Abstract
Purpose
To assess the effect of demineralized cortical fibers (DCF) on postoperative pseudarthrosis requiring revision surgery in patients undergoing pedicle subtraction osteotomy (PSO) for adult spinal deformity (ASD).
Methods
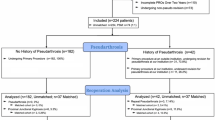
The use of DCF was introduced across all procedures in 2017 and subsequent patients undergoing PSO surgery were prospectively and consecutively registered. Following sample-size estimation, a retrospective cohort was also registered undergoing the same procedure immediately prior to the implementation of DCF. The non-DCF group underwent surgery with ABG. Minimum follow-up was 2 years in both groups. The main outcome was postoperative pseudarthrosis, either CT-verified or verified intraoperatively during revision surgery due to rod breakage and assessed using Kaplan–Meier survival analyses.
Results
A total of 48 patients were included in the DCF group and 76 in the non-DCF group. The DCF group had more frequently undergone previous spine surgery (60% vs 36%) and had shorter follow-up (32 ± 2 vs 40 ± 7 months). Pseudarthrosis occurred in 7 (15%) patients in the DCF group and 31 (41%) in the non-DCF group, corresponding to a relative risk increase of 2.6 (95%CI 1.3–2.4, P < 0.01). 1-KM survival analyses, taking time to event into account and thus the difference in follow-up, also showed increased pseudarthrosis in the non-DCF group (log-rank P = 0.022). Similarly, multivariate logistic regression adjusted for age, instrumented levels and sacral fusion was also with significantly increased odds of pseudarthrosis in the non-DCF group (OR: 4.3, 95%CI: 1.7–11.3, P < 0.01).
Conclusion
We found considerable and significant reductions in pseudarthrosis following PSO surgery with DCF compared to non-DCF.
Level of evidence
III.




Similar content being viewed by others
References
Pellisé F, Vila-Casademunt A, Ferrer M et al (2014) Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J 24:3–11. https://doi.org/10.1007/s00586-014-3542-1
Good CR, Auerbach JD, O’Leary PT, Schuler TC (2011) Adult spine deformity. Curr Rev Musculoskelet Med 4:159–167. https://doi.org/10.1007/s12178-011-9101-z
Ames CP, Scheer JK, Lafage V et al (2016) Adult spinal deformity: epidemiology, health impact, evaluation, and management. Spine Deform 4:310–322. https://doi.org/10.1016/j.jspd.2015.12.009
Everett CR, Patel RK (2007) A systematic literature review of nonsurgical treatment in adult scoliosis. Spine (Phila Pa 1976) 32:S130–S134. https://doi.org/10.1097/BRS.0b013e318134ea88
Scheer JK, Hostin R, Robinson C et al (2018) Operative management of adult spinal deformity results in significant increases in QALYs gained compared to nonoperative management. Spine (Phila Pa 1976) 43:339–347. https://doi.org/10.1097/BRS.0000000000001626
Smith JS, Shaffrey CI, Berven S et al (2009) Improvement of back pain with operative and nonoperative treatment in adults with scoliosis. Neurosurgery 65:86–94. https://doi.org/10.1227/01.NEU.0000347005.35282.6C
Smith JS, Shaffrey CI, Berven S et al (2009) Operative versus nonoperative treatment of leg pain in adults with scoliosis. Spine (Phila Pa 1976) 34:1693–1698. https://doi.org/10.1097/BRS.0b013e3181ac5fcd
Yadla S, Maltenfort MG, Ratliff JK, Harrop JS (2010) Adult scoliosis surgery outcomes: a systematic review. Neurosurg Focus 28:E3. https://doi.org/10.3171/2009.12.FOCUS09254
Charosky S, Guigui P, Blamoutier A et al (2012) Complications and risk factors of primary adult scoliosis surgery. Spine (Phila Pa 1976) 37:693–700. https://doi.org/10.1097/BRS.0b013e31822ff5c1
Sciubba DM, Yurter A, Smith JS et al (2015) A comprehensive review of complication rates after surgery for adult deformity: a reference for informed consent. Spine Deform 3:575–594. https://doi.org/10.1016/j.jspd.2015.04.005
Smith JS, Klineberg E, Lafage V et al (2016) Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. J Neurosurg Spine 25:1–14. https://doi.org/10.3171/2015.11.SPINE151036
