Abstract
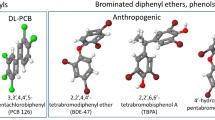
During the period of mass industrial production of plastic products, the quality of human health has decreased significantly, especially in children’s neurodevelopmental disorders. Phthalates are endocrine-disrupting chemicals that can induce neurological disorders. This review aims to compile evidence concerning the associations between neurological disorders, such as attention-deficit/hyperactivity disorder, autism spectrum disorder, decreased masculine behavior, and phthalate exposure. Phthalates dysregulate the hypothalamic–pituitary–gonadal, adrenal, and thyroid axis, which is crucial for the neurodevelopmental process. Phthalates interfere with nuclear receptors in various neural structures involved in controlling brain functions and the onset of neurological disorders at the intracellular level. It is critical to increase the current knowledge concerning phthalates’ toxicity mechanism to comprehend their harmful effect on human health.




Similar content being viewed by others
Abbreviations
- ACTH:
-
Adrenocorticotropic hormone
- ADHD:
-
Attention deficit hyperactivity disorder
- ASD:
-
Autism spectrum disorders
- BBzP:
-
Benzylbutyl phthalate
- CRH:
-
Corticotropin-releasing hormone
- CBG:
-
Corticosteroid-binding globulin
- DBP:
-
Dibutyl phthalate
- DCHP:
-
Dicyclohexyl phthalate
- DEHP:
-
Di(2-ethylhexyl) phthalate
- DEP:
-
Diethyl phthalate
- DiBP:
-
Di-iso-butyl phthalate
- DiDP:
-
Di-iso-decyl phthalate
- DiNP:
-
Di-iso-nonyl phthalate
- DMP:
-
Dimethyl phthalate
- DnBP:
-
Di-n-butyl phthalate
- DnOP:
-
Di-n-octyl phthalate
- ED:
-
Endocrine-disrupting chemical
- ER:
-
Estrogen receptor
- FSH:
-
Follicle-stimulating hormone
- FT3:
-
Free triiodothyronine
- FT4:
-
Free thyroxine
- GnRH:
-
Gonadotropin-releasing hormone
- GR:
-
Glucocorticoid receptor
- HMWP:
-
High-molecular-weight phthalate
- HPA:
-
Hypothalamic–pituitary–adrenal axis
- HPG:
-
Hypothalamic–pituitary–gonadal axis
- HPT:
-
Hypothalamic–pituitary–thyroid axis
- LH:
-
Luteinizing hormone
- LMWP:
-
Low molecular weight phthalates
- MBP:
-
Monobutyl phthalate
- MBzP:
-
Monobenzyl phthalate
- MCPP:
-
Mono-(3-carboxypropyl) phthalate
- MDI:
-
Mental developmental index
- MEHHP:
-
Mono(2-ethyl-5-hydroxyhexyl) phthalate
- MEHP:
-
Mono-(2-ethylhexyl) phthalate
- MEP:
-
Monoethyl phthalate
- MECPP:
-
Mono-(2-ethyl-5-carboxypentyl) phthalate
- MEOHP:
-
Mono(2-ethyl-5-oxohexyl) phthalate
- MiBP:
-
Mono-iso-butyl phthalate
- MnBP:
-
Mono-n-butyl phthalate
- NIS:
-
Natrium iodide symporter
- NR:
-
Nuclear receptor
- PDI:
-
Psychomotor developmental index
- SHBG:
-
Sex hormone-binding globulin
- T3:
-
Triiodothyronine
- T4:
-
Thyroxine
- TT3:
-
Total triiodothyronine
- TT4:
-
Total thyroxine
- TBG:
-
Thyroxine-binding globulin
- TPO:
-
Thyroid peroxidase
- TR:
-
Thyroid receptor
- TRH:
-
Thyroid-releasing hormone
- TSH:
-
Thyroid-stimulating hormone
- TTR:
-
Transthyretin
References
CDC. Phthalates factsheet. 2017. Available from: https://www.cdc.gov/biomonitoring/Phthalates_FactSheet.html
Itoh S. Health impacts of developmental exposure to environmental chemicals. In: Kishi R, Grandjean P, editors. Current topics in environmental health and preventive medicine. Singapore: Springer; 2020. p. 554.
Testa C, Nuti F, Hayek J, De Felice C, Chelli M, Rovero P, et al. Di-(2-ethylhexyl) phthalate and autism spectrum disorders. ASN Neuro. 2012;4(4):AN20120015.
CDC. ADHD throughout the years | CDC. 2018. Available from: https://www.cdc.gov/ncbddd/adhd/timeline.html
CDC. Data and statistics on autism spectrum disorder | CDC. 2018. Available from: https://www.cdc.gov/ncbddd/autism/data.html
Xu G, Strathearn L, Liu B, Bao W. Prevalence of autism spectrum disorder among US children and adolescents, 2014–2016. JAMA. 2018;319(1):81. https://doi.org/10.1001/jama.2017.17812.
Javorac D, Đorđević AB, Anđelković M, Tatović S, Baralić K, Antonijević E, et al. Redox and essential metal status in the brain of Wistar rats acutely exposed to a cadmium and lead mixture. Arch Ind Hyg Toxicol. 2020;71(3):197–204.
Frye RE, Cakir J, Rose S, Delhey L, Bennuri SC, Tippett M, et al. Early life metal exposure dysregulates cellular bioenergetics in children with regressive autism spectrum disorder. Transl Psychiatry. 2020. https://doi.org/10.1038/s41398-020-00905-3.
Mustieles V, Fernández MF. Bisphenol A shapes children’s brain and behavior: towards an integrated neurotoxicity assessment including human data. Environ Heal A Glob Access Sci Source. 2020;19(1):1–8.
