Abstract
Background
Pylorus-preserving gastrectomy (PPG) is a function-preserving gastrectomy for early gastric cancers (EGCs) that are preoperatively assessed as pN0 tumors and located in the middle portion of the stomach. In PPG, dissection of the lymph nodes at stations 5 and 6 is frequently incomplete, and this may be worrisome in terms of oncologic safety.
Methods
We examined lymph nodes collected from stations 5 and 6 from 196 patients who had undergone conventional distal gastrectomy (CDG) for EGC located in the middle portion of the stomach and from 24 patients who had undergone PPG.
Results
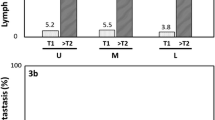
The average number of lymph nodes collected at station 5 was significantly lower with PPG than with CDG (0.08 vs. 1.32, respectively; P = 0.008). However, such a difference was not noted for station 6 nodes. The rate of macrometastasis was very low in all station 5 nodes (1 of 220, 0.45 %) and station 6 nodes (1 of 220, 0.45 %). Immunohistochemical analysis of cytokeratin in 109 cases of the CDG group and 21 cases of the PPG group showed that micrometastasis of single isolated tumor cell type was observed in only one station 6 lymph node of a patient who was initially diagnosed with pN0 EGC. There were no cases of micrometastasis in station 5 nodes.
Conclusions
The possibility of micrometastasis to station 5 and/or 6 lymph nodes may be negligible for EGC located in the middle portion of the stomach, and PPG thus might be the oncologically safe procedure when considering micrometastasis in remaining nodes in vivo at stations 5 and 6.

Similar content being viewed by others
References
Maki T, Shiratori T, Hatafuku T, Sugawara K. Pylorus-preserving gastrectomy as an improved operation for gastric ulcer. Surgery. 1967;61:838–45.
Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14:113–23.
Nunobe S, Sasako M, Saka M, Fukagawa T, Katai H, Sano T. Symptom evaluation of long-term postoperative outcomes after pylorus-preserving gastrectomy for early gastric cancer. Gastric Cancer. 2007;10:167–72.
Park do J, Lee HJ, Jung HC, Kim WH, Lee KU, Yang HK. Clinical outcome of pylorus-preserving gastrectomy in gastric cancer in comparison with conventional distal gastrectomy with Billroth I anastomosis. World J Surg. 2008;32:1029–36.
Shibata C, Shiiba KI, Funayama Y, et al. Outcomes after pylorus-preserving gastrectomy for early gastric cancer: a prospective multicenter trial. World J Surg. 2004;28:857–61.
Kong SH, Kim JW, Lee HJ, Kim WH, Lee KU, Yang HK. The safety of the dissection of lymph node stations 5 and 6 in pylorus-preserving gastrectomy. Ann Surg Oncol. 2009;16:3252–8.
Morita S, Katai H, Saka M, Fukagawa T, Sano T, Sasako M. Outcome of pylorus-preserving gastrectomy for early gastric cancer. Br J Surg. 2008;95:1131–5.
Ikeguchi M, Hatada T, Yamamoto M, et al. Evaluation of a pylorus-preserving gastrectomy for patients preoperatively diagnosed with early gastric cancer located in the middle third of the stomach. Surg Today. 2010;40:228–33.
Nitti D, Marchet A, Olivieri M, et al. Ratio between metastatic and examined lymph nodes is an independent prognostic factor after D2 resection for gastric cancer: analysis of a large European monoinstitutional experience. Ann Surg Oncol. 2003;10:1077–85.
Catalano V, Labianca R, Beretta GD, Gatta G, de Braud F, Van Cutsem E. Gastric cancer. Crit Rev Oncol Hematol. 2009;71:127–64.
Edge SB, American Joint Committee on Cancer. AJCC cancer staging manual. 7th edition. New York: Springer; 2010.
Aaltonen LA, Hamilton SR, World Health Organization, International Agency for Research on Cancer. Pathology and genetics of tumours of the digestive system. Oxford: IARC; 2000.
Arigami T, Uenosono Y, Yanagita S, et al. Clinical significance of lymph node micrometastasis in gastric cancer. Ann Surg Oncol. 2013;20:515–21.
Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–12.
Rosai J, Ackerman LV. Rosai and Ackerman’s surgical pathology. 10th edition. New York: Mosby; 2011.
Cai J, Ikeguchi M, Maeta M, Kaibara N. Micrometastasis in lymph nodes and microinvasion of the muscularis propria in primary lesions of submucosal gastric cancer. Surgery. 2000;127:32–9.
Maehara Y, Oshiro T, Endo K, et al. Clinical significance of occult micrometastasis lymph nodes from patients with early gastric cancer who died of recurrence. Surgery. 1996;119:397–402.
Morgagni P, Saragoni L, Folli S, et al. Lymph node micrometastases in patients with early gastric cancer: experience with 139 patients. Ann Surg Oncol. 2001;8:170–4.
Choi HJ, Kim YK, Kim YH, Kim SS, Hong SH. Occurrence and prognostic implications of micrometastases in lymph nodes from patients with submucosal gastric carcinoma. Ann Surg Oncol. 2002;9:13–9.
Morgagni P, Saragoni L, Scarpi E, et al. Lymph node micrometastases in early gastric cancer and their impact on prognosis. World J Surg. 2003;27:558–61.
Miyake K, Seshimo A, Kameoka S. Assessment of lymph node micrometastasis in early gastric cancer in relation to sentinel nodes. Gastric Cancer. 2006;9:197–202.
Cao L, Hu X, Zhang Y, Huang G. Adverse prognosis of clustered-cell versus single-cell micrometastases in pN0 early gastric cancer. J Surg Oncol. 2011;103:53–6.
Han KB, Jang YJ, Kim JH, et al. Clinical significance of the pattern of lymph node metastasis depending on the location of gastric cancer. J Gastric Cancer. 2011;11:86–93.
Pantel K, Brakenhoff RH, Brandt B. Detection, clinical relevance and specific biological properties of disseminating tumour cells. Nat Rev Cancer. 2008;8:329–40.
Weaver DL, Ashikaga T, Krag DN, et al. Effect of occult metastases on survival in node-negative breast cancer. N Engl J Med. 2011;364:412–21.
Kunisaki C, Akiyama H, Nomura M, et al. Significance of long-term follow-up of early gastric cancer. Ann Surg Oncol. 2006;13:363–9.
Nomura S, Kaminishi M. Surgical treatment of early gastric cancer. Dig Surg. 2007;24:96–100.
Acknowledgment
This study was supported by a faculty research grant of Yonsei University College of Medicine for 2010 (6-2010-0109).
Disclosure
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, Bh., Hong, S.W., Kim, J.W. et al. Oncologic Safety of Pylorus-preserving Gastrectomy in the Aspect of Micrometastasis in Lymph Nodes at Stations 5 and 6. Ann Surg Oncol 21, 533–538 (2014). https://doi.org/10.1245/s10434-013-3252-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-013-3252-7