Abstract
Background
Chronic pain is an important complication of breast surgery, estimated to affect 20–30% of patients. We prospectively examined surgical, demographic, and psychosocial factors associated with chronic pain 6 months after breast surgery.
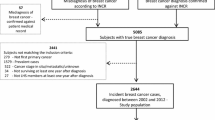
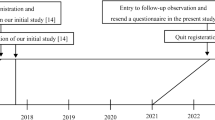
Methods
Patients undergoing breast surgery for benign and malignant disease preoperatively completed validated questionnaires to assess baseline pain and psychosocial characteristics. Pain at 6 months was quantified as the Pain Burden Index (PBI), which encompasses pain locations, severity, and frequency. Surgical type was categorized as breast-conserving surgery (BCS), mastectomy, and mastectomy with reconstruction; axillary procedure was categorized as no axillary surgery, sentinel lymph node biopsy (SLNB), and axillary dissection. PBI was compared between groups using one-way analysis of variance (ANOVA) or Kruskal–Wallis ANOVA, and the relationship between baseline demographic and psychosocial factors and PBI was assessed using Spearman’s Rank Correlation. p < 0.05 was considered significant.
Results
PBI was variable amongst patients reporting this endpoint (n = 216) at 6 months, but no difference was found between primary breast surgical types (BCS, mastectomy, and mastectomy with reconstruction) or with surgical duration. However, axillary dissection was associated with higher PBI than SLNB and no axillary procedure (p < 0.001). Younger age (< 0.001) and higher BMI (p = 0.010), as well as higher preoperative anxiety (p = 0.017), depression (p < 0.001), and catastrophizing scores (p = 0.005) correlated with higher 6-month PBI.
Conclusions
Amongst surgical variables, only axillary dissection was associated with greater pain at 6 months after surgery. Patient characteristics that were associated with higher PBI included lower age and higher BMI, as well as higher baseline anxiety, depression, and catastrophizing.


Similar content being viewed by others
References
Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367(9522):1618–25.
Brummett CM, Waljee JF, Goesling J, et al. New Persistent opioid use after minor and major surgical procedures in U.S. adults. JAMA Surg. 2017;152(6):e170504.
Duenas M, Ojeda B, Salazar A, et al. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. 2016;9:457–67.
Kulkarni AR, Pusic AL, Hamill JB, et al. Factors associated with acute postoperative pain following breast reconstruction. JPRAS Open. 2017;11:1–13.
Belfer I, Schreiber KL, Shaffer JR, et al. Persistent postmastectomy pain in breast cancer survivors: analysis of clinical, demographic, and psychosocial factors. J Pain. 2013;14(10):1185–95.
Fillingim RB. Individual differences in pain: understanding the mosaic that makes pain personal. Pain. 2017;158(Suppl 1):S11–8.
Van Damme S, Crombez G, Bijttebier P, Goubert L, Van Houdenhove B. A confirmatory factor analysis of the Pain Catastrophizing Scale: invariant factor structure across clinical and non-clinical populations. Pain. 2002;96(3):319–24.
Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7:524–32.
Cella D, Riley W, Stone A, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–94.
Choi SW, Reise SP, Pilkonis PA, et al. Efficiency of static and computer adaptive short forms compared to full length measures of depressive symptoms. Qual Life Res. 2010;19:125–35.
Gartner R, Jensen MB, Nielsen J, et al. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302(18):1985–92.
Lauridsen MC, Overgaard M, Overgaard J, et al. Shoulder disability and late symptoms following surgery for early breast cancer. Acta Oncol. 2008;47(4):569–75.
Guilliano AE, McCall L, Peitsch P, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases. Ann Surg. 2010;252(3):426–32.
Donker M, van Tienhoven G, Straver ME, Meijnen P, van de Velde CJ, Mansel RE, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomized, multicenter, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014;15(12):1303–10.
Galimberti V, Cole BF, Zurrida S, et al. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23-01): a phase 3 randomised controlled trial. Lancet Oncol. 2013;14(4):297–305.
Wilson GC, Quillin RC 3rd, Hanseman DJ, Lewis JD, Edwards MJ, Shaughnessy EA. Incidence and predictors of neuropathic pain following breast surgery. Ann Surg Oncol. 2013;20:3330–4.
Hack TF, Winkel BK, Thomas-MacLean RL, et al. Predictors of arm morbidity following breast cancer surgery. Psycho-Oncology. 2010;19:1205–12.
Andersen KG, Kehlet H. Persistent pain after breast cancer treatment: a critical review of risk factors and strategies for prevention. J Pain. 2011;12:725–46.
Schreiber KL, Kehlet H, Belfer I, Edwards RR. Predicting, preventing and managing persistent pain after breast cancer surgery: the importance of psychosocial factors. Pain Manag. 2014;4(6):445–59.
Schreiber KL, Martel MO, Shnol H, et al. Persistent pain in postmastectomy patients: comparison of psychophysical, medical, surgical, and psychosocial characteristics between patients with and without pain. Pain. 2013;154(5):660–8.
Edwards RR, Calahan C, Mensing G, et al. Pain, catastrophizing, and depression in the rheumatic diseases. Nat Rev Rheumatol. 2011;7:216–24.
Acknowledgment
This work was supported by the National Institutes of Health (NIH K23 GM110540 to KLS), and was registered at Clinicaltrials.gov.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
All authors declare that they have no conflict of interest in this study.
Rights and permissions
About this article
Cite this article
Spivey, T.L., Gutowski, E.D., Zinboonyahgoon, N. et al. Chronic Pain After Breast Surgery: A Prospective, Observational Study. Ann Surg Oncol 25, 2917–2924 (2018). https://doi.org/10.1245/s10434-018-6644-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-6644-x