Gibson EA, Siegel EL, Eniola F, Herbstman JB, Factor-Litvak P. Effects of polybrominated diphenyl ethers on child cognitive, behavioral, and motor development. Int J Environ Res Public Health. 2018; 15. Available from: /pmc/articles/PMC6121413/?report=abstract
Bellinger DC. Environmental chemical exposures and neurodevelopmental impairments in children. Pediatr Med. 2018;1(0):9–9. Available from: http://pm.amegroups.com/article/view/4617/html
Ishido M, Masuo Y, Sayato-Suzuki J, Oka S, Niki E, Morita M. Dicyclohexylphthalate causes hyperactivity in the rat concomitantly with impairment of tyrosine hydroxylase immunoreactivity. J Neurochem. 2004;91(1):69–76. https://doi.org/10.1111/j.1471-4159.2004.02696.x.
Wang R, Xu X, Zhu Q. Pubertal exposure to di-(2-ethylhexyl) phthalate influences social behavior and dopamine receptor D2 of adult female mice. Chemosphere. 2016;144:1771–9.
Park S, Kim BN, Cho SC, Kim Y, Kim JW, Lee JY, et al. Association between urine phthalate levels and poor attentional performance in children with attention-deficit hyperactivity disorder with evidence of dopamine gene-phthalate interaction. Int J Environ Res Public Health. 2014;11(7):6743–56.
Dubois J, Dehaene-Lambertz G, Dehaene-Lambertz Fetal G, development postnatal. Fetal and postnatal development of the cortex: MRI and genetics. Brain Mapping: an encyclopedic reference. 2015;2:11–19. Available from: https://hal.archives-ouvertes.fr/hal-02436275
O’Rahilly R, Muller F. The embryonic human brain. Hoboken: Wiley; 2005. p. 360.
Kolb B, Gibb R. Brain plasticity and behaviour in the developing brain. J Can Acad Child Adolesc Psychiatry. 2011;20(4):265–76.
Mráz P, Belej K, Beňuška J, Holomáňová A, Macková M, Šteňová J. Human anatomy 2. [Anatómia človeka 2]. Slovak Academic Press; 2006. 486 p
Ikemoto S. Dopamine reward circuitry: Two projection systems from the ventral midbrain to the nucleus accumbens-olfactory tubercle complex. Brain Res Rev. 2007;56(1):27–78.
Lövblad KO, Schaller K, Isabel VM. The fornix and limbic system. Semin Ultrasound CT MRI. 2014;35(5):459–73.
Rushworth MF, Buckley MJ, Behrens TE, Walton ME, Bannerman DM. Functional organization of the medial frontal cortex. Curr Opin Neurobiol. 2007;17(2):220–7.
Stevens FL, Hurley RA, Taber KH. Anterior cingulate cortex: unique role in cognition and emotion. J Neuropsychiatry Clin Neurosci. 2011;23(2):121–5.
Fatahi Z, Haghparast A, Khani A, Kermani M. Functional connectivity between anterior cingulate cortex and orbitofrontal cortex during value-based decision making. Neurobiol Learn Mem. 2018;147:74–8.
Pooters T, Laeremans A, Gantois I, Vermaercke B, Arckens L, D’Hooge R. Comparison of the spatial-cognitive functions of dorsomedial striatum and anterior cingulate cortex in mice. PLoS ONE. 2017;12(5):e0176295.
Sant KE, Dolinoy DC, Jilek JL, Sartor MA, Harris C. Mono-2-ethylhexyl phthalate disrupts neurulation and modifies the embryonic redox environment and gene expression. Reprod Toxicol. 2016;63:32–48.
Komada M, Gendai Y, Kagawa N, Nagao T. Prenatal exposure to di(2-ethylhexyl) phthalate impairs development of the mouse neocortex. Toxicol Lett. 2016;259:69–79.
Xu Y, Agrawal S, Cook TJ, Knipp GT. Di-(2-ethylhexyl)-phthalate affects lipid profiling in fetal rat brain upon maternal exposure. Arch Toxicol. 2007;81(1):57–62.
Li X, Jiang L, Cheng L, Chen H. Dibutyl phthalate-induced neurotoxicity in the brain of immature and mature rat offspring. Brain Dev. 2014;36(8):653–60.
Smith CA, MacDonald A, Holahan MR. Acute postnatal exposure to di(2-ethylhexyl) phthalate adversely impacts hippocampal development in the male rat. Neuroscience. 2011;193:100–8.
Ipapo KN, Factor-Litvak P, Whyatt RM, Calafat AM, Diaz D, Perera F, et al. Maternal prenatal urinary phthalate metabolite concentrations and visual recognition memory among infants at 27 weeks. Environ Res. 2017;155:7–14.
Braun JM, Bellinger DC, Hauser R, Wright RO, Chen A, Calafat AM, et al. Prenatal phthalate, triclosan, and bisphenol A exposures and child visual-spatial abilities. Neurotoxicology. 2017;58:75–83. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27888119
Polanska K, Ligocka D, Sobala W, Hanke W. Phthalate exposure and child development: the polish mother and child cohort study. Early Hum Dev. 2014;90(9):477–85.
Whyatt RM, Liu X, Rauh VA, Calafat AM, Just AC, Hoepner L, et al. Maternal prenatal urinary phthalate metabolite concentrations and child mental, psychomotor, and behavioral development at 3 years of age. Environ Health Perspect. 2012;120(2):290–5.
