Abstract
Purpose
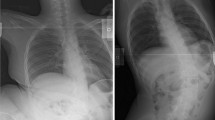
Intraoperative traction (ITx) has been demonstrated to be a useful adjunct intervention at the time of posterior spinal fusion (PSF) for the treatment of severe neuromuscular scoliosis (NMS) to improve the coronal spinal deformity and pelvic obliquity. The purpose of this study is to determine if preoperative flexibility radiographs can predict the amount of spinal deformity and pelvic obliquity correction at final follow-up.
Methods
This was a retrospective analysis of a single-surgeon series who underwent PSF to the pelvis with adjunct ITx for NMS. Database query identified 76 NMS patients, of which 41 met inclusion criteria. Demographic, radiographic and operative data were analyzed.
Results
Of the 41 study patients, 56% (n = 23) were male and mean age at surgery was 13.6 years. Mean follow-up of 4.1 years (minimum follow-up 2 years). 35 patients had cerebral palsy, 5 patients were syndromic, and 1 patient had myelomeningocele. The average preoperative weight was 35 kg and all were wheelchair ambulators. Total traction applied on average was 49% of the preoperative body weight. Mean preoperative coronal deformity was 91° which improved to 43° at final follow-up (53% correction). Push-supine imaging had the strongest correlation to major coronal deformity outcome at final follow-up (r2 = 0.87, p ≤ 0.0001). Compared to push-supine imaging, there was a mean greater coronal deformity correction of 18 ± 10° (p ≤ 0.0001) at final follow-up. To predict the final coronal deformity, the regression equation was final Cobb angle = 1.13085 + preop push-supine Cobb angle × 0.68830. Mean preoperative pelvic obliquity was 34° which improved to 12° at final follow-up (65% correction). Push-supine imaging had the strongest correlation to pelvic obliquity outcome at final follow-up (r2 = 0.59, p = 0.0001). Compared to push-supine imaging, there was a mean greater pelvic obliquity correction of 3 ± 10° (p = 0.0857) at final follow-up. The regression equation was final POB = 6.42096 + preop push-supine POB × 0.36675. Mean preoperative kyphosis was 70° and 52° at final follow-up (26% correction).
Conclusion
The results of this study demonstrated for preoperative planning that the push-supine flexibility radiograph is most predictive of the coronal deformity and of the pelvic obliquity correction. At final follow-up in this NMS population, there was a mean greater improvement of 18° for coronal deformity versus preoperative push-supine imaging and 3° for pelvic obliquity versus preoperative push-supine imaging. At the time of PSF, ITx is an effective adjunct technique to improve coronal deformity and POB for NMS producing 53% coronal correction, 65% POB correction, and 26% kyphosis correction.
Level of evidence
IV.



Similar content being viewed by others
References
Benson ER, Thomson JD, Smith BG, Banta JV (1998) Results and morbidity in a consecutive series of patients undergoing spinal fusion for neuromuscular scoliosis. Spine (Phila Pa 1976) 23:2308–2317 (discussion 18)
Drummond D, Breed AL, Narechania R (1985) Relationship of spine deformity and pelvic obliquity on sitting pressure distributions and decubitus ulceration. J Pediatr Orthop 5:396–402
Majd ME, Muldowny DS, Holt RT (1997) Natural history of scoliosis in the institutionalized adult cerebral palsy population. Spine (Phila Pa 1976) 22:1461–1466
Comstock CP, Leach J, Wenger DR (1998) Scoliosis in total-body-involvement cerebral palsy. Analysis of surgical treatment and patient and caregiver satisfaction. Spine (Phila Pa 1976) 23:1412–1424 (discussion 24–5)
Thometz JG, Simon SR (1988) Progression of scoliosis after skeletal maturity in institutionalized adults who have cerebral palsy. J Bone Jt Surg Am 70:1290–1296
Stevens DB, Beard C (1989) Segmental spinal instrumentation for neuromuscular spinal deformity. Clin Orthop Relat Res 242:164–168
Sarwark J, Sarwahi V (2007) New strategies and decision making in the management of neuromuscular scoliosis. Orthop Clin N Am 38:485–496 (v)
Swank SM, Cohen DS, Brown JC (1989) Spine fusion in cerebral palsy with L-rod segmental spinal instrumentation. A comparison of single and two-stage combined approach with Zielke instrumentation. Spine (Phila Pa 1976) 14:750–759
Lonstein JE, Akbarnia A (1983) Operative treatment of spinal deformities in patients with cerebral palsy or mental retardation. An analysis of one hundred and seven cases. J Bone Jt Surg Am 65:43–55
Keeler KA, Lenke LG, Good CR et al (2010) Spinal fusion for spastic neuromuscular scoliosis: is anterior releasing necessary when intraoperative halo-femoral traction is used? Spine (Phila Pa 1976) 35:E427–E433