Silber JS, Anderson DG, Daffner SD et al (2003) Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 28:134–139. https://doi.org/10.1097/00007632-200301150-00008
Sawin PD, Traynelis VC, Menezes AH (1998) A comparative analysis of fusion rates and donor-site morbidity for autogeneic rib and iliac crest bone grafts in posterior cervical fusions. J Neurosurg 88:255–265. https://doi.org/10.3171/jns.1998.88.2.0255
Younger EM, Chapman MW (1989) Morbidity at bone graft donor sites. J Orthop Trauma 3:192–195. https://doi.org/10.1097/00005131-198909000-00002
Wildemann B, Kadow-Romacker A, Haas NP, Schmidmaier G (2007) Quantification of various growth factors in different demineralized bone matrix preparations. J Biomed Mater Res Part A 81A:437–442. https://doi.org/10.1002/jbm.a.31085
Plantz MA, Hsu WK (2020) Recent research advances in biologic bone graft materials for spine surgery. Curr Rev Musculoskelet Med 13:318–325. https://doi.org/10.1007/s12178-020-09620-4
Fu T-S, Wang I-C, Lu M-L et al (2016) The fusion rate of demineralized bone matrix compared with autogenous iliac bone graft for long multi-segment posterolateral spinal fusion. BMC Musculoskelet Disord 17:3. https://doi.org/10.1186/s12891-015-0861-2
Aghdasi B, Montgomery SR, Daubs MD, Wang JC (2013) A review of demineralized bone matrices for spinal fusion: the evidence for efficacy. Surg 11:39–48. https://doi.org/10.1016/j.surge.2012.08.001
Han S, Park B, Lim J-W et al (2020) Comparison of fusion rate between demineralized bone matrix versus autograft in lumbar fusion: meta-analysis. J Korean Neurosurg Soc. https://doi.org/10.3340/jkns.2019.0185
Buser Z, Brodke DS, Youssef JA et al (2018) Allograft versus demineralized bone matrix in instrumented and noninstrumented lumbar fusion: a systematic review. Glob Spine J 8:396–412. https://doi.org/10.1177/2192568217735342
Russell N, Walsh WR, Lovric V et al (2020) In-vivo performance of seven commercially available demineralized bone matrix fiber and putty products in a rat posterolateral fusion model. Front Surg 7:1–11. https://doi.org/10.3389/fsurg.2020.00010
Lee KJH, Roper JG, Wang JC (2005) Demineralized bone matrix and spinal arthrodesis. Spine J 5:S217–S223. https://doi.org/10.1016/j.spinee.2005.02.006
Martin GJ, Boden SD, Titus L, Scarborough NL (1999) New formulations of demineralized bone matrix as a more effective graft alternative in experimental posterolateral lumbar spine arthrodesis. Spine (Phila Pa 1976) 24:637–645. https://doi.org/10.1097/00007632-199904010-00005
Street JT, Lenehan BJ, DiPaola CP et al (2012) Morbidity and mortality of major adult spinal surgery. A prospective cohort analysis of 942 consecutive patients. Spine J 12:22–34. https://doi.org/10.1016/j.spinee.2011.12.003
Karstensen S, Bari T, Gehrchen M et al (2016) Morbidity and mortality of complex spine surgery: a prospective cohort study in 679 patients validating the Spine AdVerse Event Severity (SAVES) system in a European population. Spine J 16:146–153. https://doi.org/10.1016/j.spinee.2015.09.051
Bari TJ, Karstensen S, Sørensen MD et al (2019) Readmission following complex spine surgery in a prospective cohort of 679 patients – 2-years follow up using the Spine AdVerse Event Severity (SAVES) system. Spine J. https://doi.org/10.1016/j.spinee.2019.12.004
Bari TJ, Karstensen S, Sørensen MD et al (2020) Revision surgery and mortality following complex spine surgery: 2-year follow-up in a prospective cohort of 679 patients using the Spine AdVerse Event Severity (SAVES) system. Spine Deform. https://doi.org/10.1007/s43390-020-00164-8
Maillot C, Ferrero E, Fort D et al (2015) Reproducibility and repeatability of a new computerized software for sagittal spinopelvic and scoliosis curvature radiologic measurements: Keops®. Eur Spine J 24:1574–1581. https://doi.org/10.1007/s00586-015-3817-1
R Core Team (2020) R: A Language and Environment for Statistical Computing
Gerds TA (2019) prodlim: Product-limit estimation for censored event history analysis
Therneau TM (2020) A Package for Survival Analysis in R