Doherty BT, Engel SM, Buckley JP, Silva MJ, Calafat AM, Wolff MS. Prenatal phthalate biomarker concentrations and performance on the Bayley Scales of Infant Development-II in a population of young urban children. Environ Res. 2017;152:51–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27741448
Téllez-Rojo MM, Cantoral A, Cantonwine DE, Schnaas L, Peterson K, Hu H, et al. Prenatal urinary phthalate metabolites levels and neurodevelopment in children at two and three years of age. Sci Total Environ. 2013;461–462:386–90.
Jankowska A, Polańska K, Hanke W, Wesołowska E, Ligocka D, Waszkowska M, et al. Prenatal and early postnatal phthalate exposure and child neurodevelopment at age of 7 years—Polish Mother and Child Cohort. Environ Res. 2019;177:108626.
Won EK, Kim Y, Ha M, Burm E, Kim YS, Lim H, et al. Association of current phthalate exposure with neurobehavioral development in a national sample. Int J Hyg Environ Health. 2016;219(4–5):364–71.
Cho SC, Bhang SY, Hong YC, Shin MS, Kim BN, Kim JW, et al. Relationship between environmental phthalate exposure and the intelligence of school-age children. Environ Health Perspect. 2010;118(7):1027–32.
Olesen TS, Bleses D, Andersen HR, Grandjean P, Frederiksen H, Trecca F, et al. Prenatal phthalate exposure and language development in toddlers from the Odense Child Cohort. Neurotoxicol Teratol. 2018;65:34–41.
Huang PC, Tsai CH, Chen CC, Wu MT, Chen MLMK, Wang SL, et al. Intellectual evaluation of children exposed to phthalate-tainted products after the 2011 Taiwan phthalate episode. Environ Res. 2017;156:158–66. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28342962
Jankowska A, Polańska K, Koch HM, Pälmke C, Waszkowska M, Stańczak A, et al. Phthalate exposure and neurodevelopmental outcomes in early school age children from Poland. Environ Res. 2019;179:108829.
Messerlian C, Bellinger D, Mínguez-Alarcón L, Romano ME, Ford JB, Williams PL, et al. Paternal and maternal preconception urinary phthalate metabolite concentrations and child behavior. Environ Res. 2017;158:720–8.
Lien Y-J, Ku H-Y, Su P-H, Chen S-J, Chen H-Y, Liao P-C, et al. Prenatal exposure to phthalate esters and behavioral syndromes in children at 8 years of age: Taiwan Maternal and Infant Cohort Study. Environ Health Perspect. 2015;123(1):95–100. https://doi.org/10.1289/ehp.1307154.
Miodovnik A, Engel SM, Zhu C, Ye X, Soorya LV, Silva MJ, et al. Endocrine disruptors and childhood social impairment. Neurotoxicology. 2011;32(2):261–7.
Schwartzer JJ, Koenig CM, Berman RF. Using mouse models of autism spectrum disorders to study the neurotoxicology of gene-environment interactions. Neurotoxicol Teratol. 2013;36:17–35.
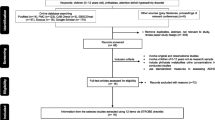
Ejaredar M, Nyanza EC, Ten Eycke K, Dewey D. Phthalate exposure and childrens neurodevelopment: a systematic review. Environ Res. 2015;142:51–60.
Holahan MR, Smith CA. Phthalates and neurotoxic effects on hippocampal network plasticity. Neurotoxicology. 2015;48:21–34.
Swan SH, Liu F, Hines M, Kruse RL, Wang C, Redmon JB, et al. Prenatal phthalate exposure and reduced masculine play in boys. Int J Androl. 2010;33(2):259–69. https://doi.org/10.1111/j.1365-2605.2009.01019.x.
Percy Z, Xu Y, Sucharew H, Khoury JC, Calafat AM, Braun JM, et al. Gestational exposure to phthalates and gender-related play behaviors in 8-year-old children: an observational study. Environ Heal A Glob Access Sci Source. 2016;15(1):1–9.
Knickmeyer RC, Baron-Cohen S. Topical review: fetal testosterone and sex differences in typical social development and in autism. J Child Neurol. 2006;21(10):825–45.
Werling DM, Geschwind DH. Sex differences in autism spectrum disorders. Curr Opin Neurol. 2013;26(2):146–53.
APA. What is autism spectrum disorder?. 2018. Available from: https://www.psychiatry.org/patients-families/autism/what-is-autism-spectrum-disorder
NIMH. Autism spectrum disorder. 2018. Available from: https://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-asd/index.shtml
Amaral DG, Schumann CM, Nordahl CW. Neuroanatomy of autism. Trends Neurosci. 2008;31:137–45.
Ha S, Sohn I-J, Kim N, Sim HJ, Cheon K-A. Characteristics of brains in autism spectrum disorder: structure, function and connectivity across the lifespan. Exp Neurobiol. 2015;24(4):273–84.
Kardas F, Bayram AK, Demirci E, Akin L, Ozmen S, Kendirci M, et al. Increased Serum Phthalates (MEHP, DEHP) and Bisphenol a concentrations in children with autism spectrum disorder. J Child Neurol. 2016;31(5):629–35. https://doi.org/10.1177/0883073815609150.
Philippat C, Bennett DH, Krakowiak P, Rose M, Hwang HM, Hertz-Picciotto I. Phthalate concentrations in house dust in relation to autism spectrum disorder and developmental delay in the CHildhood Autism Risks from Genetics and the Environment (CHARGE) study Children’s Environmental Health. Environ Heal A Glob Access Sci Source. 2015;14(1).
Stein TP, Schluter MD, Steer RA, Ming X. Autism and phthalate metabolite glucuronidation. J Autism Dev Disord. 2013;43(11):2677–85.