Boachie-Adjei O, Lonstein JE, Winter RB et al (1989) Management of neuromuscular spinal deformities with Luque segmental instrumentation. J Bone Jt Surg Am 71:548–562
Gau YL, Lonstein JE, Winter RB, Koop S, Denis F (1991) Luque-Galveston procedure for correction and stabilization of neuromuscular scoliosis and pelvic obliquity: a review of 68 patients. J Spinal Disord 4:399–410
Mohamad F, Parent S, Pawelek J et al (2007) Perioperative complications after surgical correction in neuromuscular scoliosis. J Pediatr Orthop 27:392–397
Rinella A, Lenke L, Whitaker C et al (2005) Perioperative halo-gravity traction in the treatment of severe scoliosis and kyphosis. Spine (Phila Pa 1976) 30:475–482
Takeshita K, Lenke LG, Bridwell KH et al (2006) Analysis of patients with nonambulatory neuromuscular scoliosis surgically treated to the pelvis with intraoperative halo-femoral traction. Spine (Phila Pa 1976) 31:2381–2385
Fuhrhop SK, Keeler KA, Oto M et al (2013) Surgical treatment of scoliosis in non-ambulatory spastic quadriplegic cerebral palsy patients: a matched cohort comparison of unit rod technique and all-pedicle screw constructs. Spine Deform 1:389–394
O’Brien M, Kuklo T, Blanke K, Lenke L (2005) Radiographic measurement manual. Spinal deformity study group. Medtronic Sofamor Danek
Bogunovic L, Lenke LG, Bridwell KH, Luhmann SJ (2013) Preoperative halo-gravity traction for severe pediatric spinal deformity: complications, radiographic correction and changes in pulmonary function. Spine Deform 1:33–39
Watanabe K, Lenke LG, Bridwell KH et al (2010) Efficacy of perioperative halo-gravity traction for treatment of severe scoliosis (>/=100 degrees). J Orthop Sci 15:720–730
Vialle R, Delecourt C, Morin C (2006) Surgical treatment of scoliosis with pelvic obliquity in cerebral palsy: the influence of intraoperative traction. Spine (Phila Pa 1976) 31:1461–1466
Hamzaoglu A, Ozturk C, Aydogan M et al (2008) Posterior only pedicle screw instrumentation with intraoperative halo-femoral traction in the surgical treatment of severe scoliosis (>100 degrees). Spine (Phila Pa 1976) 33:979–983
Erdem MN, Oltulu I, Karaca S, Sari S, Aydogan M (2018) Intraoperative halo-femoral traction in surgical treatment of adolescent idiopathic scoliosis curves between 70 degrees and 90 degrees: is it effective? Asian Spine J 12:678–685
Auerbach JD, Spiegel DA, Zgonis MH et al (2009) The correction of pelvic obliquity in patients with cerebral palsy and neuromuscular scoliosis: is there a benefit of anterior release prior to posterior spinal arthrodesis? Spine (Phila Pa 1976) 34:E766–E774
MacEwen GD, Bunnell WP, Sriram K (1975) Acute neurological complications in the treatment of scoliosis. A report of the Scoliosis Research Society. J Bone Jt Surg Am 57:404–408
Lenke LG, Sugrue PA, Bridwell KH et al (2015) Paper #14 the radiographic and clinical impact of preoperative halo-gravity traction in the treatment of early-onset spinal deformity. Spine Deformity 3:617–618
Barsoum WK, Mayerson J, Bell GR (1999) Cranial nerve palsy as a complication of operative traction. Spine (Phila Pa 1976) 24:585–586
Wilkins C, MacEwen GD (1977) Cranial nerve injury from halo traction. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-197707000-00015
Saleh H, Yohe N, Razi A, Saleh A (2018) Efficacy and complications of the use of Gardner-Wells Tongs: a systematic review. J Spine Surg 4:123–129
Grundy DJ (1983) Skull traction and its complications. Injury 15:173–177
Choo JH, Liu WY, Kumar VP (1996) Complications from the Gardner-Wells tongs. Injury 27:512–513
Acknowledgements
The author would like to acknowledge his research mentor, Dr. Scott Luhmann, the NIH for providing stipend funding, and the Washington University Office of Medical Student Research for helping to make this possible.
Funding
NIH Grant T35HL007815-25, Washington University Summer Research Program.
Author information
Authors and Affiliations
Contributions
Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work: TB and SJL. Drafting the work or revising it critically for important intellectual content: TB and SJL. Final approval of the version to be published: TB and SJL. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: TB and SJL.
Corresponding author
Ethics declarations
Conflict of interest
No conflicts exist for any of the authors pertaining to the submitted work.
Ethical approval
No human subjects or animals participated therefore no informed consent was obtained. IRB approval was obtained from Washington University Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bane, T., Luhmann, S.J. Predicting the impact of intraoperative halo-femoral traction from preoperative imaging in neuromuscular scoliosis. Spine Deform 10, 679–687 (2022). https://doi.org/10.1007/s43390-021-00461-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-021-00461-w