
Zhao, D., Huang, D., Zhang, G., Wang, X., Zhang, T., & Ma, X. (2020). Positive and negative factors for the treatment outcomes following total ankle arthroplasty? A systematic review. Foot And Ankle Surgery, Jan;26(1), 1–13. https://doi.org/10.1016/j.fas.2018.12.003
Gross, C. E., Palanca, A. A., & DeOrio, J. K. (2018). Design Rationale for Total Ankle Arthroplasty Systems: An Update. Journal of the American Academy of Orthopaedic Surgeons, 26(10), 353–359. https://doi.org/10.5435/JAAOS-D-16-00715
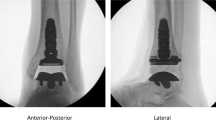
Integra LifeSciences (2021). -03-01) CADENCE Total Ankle System Surgical Technique. from https://cadenceankle.com/
STAR total ankle system operative technique from https://footankle.stryker.com/en/products/total-ankle-replacements/star-ankle
Wright Medical Group N.V. INBONE II total ankle system surgical technique. from http://www.totalankleinstitute.com/INBONE-Products/INBONE-ANKLE/
Wright Medical Group N.V. INFINITY Total Ankle System Surgical technique. from http://www.totalankleinstitute.com/INFINITY-Products/INFINITY-ANKLE/
Hvid, I., Rasmussen, O., Jensen, N. C., & Nielsen, S. (1985). Trabecular bone strength profiles at the ankle joint. Clinical Orthopaedics And Related Research, 199, 306–312
Bischoff, J. E., Schon, L., & Saltzman, C. (2017). Influence of Geometry and Depth of Resections on Bone Support for Total Ankle Replacement. Foot & ankle international, 38(9), 1026–1034. https://doi.org/10.1177/1071100717712508
Zhang, Q. H., Cossey, A., & Tong, J. (2016). Stress shielding in periprosthetic bone following a total knee replacement: Effects of implant material, design and alignment. Medical Engineering & Physics, 38(12), 1481–1488. https://doi.org/10.1016/j.medengphy.2016.09.018
Lee, R. W., Volz, R. G., & Sheridan, D. C. (1991). The role of fixation and bone quality on the mechanical stability of tibial knee components.Clin Orthop Relat Res(273):177–183
Wang, S., Wang, B., Lan, X., Xu, Z., Huang, H., Wang, X. … Ma, J. (2021). Application of a Personalized Finite Element Analysis and 3D-Printed Navigation Template in the Treatment of Femoral Neck Fracture with Cannulated Screw. Journal of Medical and Biological Engineering, 41(6), 934–941. https://doi.org/10.1007/s40846-021-00667-3
Xu, J. H., Tu, Z. X., Xu, J. X., Zhang, S. Y., & Tan, J. R. (2021). Biomechanical Strengthening Design for Limb Articulation Based on Reconstructed Skeleton Kinesthetics. Journal of Medical and Biological Engineering, 41(5), 715–729. https://doi.org/10.1007/s40846-021-00645-9
Terrier, A., Larrea, X., Guerdat, J., & Crevoisier, X. (2014). Development and experimental validation of a finite element model of total ankle replacement. Journal of Biomechanics, 47(3), 742–745. https://doi.org/10.1016/j.jbiomech.2013.12.022
Sopher, R. S., Amis, A. A., Calder, J. D., & Jeffers, J. R. T. (2017). Total ankle replacement design and positioning affect implant-bone micromotion and bone strains. Medical Engineering & Physics, 42, 80–90. https://doi.org/10.1016/j.medengphy.2017.01.022
Zhao, D. H., Huang, D. C., Zhang, G. H., Fan, Y. P., & Ma, X. (2019). Talar Dome Investigation and Talocrural Joint Axis Analysis Based on Three-Dimensional (3D) Models: Implications for Prosthetic Design. BioMed Research International, 2019, 1–10. https://doi.org/10.1155/2019/8634159
Linde, F., Hvid, I., & Madsen, F. (1992). The effect of specimen geometry on the mechanical behaviour of trabecular bone specimens. Journal of Biomechanics, 25(4), 359–368
Carter, D. R., & Hayes, W. C. (1977). The compressive behavior of bone as a two-phase porous structure.JBJS, 59(7)
Mondal, S., & Ghosh, R. (2019). The Effects of Implant Orientations and Implant–Bone Interfacial Conditions on Potential Causes of Failure of Tibial Component Due to Total Ankle Replacement. Journal of Medical and Biological Engineering, 39(4), 541–551. https://doi.org/10.1007/s40846-018-0435-5
Linde, F., Hvid, I., & Madsen, F. (1992). The effect of specimen geometry on the mechanical behaviour of trabecular bone specimens. Journal of Biomechanics, 25(4), 359–368. https://doi.org/10.1016/0021-9290(92)90255-Y
Mondal, S., & Ghosh, R. (2017). A numerical study on stress distribution across the ankle joint: Effects of material distribution of bone, muscle force and ligaments. Journal of orthopaedics, 14(3), 329–335. https://doi.org/10.1016/j.jor.2017.05.003
Seireg, A., & Arvikar, R. J. (1975). The prediction of muscular load sharing and joint forces in the lower extremities during walking. Journal of Biomechanics, 8(2), 89–102. https://doi.org/10.1016/0021-9290(75)90089-5
FDA SUMMARY OF SAFETY AND EFFECTIVENESS (SSED) of Scandinavian Total Ankle Replacement System (STAR Ankle) from https://www.accessdata.fda.gov/cdrh_docs/pdf5/P050050b.pdf
FDA SUMMARY OF SAFETY AND EFFECTIVENESS DATA (SSED) of Hintermann Series H3 Total Ankle Replacement System from https://www.accessdata.fda.gov/cdrh_docs/pdf16/P160036B.pdf
Tuncer, M., Cobb, J. P., Hansen, U. N., & Amis, A. A. (2013). Validation of multiple subject-specific finite element models of unicompartmental knee replacement. Medical Engineering & Physics, 35(10), 1457–1464. https://doi.org/10.1016/j.medengphy.2013.03.020
Terrier, A., Fernandes, C. S., Guillemin, M., & Crevoisier, X. (2017). Fixed and mobile-bearing total ankle prostheses: Effect on tibial bone strain. Clinical biomechanics (Bristol Avon), 48, 57–62. https://doi.org/10.1016/j.clinbiomech.2017.07.009
Acknowledgements
None.
Funding
This project was supported by Natural Science Foundation of Shanghai (Grant No. 19ZR1407400), Clinical Research Plan of SHDC (Grant No. SHDC2020CR3071B), and Science and Technology Commission of Shanghai Municipality (Grant No. 21511102200).
Author information
Authors and Affiliations
Contributions
J.Y. and D.Z. contributed equally. J.Y. and D.Z. performed the finite element analysis, drafted the manuscript and designed the figures. J.Y. and S.W. aided in interpreting the results and worked on the manuscript. S.W., C.Z. and J.H. performed the measurements, X.M. and X.W. were involved in planning and supervised the work. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institute’s ethical committee (Approval letter No. 2021 − 457).
Consent for publication
Participants enrolled into the study agreed the use of data for research.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yu, J., Zhao, D., Wang, S. et al. Finite Element Analysis of the Biomechanical Effect of Bone Resection Depth in the Distal Tibia after Total Ankle Replacement. J. Med. Biol. Eng. 42, 422–428 (2022). https://doi.org/10.1007/s40846-022-00722-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-022-00722-7