Jeddi MZ, Janani L, Memari AH, Akhondzadeh S, Yunesian M. The role of phthalate esters in autism development: a systematic review. Environ Res. 2016;151:493–504. https://doi.org/10.1016/j.envres.2016.08.021.
Betz AJ, Jayatilaka S, Joshi J, Ramanan S, Debartolo D, Pylypiw H, et al. Chronic exposure to benzyl butyl phthalate (BBP) alters social interaction and fear conditioning in male adult rats: alterations in amygdalar MeCP2, ERK1/2 and ERα. Neuro Endocrinol Lett. 2013;34(5):347–58.
DeBartolo D, Jayatilaka S, Yan Siu N, Rose M, Ramos RL, Betz AJ. Perinatal exposure to benzyl butyl phthalate induces alterations in neuronal development/maturation protein expression, estrogen responses, and fear conditioning in rodents. Behav Pharmacol. 2016;27(1):77–82. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26376073
Park S, Lee JM, Kim JW, Cheong JH, Yun HJ, Hong YC, et al. Association between phthalates and externalizing behaviors and cortical thickness in children with attention deficit hyperactivity disorder. Psychol Med. 2015;45(8):1601–12.
NIHM. Attention-deficit/hyperactivity disorder. 2016. Available from: https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd/index.shtml
Krain AL, Castellanos FX. Brain development and ADHD. Clin Psychol Rev. 2006;26(4):433–44.
Gehricke JG, Kruggel F, Thampipop T, Alejo SD, Tatos E, Fallon J, et al. The brain anatomy of attention-deficit/hyperactivity disorder in young adults—a magnetic resonance imaging study. PLoS ONE. 2017;12(4):e0175433.
Chopra V, Harley K, Lahiff M, Eskenazi B. Association between phthalates and attention deficit disorder and learning disability in U.S. children, 6–15 years. Environ Res. 2014;128:64–9.
Hu D, Wang YX, Chen WJ, Zhang Y, Li HH, Xiong L, et al. Associations of phthalates exposure with attention deficits hyperactivity disorder: a case-control study among Chinese children. Environ Pollut. 2017;229:375–85.
Stroustrup A, Bragg JB, Andra SS, Curtin PC, Spear EA, Sison DB, et al. Neonatal intensive care unit phthalate exposure and preterm infant neurobehavioral performance. PLoS One. 2018;13(3).
Masuo Y, Morita M, Oka S, Ishido M. Motor hyperactivity caused by a deficit in dopaminergic neurons and the effects of endocrine disruptors: a study inspired by the physiological roles of PACAP in the brain. Regul Pept. 2004;123(1–3):225–34. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0167011504001752
Tamm C, Ceccatelli S. Mechanistic insight into neurotoxicity induced by developmental insults. Biochem Biophys Res Commun. 2017;482(3):408–18.
Rock KD, Patisaul HB. Environmental mechanisms of neurodevelopmental toxicity. Curr Environ Heal Rep. 2018;5(1):145–57.
Nestler EJ, Hyman SE, Holzman DM, Malenka RC. Molecular neuropharmacology. 3rd ed. New York: McGraw-Hill Education; 2015. p. 914.
Gardill BR, Vogl MR, Lin HY, Hammond GL, Muller YA. Corticosteroid-binding globulin: structure-function implications from species differences. PLoS ONE. 2012;7(12):e52759.
Drake AJ, Tang JI, Nyirenda MJ. Mechanisms underlying the role of glucocorticoids in the early life programming of adult disease. Clin Sci. 2007;113:219–32.
Davis EP, Head K, Buss C, Sandman CA. Prenatal maternal cortisol concentrations predict neurodevelopment in middle childhood. Psychoneuroendocrinology. 2017;75:56–63. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27771566
O’Donnell K, O’Connor TG, Glover V. Prenatal stress and neurodevelopment of the child: focus on the HPA axis and role of the placenta. Dev Neurosci. 2009;31(4):285–92.
Sheikh IA, Beg MA. Endocrine disruption: in silico interactions between phthalate plasticizers and corticosteroid binding globulin. J Appl Toxicol. 2017;37(12):1471–80.
Ahmad S, Khan MF, Parvez S, Akhtar M, Raisuddin S. Molecular docking reveals the potential of phthalate esters to inhibit the enzymes of the glucocorticoid biosynthesis pathway. J Appl Toxicol. 2017;37(3):265–77. https://doi.org/10.1002/jat.3355.
Araki A, Mitsui T, Miyashita C, Nakajima T, Naito H, Ito S, et al. Association between maternal exposure to di(2-ethylhexyl) phthalate and reproductive hormone levels in fetal blood: The Hokkaido Study on environment and children’s health. PLoS ONE. 2014;9(10):e109039.
Wang DC, Chen TJ, Lin ML, Jhong YC, Chen SC. Exercise prevents the increased anxiety-like behavior in lactational di-(2-ethylhexyl) phthalate-exposed female rats in late adolescence by improving the regulation of hypothalamus-pituitary-adrenal axis. Horm Behav. 2014;66(4):674–84. Available from: https://pubmed.ncbi.nlm.nih.gov/25251977/
Sun X, Li J, Jin S, Li Y, Liu W, Zhao H, et al. Associations between repeated measures of maternal urinary phthalate metabolites during pregnancy and cord blood glucocorticoids. Environ Int. 2018;121:471–9. Available from: https://www.sciencedirect.com/science/article/pii/S0160412018315113
Nuttall JR, Kucera HR, Supasai S, Gaikwad NW, Oteiza PI. Combined effects of gestational phthalate exposure and zinc deficiency on steroid metabolism and growth. Toxicol Sci. 2017;156(2):469–79.
