Abstract
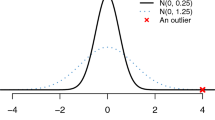
Continuity of care, and in particular provider continuity, is increasingly becoming a central aim of health care policy in a majority of clinical settings. Over the past three decades, a number of statistics have been introduced to provide a quantitative measure of continuity, but generally speaking, all existing continuity measures each reflect either the concentration of providers or the sequential continuity in a series of patient visits-none reflect both. Since concentration is often considered as important as consecutiveness, an improved index, termed the alpha index, is introduced here. In simple terms, the alpha index is a weighted average of the concentration of providers and the sequential continuity. By combining these two aspects of continuity with a user-specified weight, alpha, this new index can be more satisfactory in evaluating overall levels of continuity of care. In this article, the underlying concepts of this new measure, as well as its statistical properties such as bias and consistency, are discussed analytically. Numerical examples are given to illustrate the results.
Similar content being viewed by others
References
T. W. Bice and S. B. Boxerman. “A quantitative measure of continuity of care,” Medical Care, 15, pp. 347-349, 1977.
R. J. Blendon, R. A. Knox, M. Brodie, J. M. Benson and G. Chervinsky. “Americans compare managed care, Medicare, and fee for service,” Journal of American Health Policy, 4, pp. 42-47, 1994.
E. Branscomb, T. Slezak, R. Pae, D. Galas, A. V. Carrano and M. Waterman. “Optimizing restriction fragment fingerprinting methods for ordering large genomic libraries,” Genomics, 8, pp. 351-366, 1990.
N. Breslau and K. Reeb. “Continuity of care in a university-based practice,” Journal of Medical Education, 50, pp. 965-969, 1975.
O. Carrasquillo, D. U. Himmelstein, S. Woolhandler and D. H. Bor. “Can Medicaid managed care provide continuity of care to new Medicaid enrollees? An analysis of tenure on Medicaid,” American Journal of Public Health, 88, pp. 464-466, 1998.
A. J. Dietrich and K. I. Marton. “Does continuous care from a physician make a difference?” Journal of Family Practice, 15, pp. 929-937, 1982.
G. Ejlertsson and S. Berg. “Continuity-of-care measures: an analytic and empirical comparison,” Medical Care, 22, pp. 231-239, 1984.
E. J. Emanuel and N. N. Dubler. “Preserving the physician-patient relationship in the era of managed care,” JAMA, 273, pp. 323-329, 1995.
E. A. Eriksson. “Continuity-of-care measures: random assignment of patients to providers and the impact of utilization level,” Medical Care, 28, pp. 180-190, 1990.
E. A. Eriksson and L. G. Mattsson. “Quantitative measurement of continuity of care,” Medical Care, 21, pp. 858-875, 1983.
S. A. Flocke, K. C. Stange and S. J. Zyzanski. “The impact of insurance type and forced discontinuity on the delivery of primary care,” Journal of Family Practice, 45, pp. 129-135, 1997.
G. Freeman and P. Hjortdahl. “What future for continuity of care in general practice?” BMJ, 314, pp. 1870-1873, 1997.
J. C. Fu and W. Y. W. Lou. “On the exact distribution of SECON and its application,” Statistica Sinica, 10, pp. 999-1010, 2000.
K. Grumbach. “Continuity of insurance coverage-a precondition for continuity of primary care,” American Journal of Public Health, 88, pp. 348-349, 1998.
A. Gut. An Intermediate Course in Probability. Springer-Verlag, New York, 1995.
M. Hall and N. Tideman. “Measures of concentration,” Journal of the American Statistical Association, 62, pp. 162-168, 1967.
P. E. Hart. “Entropy and other measures of concentration,” Journal of the Royal Statistical Society, Part I, 134, pp. 73-85, 1971.
C. Hoffman, D. Rice and H. Y. Sung. “Persons with chronic conditions. Their prevalence and costs,” JAMA, 276, pp. 1473-1479, 1996.
M. S. Jellinek and B. Nurcombe. “Two wrongs don't make a right: managed care, mental health, and the marketplace,” JAMA, 270, pp. 1737-1739, 1993.
S. Kullback. Information Theory and Statistics. John Wiley, New York, 1968.
S. Kullback and R. A. Leibler. “On information and sufficiency,” Annals of Mathematical Statistics, 22, pp. 79-89, 1951.
W. Y. W. Lou. “The exact distribution of the continuity of care measure NOP,” Statistics and Probability Letters, 48, pp. 361-368, 2000.
B. Robson and R. H. Pain. “Analysis of the code relating sequence to conformation in globular proteins,” Biochemistry Journal, 141, pp. 853-867, 1974.
J. Rogers and P. Curtis. “The concept and measurement of continuity in primary care,” American Journal of Public Health, 70, pp. 122-127, 1980.
L. L. Roos, N. P. Roos, P. Gilbert and J. P. Nicol. “Continuity of care: does it contribute to quality of care?” Medical Care, 18, pp. 174-184, 1980.
S. M. Ross. Introduction to Probability Models, Fifth Edition. Academic Press, San Diego, 1993.
L. V. Rubenstein, A. Fink, E. M. Yano, B. Simon, B. Chernof and A. S. Robbins. “Increasing the impact of quality improvement on health: an expert panel method for setting institutional priorities,” The Joint Commission Journal on Quality Improvement, 21, pp. 420-432, 1995.
S. M. Shortell, “Continuity of medical care: conceptualization and measurement,” Medical Care, 14, pp. 377-391, 1976.
O. Smedby, G. Eklund, E. A. Eriksson and B. Smedby. “Measures of continuity of care: a register-based correlation study,” Medical Care, 24, pp. 511-518, 1986.
B. Starfield. “Continuous confusion?” American Journal of Public Health, 70, pp. 117-119, 1980.
D. M. Steinwachs. “Measuring provider continuity in ambulatory care,” Medical Care, 17, pp. 551-565, 1979.
M. A. Testa and D. C. Simonson. “Health economic benefits and quality of life during improved glycemic control in patients with type 2 diabetes mellitus: a randomized, controlled, double-blind trial,” JAMA, 280, pp. 1490-1496, 1998.
E. M. Wall. “Continuity of care and family medicine: definition, determinants, and relationship to outcome,” Journal of Family Practice, 13, pp. 655-664, 1981.
E. M. Wall. “Managed care and discontinuity of primary care providers: is there evidence of poorer outcomes?” Journal of Family Practice, 45, pp. 125-126, 1997.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lou, W.Y.W. A New Measure for Continuity of Care: The Alpha Index. Health Services & Outcomes Research Methodology 1, 277–289 (2000). https://doi.org/10.1023/A:1011447327152
Issue Date:
DOI: https://doi.org/10.1023/A:1011447327152