Therneau TM, Grambsch PM (2000) Modeling survival data: extending the {C}ox model. Springer, New York
Wickham H (2016) ggplot2: elegant graphics for data analysis. Springer, New York
Rampersaud YR, Neary MA, White K (2010) Spine Adverse Events Severity System. Spine (Phila Pa 1976) 35:790–795. https://doi.org/10.1097/BRS.0b013e3181bf25a3
Rampersaud YR, Anderson PA, Dimar JR, Fisher CG (2016) Spinal adverse events severity system, version 2 (SAVES-V2): inter- and intraobserver reliability assessment. J Neurosurg Spine 25:256–263. https://doi.org/10.3171/2016.1.SPINE14808
Paul JC, Lonner BS, Vira S et al (2016) Use of recombinant bone morphogenetic protein is associated with reduced risk of reoperation after spine fusion for adult spinal deformity. Spine (Phila Pa 1976) 41:E15–E21. https://doi.org/10.1097/BRS.0000000000001173
Kim HJ, Buchowski JM, Zebala LP et al (2013) RhBMP-2 is superior to iliac crest bone graft for long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976) 38:1209–1215. https://doi.org/10.1097/BRS.0b013e31828b656d
Poorman GW, Jalai CM, Boniello A et al (2017) Bone morphogenetic protein in adult spinal deformity surgery: a meta-analysis. Eur Spine J 26:2094–2102. https://doi.org/10.1007/s00586-016-4841-5
Glassman SD, Carreon LY, Campbell MJ et al (2008) The perioperative cost of Infuse bone graft in posterolateral lumbar spine fusion. Spine J 8:443–448. https://doi.org/10.1016/j.spinee.2007.03.004
Louie PK, Hassanzadeh H, Singh K (2014) Epidemiologic trends in the utilization, demographics, and cost of bone morphogenetic protein in spinal fusions. Curr Rev Musculoskelet Med 7:177–181. https://doi.org/10.1007/s12178-014-9222-2
Zadegan SA, Abedi A, Jazayeri SB et al (2017) Demineralized bone matrix in anterior cervical discectomy and fusion: a systematic review. Eur Spine J 26:958–974. https://doi.org/10.1007/s00586-016-4858-9
Pichelmann MA, Lenke LG, Bridwell KH et al (2010) Revision rates following primary adult spinal deformity surgery. Spine (Phila Pa 1976) 35:219–226. https://doi.org/10.1097/BRS.0b013e3181c91180
Funding
No external funding was received.
Author information
Authors and Affiliations
Contributions
TJB: Substantial contributions to the conception or design of the work. Substantial contributions to the acquisition, analysis and interpretation of data. Revising the work critically for important intellectual content. Final approval of the version to be published. Agree to be accountable for all aspects of the work. LVH: Substantial contributions to the conception or design of the work. Revising the work critically for important intellectual content. Final approval of the version to be published. Agree to be accountable for all aspects of the work. BD: Substantial contributions to the conception or design of the work. Revising the work critically for important intellectual content. Final approval of the version to be published. Agree to be accountable for all aspects of the work. MG: Substantial contributions to the conception or design of the work. Revising the work critically for important intellectual content. Final approval of the version to be published. Agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
BD (consulting fees from K2M outside of the submitted work), MG (institutional grants from K2M and Medtronic outside of the submitted work), the remaining authors report no conflicts of interest.
Ethical approval
This study was approved by the National Health and Medical authority and The National Data Protection Agency.
Informed consent
This study includes no experimental investigation.
Availability of data
Data are not available under local data protection law.
Code availability
Can be made available upon reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bari, T.J., Hansen, L.V., Dahl, B. et al. Use of demineralized cortical fibers is associated with reduced risk of pseudarthrosis after pedicle subtraction osteotomy for adult spinal deformity. Spine Deform 10, 657–667 (2022). https://doi.org/10.1007/s43390-021-00444-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00444-x