Srilanchakon K, Thadsri T, Jantarat C, Thengyai S, Nosoognoen W, Supornsilchai V. Higher phthalate concentrations are associated with precocious puberty in normal weight Thai girls. J Pediatr Endocrinol Metab. 2017;30(12):1293–8. Available from: http://www.degruyter.com/view/j/jpem.2017.30.issue-12/jpem-2017-0281/jpem-2017-0281.xml
Nakajin S, Shinoda S, Ohno S, Nakazawa H, Makino T. Effect of phthalate esters and alkylphenols on steroidogenesis in human adrenocortical H295R cells. Environ Toxicol Pharmacol. 2001;10(3):103–10.
Liu K, Zou C, Qin B. The association between nuclear receptors and ocular diseases. Oncotarget. 2017;8(16):27603–15.
Bramble MS, Vashist N, Vilain E. Sex steroid hormone modulation of neural stem cells: a critical review. Biol Sex Differ. 2019;10(28):1–10.
Thompson EB. Apoptosis and steroid hormones. Mol Endocirnology. 1994;8(6):665–73.
Asai D, Tahara Y, Nakai M, Yakabe Y, Takatsuki M, Nose T, et al. Structural essentials of xenoestrogen dialkyl phthalates to bind to the estrogen receptors. Toxicol Lett. 2000;118(1–2):1–8.
Brzozowski AM, Pike ACW, Dauter Z, Hubbard RE, Bonn T, Engström O, et al. Molecular basis of agonism and antagonism in the oestrogen receptor. Nature. 1997;389(6652):753–8. Available from: http://www.nature.com/articles/39645
Okamoto Y, Ueda K, Kojima N. Potential risks of phthalate esters: acquisition of endocrine-disrupting activity during environmental and metabolic processing. J Heal Sci. 2011;57(6):497–503.
Harter CJL, Kavanagh GS, Smith JT. The role of kisspeptin neurons in reproduction and metabolism. J Endocrinol. 2018;238(3):R173–83.
Cadagan D, Towlson C. Mechanisms of luteinising hormone regulation in female steroidogenesis. Am J Med Case Rep. 2017;5(3):65–8.
Casarini L, Crépieux P. Molecular mechanisms of action of FSH. Fron Endocrinol. 2019;10:305.
Jones RE, Lopez KH. Human reproductive biology. 4th ed. Amsterdam: Elsevier Inc.; 2013. p. 1–381.
Roselli CE, Liu M, Hurn PD. Brain aromatization: classic roles and new perspectives. Semin Reprod Med. 2009;27(3):207–17.
Arnold AP, Mccarthy MM. Sexual differentiation of the brain and behavior: a primer. Best Pract Res Clin Endocrinol Metab. 2016;21(3):2139–68.
Bakker J, De Mees C, Douhard Q, Balthazart J, Gabant P, Szpirer J, et al. Alpha-fetoprotein protects the developing female mouse brain from masculinization and defeminization by estrogens. Nat Neurosci. 2006;9(2):220–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16388309
Mccarthy MM. Estradiol and the developing brain. Physiol Rev. 2009;88(1):91–124.
de Bournonville C, Ball GF, Balthazart J, Cornil CA. Rapid changes in brain aromatase activity in the female quail brain following expression of sexual behaviour. J Neuroendocrinol. 2017;29(11):e12542. https://doi.org/10.1111/jne.12542.
Schwarz JM, Mccarthy MM. Cellular mechanisms of estradiol-mediated masculinization of the brain. J Steroid Biochem Mol Biol. 2008;109(3–5):300–6.
Coolen LM, Peters HJPW, Veening JG. Anatomical interrelationships of the medial preoptic area and other brain regions activated following male sexual behavior: a combined Fos and tract-tracing study. J Comp Neurol. 1998;397(3):421–35.
Hlisníková H, Petrovičová I, Kolena B, Šidlovská M, Sirotkin A. Effects and mechanisms of phthalates’ action on reproductive processes and reproductive health: a literature review. Int J Environ Res Public Health. 2020;17:1–37.
Sathyanarayana S, Butts S, Wang C, Barrett E, Nguyen R, Schwartz SM, et al. Early prenatal phthalate exposure, sex steroid hormones, and birth outcomes. J Clin Endocrinol Metab. 2017;102(6):1870–8.
Johns LE, Ferguson KK, Soldin OP, Cantonwine DE, Rivera-González LO, Del Toro AVA, et al. Urinary phthalate metabolites in relation to maternal serum thyroid and sex hormone levels during pregnancy: a longitudinal analysis. Reprod Biol Endocrinol. 2015;13(1):1–12. Available from: http://www.rbej.com/content/13/1/4
Carbone S, Samaniego YA, Cutrera R, Reynoso R, Cardoso N, Scacchi P, et al. Different effects by sex on hypothalamic-pituitary axis of prepubertal offspring rats produced by in utero and lactational exposure to di-(2-ethylhexyl) phthalate (DEHP). Neurotoxicology. 2012;33(1):78–84.
Qin X, Ma Q, Yuan J, Hu X, Tan Q, et al. The effects of di-2-ethylhexyl phthalate on testicular ultrastructure and hormone-regulated gene expression in male rats. pubs.rsc.org. 2018;7(3):408–14. Available from: https://pubs.rsc.org/en/content/articlehtml/2018/tx/c7tx00257b
Liu T, Li N, Zhu J, Yu G, Guo K, Zhou L, et al. Effects of di-(2-ethylhexyl) phthalate on the hypothalamus-pituitary-ovarian axis in adult female rats. Reprod Toxicol. 2014;46:141–7. Available from: https://www.sciencedirect.com/science/article/pii/S0890623814000501
Liu T, Jia Y, Zhou L, Wang Q, Sun D, Xu J, et al. Effects of Di-(2-ethylhexyl) Phthalate on the Hypothalamus–Uterus in Pubertal Female Rats. Int J Environ Res Public Health. 2016;13(11):1130. Available from: http://www.mdpi.com/1660-4601/13/11/1130
Ha M, Guan X, Wei L, Li P, Yang M, Liu C. Di-(2-ethylhexyl) phthalate inhibits testosterone level through disturbed hypothalamic–pituitary–testis axis and ERK-mediated 5α-Reductase 2. Sci Total Environ. 2016;563–564:566–75. Available from: https://www.sciencedirect.com/science/article/pii/S0048969716308439
Giribabu N, Sainath SB, Reddy PS. Prenatal di-n-butyl phthalate exposure alters reproductive functions at adulthood in male rats. Environ Toxicol. 2014;29(5):534–44.
Gao HT, Xu R, Cao WX, Qian LL, Wang M, Lu L, et al. Effects of six priority controlled phthalate esters with long-term low-dose integrated exposure on male reproductive toxicity in rats. Food Chem Toxicol. 2017;101:94–104.
Repouskou A, Panagiotidou E, Panagopoulou L, Bisting PL, Tuck AR, Sjödin MOD, et al. Gestational exposure to an epidemiologically defined mixture of phthalates leads to gonadal dysfunction in mouse offspring of both sexes. Sci Rep. 2019;9(1):6424. Available from: http://www.nature.com/articles/s41598-019-42377-6
Meltzer D, Martinez-Arguelles DB, Campioli E, Lee S, Papadopoulos V. In utero exposure to the endocrine disruptor di(2-ethylhexyl) phthalate targets ovarian theca cells and steroidogenesis in the adult female rat. Reprod Toxicol. 2015;51:47–56. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25530038
Liu T, Wang Y, Yang M, Shao P, Duan L, Li M, et al. Di-(2-ethylhexyl) phthalate induces precocious puberty in adolescent female rats. Iran J Basic Med Sci. 2018;21(8):848. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30186573
Sen N, Liu X, Craig ZR. Short term exposure to di-n-butyl phthalate (DBP) disrupts ovarian function in young CD-1 mice. Reprod Toxicol. 2015;53:15–22.
Martinez-Arguelles DB, Guichard T, Culty M, Zirkin BR, Papadopoulos V. In utero exposure to the antiandrogen Di-(2-ethylhexyl) phthalate decreases adrenal aldosterone production in the adult rat 1. Biol Reprod. 2011;85(1):51–61. Available from: https://pubmed.ncbi.nlm.nih.gov/21389346/
Baralić K, Djordjevic AB, Živančević K, Antonijević E, Anđelković M, Javorac D, et al. Toxic effects of the mixture of phthalates and bisphenol a—subacute oral toxicity study in Wistar rats. Int J Environ Res Public Health. 2020;17(3):1–24.
Lv Y, Dong Y, Wang Y, Zhu Q, Li L, Li X, et al. Benzyl butyl phthalate non-linearly affects rat Leydig cell development during puberty. Toxicol Lett. 2019;314:53–62.
Brehm E, Rattan S, Gao L, Flaws JA. Prenatal exposure to Di(2-ethylhexyl) phthalate causes long-term transgenerational effects on female reproduction in mice. Endocrinology. 2018;159(2):795–809.
Li N, Liu T, Guo K, Zhu J, Yu G, Wang S, et al. Effect of mono-(2-ethylhexyl) phthalate (MEHP) on proliferation of and steroid hormone synthesis in rat ovarian granulosa cells in vitro. J Cell Physiol. 2018;233(4):3629–37.
Pathirana IN, Kawate N, Tsuji M, Takahashi M, Hatoya S, Inaba T, et al. In vitro effects of estradiol-17β, monobutyl phthalate and mono-(2-ethylhexyl) phthalate on the secretion of testosterone and insulin-like peptide 3 by interstitial cells of scrotal and retained testes in dogs. Theriogenology. 2011;76(7):1227–33.
Qin X, Ma Q, Yuan J, Hu X, Tan Q, Zhang Z, et al. The effects of di-2-ethylhexyl phthalate on testicular ultrastructure and hormone-regulated gene expression in male rats. 2018;7(3):408–14. Available from: https://pubs.rsc.org/en/content/articlehtml/2018/tx/c7tx00257b
Yamaguchi T, Maeda M, Ogata K, Abe J, Utsumi T, Kimura K. The effects on the endocrine system under hepatotoxicity induction by phenobarbital and di(2-ethylhexyl)phthalate in intact juvenile male rats. J Toxicol Sci. 2019;44(7):459–69.
Zhu Y-P, Li E-H, Sun W-L, Xu D-L, Liu Z-H, Zhao W, et al. Maternal exposure to di-n-butyl phthalate (DBP) induces combined anorectal and urogenital malformations in male rat offspring. Reprod Toxicol. 2016;61:169–76. Available from: https://www.sciencedirect.com/science/article/pii/S0890623816300570
Abdel-Maksoud FM, Leasor KR, Butzen K, Braden TD, Akingbemi BT. Prenatal exposures of male rats to the environmental chemicals bisphenol A and di(2-ethylhexyl) phthalate impact the sexual differentiation process. Endocrinology. 2015;156(12):4672–83.
Hannon PR, Brannick KE, Wang W, Gupta RK, Flaws JA. Di(2-ethylhexyl) phthalate inhibits antral follicle growth, induces atresia, and inhibits steroid hormone production in cultured mouse antral follicles. Toxicol Appl Pharmacol. 2015;284(1):42–53. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25701202
Lottrup G, Andersson A-M, Leffers H, Mortensen GK, Toppari J, Skakkebaek NE, et al. Possible impact of phthalates on infant reproductive health. Int J Androl. 2006;29(1):172–80. https://doi.org/10.1111/j.1365-2605.2005.00642.x.
Wen H-J, Chen C, Wu M-T, Chen M-L, Sun C-W, Wu W, et al. Phthalate exposure and reproductive hormones and sex-hormone binding globulin before puberty – Phthalate contaminated- foodstuff episode in Taiwan. PLoS One. 2017;12(4):1–17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28410414
Sheikh IA, Turki RF, Abuzenadah AM, Damanhouri GA, Beg MA. Endocrine disruption: computational perspectives on human sex hormone-binding globulin and phthalate plasticizers. Saleem M, editor. PLoS ONE. 2016;11(3):e0151444. https://doi.org/10.1371/journal.pone.0151444.
Sheikh IA, Yasir M, Abu-Elmagd M, Dar TA, Abuzenadah AM, Damanhouri GA, et al. Human sex hormone-binding globulin as a potential target of alternate plasticizers: an in silico study. BMC Struct Biol. 2016;16:11–20.
Zhou J, Zhang H, Cohen RS, Pandey SC. Effects of estrogen treatment on expression of brain-derived neurotrophic factor and cAMP response element-binding protein expression and phosphorylation in rat amygdaloid and hippocampal structures. Neuroendocrinology. 2005;81(5):294–310.
Luine V, Frankfurt M. Interactions between estradiol, BDNF and dendritic spines in promoting memory. Neuroscience. 2013;239:34–45.
Lechan RM, Fekete C. The TRH neuron: a hypothalamic integrator of energy metabolism. Prog Brain Res. 2006;153:209–35.
Sharlin DS. Thyroid-disrupting chemicals as developmental neurotoxicants. In: Environmental factors in neurodevelopmental and neurodegenerative disorders. Amsterdam: Elsevier; 2015. p. 167–92.
Little AG. Local regulation of thyroid hormone signalling. In: Vitamins and hormones. Cambridge: Academic Press; 2018. p. 1–17.
Chakravarthy V, Ejaz S. Thyroxine-binding globulin deficiency. StatPearls Publishing; 2020. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31334994
Darrouzet E, Lindenthal S, Marcellin D, Pellequer JL, Pourcher T. The sodium/iodide symporter: state of the art of its molecular characterization. Biochim Biophys Acta. 2014;1838:244–53 Available from: http://www.ncbi.nlm.nih.gov/pubmed/23988430
Bhagavan NV, Ha C-E. Essentials of medical biochemistry: with clinical cases. 2nd ed. Massachusetts: Academic Press; 2015. p. 752.
Korevaar TIM, Muetzel R, Medici M, Chaker L, Jaddoe VW V, de Rijke YB, et al. Association of maternal thyroid function during early pregnancy with offspring IQ and brain morphology in childhood: a population-based prospective cohort study. Lancet Diabetes Endocrinol. 2016;4(1):35–43. Available from: https://www.sciencedirect.com/science/article/abs/pii/S2213858715003277
Henrichs J, Ghassabian A, Peeters RP, Tiemeier H. Maternal hypothyroxinemia and effects on cognitive functioning in childhood: How and why? Clin Endocrinol. 2013;79:152–62. https://doi.org/10.1111/cen.12227.
Howdeshell KL. A model of the development of the brain as a construct of the thyroid system. Environ Health Perspect. 2002;110(3):337–48.
Huang PC, Tsai CH, Liang WY, Li SS, Huang H Bin, Kuo PL. Early phthalates exposure in pregnant women is associated with alteration of thyroid hormones. PLoS One. 2016;11(7):e0159398. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27455052
Yao H, Han Y, Gao H, Huang K, Ge X, Xu Y, et al. Maternal phthalate exposure during the first trimester and serum thyroid hormones in pregnant women and their newborns. Chemosphere. 2016;157:42–8.
Romano ME, Eliot MN, Zoeller RT, Hoofnagle AN, Calafat AM, Karagas MR, et al. Maternal urinary phthalate metabolites during pregnancy and thyroid hormone concentrations in maternal and cord sera: the HOME Study. Int J Hyg Environ Health. 2018;221(4):623–31.
Peck JD, Robledo C, Neas B, Calafat AM, Sjodin A, Blount B, Wild R, Cowan LD. Phthalates polycyclic aromatic hydrocarbons and perchlorate associations with thyroid hormones during pregnancy: results from a Pilot Study. Epidemiology. 2008;19(6):S235.
Kuo FC, Su SW, Wu CF, Huang MC, Shiea J, Chen BH, et al. Relationship of urinary phthalate metabolites with serum thyroid hormones in pregnant women and their newborns: a prospective birth cohort in Taiwan. PLoS ONE. 2015;10(6):1–15.
Minatoya M, Naka jima S, Sasaki S, Araki A, Miyashita C, Ikeno T, et al. Effects of prenatal phthalate exposure on thyroid hormone levels, mental and psychomotor development of infants: the Hokkaido Study on Environment and Children’s Health. Sci Total Environ. 2016;565:1037–43.
Liu C, Zhao L, Wei L, Li L. DEHP reduces thyroid hormones via interacting with hormone synthesis-related proteins, deiodinases, transthyretin, receptors, and hepatic enzymes in rats. Environ Sci Pollut Res. 2015;22(16):12711–9.
Kim M, Jeong JS, Kim H, Hwang S, Park IH, Lee BC, et al. Low dose exposure to di-2-ethylhexylphthalate in Juvenile rats alters the expression of genes related with thyroid hormone regulation. Biomol Ther. 2018;26(5):512–9.
Ye H, Ha M, Yang M, Yue P, Xie Z, Liu C. Di2-ethylhexyl phthalate disrupts thyroid hormone homeostasis through activating the Ras/Akt/TRHr pathway and inducing hepatic enzymes. Sci Rep. 2017;7:1–12.
Dong J, Cong Z, You M, Fu Y, Wang Y, Wang Y, et al. Effects of perinatal di (2-ethylhexyl) phthalate exposure on thyroid function in rat offspring. Environ Toxicol Pharmacol. 2018;2019(67):53–60.
Dong X, Dong J, Zhao Y, Guo J, Wang Z, Liu M, et al. Effects of long-term in vivo exposure to di-2-ethylhexylphthalate on thyroid hormones and the tsh/tshr signaling pathways in wistar rats. Int J Environ Res Public Health. 2017;14(1):44.
Jia PP, Ma YB, Lu CJ, Mirza Z, Zhang W, Jia YF, et al. The effects of disturbance on Hypothalamus-Pituitary-Thyroid (HPT) axis in zebrafish larvae after exposure to DEHP. PLoS ONE. 2016;11(5):e0155762.
Zhang P, Guan X, Yang M, Zeng L, Liu C. Roles and potential mechanisms of selenium in countering thyrotoxicity of DEHP. Sci Total Environ. 2018;619–620:732–9.
Hansen JF, Brorson MM, Boas M, Frederiksen H, Nielsen CH, Lindström ES, et al. Phthalates are metabolised by primary thyroid cell cultures but have limited influence on selected thyroid cell functions in vitro. PLoS ONE. 2016;11(3):e0151192.
Wenzel A, Franz C, Breous E, Loos U. Modulation of iodide uptake by dialkyl phthalate plasticisers in FRTL-5 rat thyroid follicular cells. Mol Cell Endocrinol. 2005;244(1–2):63–71.
Du ZP, Feng S, Li YL, Li R, Lv J, Ren WQ, et al. Di-(2-ethylhexyl) phthalate inhibits expression and internalization of transthyretin in human placental trophoblastic cells. Toxicol Appl Pharmacol. 2020;394(81):114960.
Ishihara A, Nishiyama N, Sugiyama SI, Yamauchi K. The effect of endocrine disrupting chemicals on thyroid hormone binding to Japanese quail transthyretin and thyroid hormone receptor. Gen Comp Endocrinol. 2003;134(1):36–43. Available from: https://pubmed.ncbi.nlm.nih.gov/13129501/
Weiss JM, Andersson PL, Zhang J, Simon E, Leonards PEG, Hamers T, et al. Tracing thyroid hormone-disrupting compounds: database compilation and structure-activity evaluation for an effect-directed analysis of sediment. Anal Bioanal Chem. 2017;407(19):5625–34.
Ishihara A, Sawatsubashi S, Yamauchi K. Endocrine disrupting chemicals: interference of thyroid hormone binding to transthyretins and to thyroid hormone receptors. Mol Cell Endocrinol. 2003;199(1–2):105–17.
Duan J, Kang J, Deng T, Yang X, Chen M. Exposure to DBP and high iodine aggravates autoimmune thyroid disease through increasing the levels of IL-17 and thyroid-binding globulin in Wistar rats. Toxicol Sci. 2018;163(1):196–205.
Cavanagh JAE, Trought K, Mitchell C, Northcott G, Tremblay LA. Assessment of endocrine disruption and oxidative potential of bisphenol-A, triclosan, nonylphenol, diethylhexyl phthalate, galaxolide, and carbamazepine, common contaminants of municipal biosolids. Toxicol Vitr. 2018;48:342–9.
Prezioso G, Giannini C, Chiarelli F. Effect of thyroid hormones on neurons and neurodevelopment. Horm Res Paediatr. 2018;90(2):73–81.
Shen O, Du G, Sun H, Wu W, Jiang Y, Song L, et al. Comparison of in vitro hormone activities of selected phthalates using reporter gene assays. Toxicol Lett. 2009;191(1):9–14.
Li N, Wang D, Zhou Y, Ma M, Li J, Wang Z. Dibutyl phthalate contributes to the thyroid receptor antagonistic activity in drinking water processes. Environ Sci Technol. 2010;44(17):6863–8. https://doi.org/10.1021/es101254c.
Simon C, Onghena M, Covaci A, Van Hoeck E, Van Loco J, Vandermarken T, et al. Screening of endocrine activity of compounds migrating from plastic baby bottles using a multi-receptor panel of in vitro bioassays. Toxicol Vitr. 2016;37:121–33. Available from: https://www.sciencedirect.com/science/article/pii/S0887233316301849
Vandenberg LN, Colborn T, Hayes TB, Heindel JJ, Jacobs DR, Lee D-H, et al. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr Rev. 2012;33(3):378–455. https://doi.org/10.1210/er.2011-1050.
Diamanti-Kandarakis E, Bourguignon J-P, Giudice LC, Hauser R, Prins GS, Soto AM, et al. Endocrine-disrupting chemicals: an endocrine society scientific statement. Endocr Rev. 2009;30(4):293–342.
Acknowledgements
This study was supported by the project of the Ministry of Health of SR [2016/9-UKFN-1].
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hlisníková, H., Petrovičová, I., Kolena, B. et al. Effects and mechanisms of phthalates’ action on neurological processes and neural health: a literature review. Pharmacol. Rep 73, 386–404 (2021). https://doi.org/10.1007/s43440-021-00215-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43440-021-00215-5