Abstract
Background
Obesity and metabolic syndrome are associated with inflammatory hepatic parenchymal disease (HPD) and increased risk for recurrence after resection of colorectal liver metastases (CRLM). The independent impact of HPD on recurrence patterns has not been well defined.
Methods
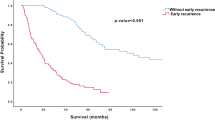
The nonalcoholic fatty liver disease activity score (NAS) was used to quantify HPD including steatosis and fibrosis for all patients with completely resected CRLM between April 2003 and March 2007. Clinicopathologic factors, perioperative history, and outcomes were compared with the NAS. Fisher’s exact test was used to examine the association between severe HPD (NAS ≥ 3) with clinical and perioperative characteristics. Kaplan–Meier methods were used to estimate recurrence-free survival (RFS). The cumulative incidences of recurrence [any intrahepatic recurrence (IHR), extrahepatic recurrence only (EHR), and death without recurrence (DWR)] were estimated using competing risks methods.
Results
Among the 357 patients included in this study, microsteatosis was noted in 124 (35%) patients, severe HPD in 31 (9%), steatohepatitis in 14 (4%), and sinusoidal injury in 36 (10%). After median follow-up of 127 months (range 4–175 months), 10-year RFS was 22% [95% confidence interval (CI) 17–27%]. Ten-year cumulative incidence for IHR, EHR, and DWR was 37%, 30%, and 12%, respectively. After controlling for confounders, NAS ≥ 3 was independently associated with higher risk of IHR [hazard ratio (HR) 1.76, 95% CI 1.07–2.90, p = 0.027] and lower risk of EHR (HR 0.18, 95% CI 0.04–0.75, p = 0.019) on multivariable analysis.
Conclusions
Severe HPD was associated with increased IHR risk and decreased EHR risk. Future investigation into whether improving HPD from reversible etiologies can reduce the risk for IHR is warranted.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34.
de Jong MC, Pulitano C, Ribero D, et al. Rates and patterns of recurrence following curative intent surgery for colorectal liver metastasis: an international multi-institutional analysis of 1669 patients. Ann Surg. 2009;250(3):440–448.
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230(3):309–318; discussion 318-321.
Nordlinger B, Guiguet M, Vaillant JC, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer. 1996;77(7):1254–1262.
Iwatsuki S, Dvorchik I, Madariaga JR, et al. Hepatic resection for metastatic colorectal adenocarcinoma: a proposal of a prognostic scoring system. J Am Coll Surg. 1999;189(3):291–299.
Margonis GA, Buettner S, Andreatos N, et al. Association of BRAF mutations with survival and recurrence in surgically treated patients with metastatic colorectal liver cancer. JAMA Surg. 2018;153(7):e180996.
Margonis GA, Sasaki K, Gholami S, et al. Genetic and morphological evaluation (GAME) score for patients with colorectal liver metastases. Br J Surg. 2018;105(9):1210–1220.
Margonis GA, Spolverato G, Kim Y, Karagkounis G, Choti MA, Pawlik TM. Effect of KRAS mutation on long-term outcomes of patients undergoing hepatic resection for colorectal liver metastases. Ann Surg Oncol. 2015;22(13):4158–4165.
Stadlmayr A, Aigner E, Steger B, et al. Nonalcoholic fatty liver disease: an independent risk factor for colorectal neoplasia. J Intern Med. 2011;270(1):41–49.
Wong VW, Wong GL, Tsang SW, et al. High prevalence of colorectal neoplasm in patients with non-alcoholic steatohepatitis. Gut. 2011;60(6):829–836.
Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346(16):1221–1231.
Diehl AM, Day C. Cause, pathogenesis, and treatment of nonalcoholic steatohepatitis. N Engl J Med. 2017;377(21):2063–2072.
Parikh ND, Marrero WJ, Wang J, et al. Projected increase in obesity and non-alcoholic-steatohepatitis-related liver transplantation waitlist additions in the United States. Hepatology. 2019;70(2):487–495.
Murono K, Kitayama J, Tsuno NH, et al. Hepatic steatosis is associated with lower incidence of liver metastasis from colorectal cancer. Int J Colorectal Dis. 2013;28(8):1065–1072.
Hamady ZZ, Rees M, Welsh FK, et al. Fatty liver disease as a predictor of local recurrence following resection of colorectal liver metastases. Br J Surg. 2013;100(6):820–826.
Molla NW, Hassanain MM, Fadel Z, et al. Effect of non-alcoholic liver disease on recurrence rate and liver regeneration after liver resection for colorectal liver metastases. Curr Oncol. 2017;24(3):e233–e243.
Wolf PS, Park JO, Bao F, et al. Preoperative chemotherapy and the risk of hepatotoxicity and morbidity after liver resection for metastatic colorectal cancer: a single institution experience. J Am Coll Surg. 2013;216(1):41–49.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41(6):1313–1321.
Rubbia-Brandt L, Audard V, Sartoretti P, et al. Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in patients with metastatic colorectal cancer. Ann Oncol. 2004;15(3):460–466.
Rubbia-Brandt L, Lauwers GY, Wang H, et al. Sinusoidal obstruction syndrome and nodular regenerative hyperplasia are frequent oxaliplatin-associated liver lesions and partially prevented by bevacizumab in patients with hepatic colorectal metastasis. Histopathology. 2010;56(4):430–439.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509.
Cholankeril G, Wong RJ, Hu M, et al. Liver transplantation for nonalcoholic steatohepatitis in the US: temporal trends and outcomes. Dig Dis Sci. 2017;62(10):2915–2922.
Rashid A, Pizer ES, Moga M, et al. Elevated expression of fatty acid synthase and fatty acid synthetic activity in colorectal neoplasia. Am J Pathol. 1997;150(1):201–208.
Zaytseva YY, Harris JW, Mitov MI, et al. Increased expression of fatty acid synthase provides a survival advantage to colorectal cancer cells via upregulation of cellular respiration. Oncotarget. 2015;6(22):18891–18904.
Pizer ES, Chrest FJ, DiGiuseppe JA, Han WF. Pharmacological inhibitors of mammalian fatty acid synthase suppress DNA replication and induce apoptosis in tumor cell lines. Cancer Res. 1998;58(20):4611–4615.
Murata S, Yanagisawa K, Fukunaga K, et al. Fatty acid synthase inhibitor cerulenin suppresses liver metastasis of colon cancer in mice. Cancer Sci. 2010;101(8):1861–1865.
Zaytseva YY, Rychahou PG, Le AT, et al. Preclinical evaluation of novel fatty acid synthase inhibitors in primary colorectal cancer cells and a patient-derived xenograft model of colorectal cancer. Oncotarget. 2018;9(37):24787–24800.
Zaytseva YY, Rychahou PG, Gulhati P, et al. Inhibition of fatty acid synthase attenuates CD44-associated signaling and reduces metastasis in colorectal cancer. Cancer Res. 2012;72(6):1504–1517.
Wen YA, Xing X, Harris JW, et al. Adipocytes activate mitochondrial fatty acid oxidation and autophagy to promote tumor growth in colon cancer. Cell Death Dis. 2017;8(2):e2593.
Zeiss J, Merrick HW, Savolaine ER, Woldenberg LS, Kim K, Schlembach PJ. Fatty liver change as a result of hepatic artery infusion chemotherapy. Am J Clin Oncol. 1990;13(2):156–160.
Vauthey JN, Pawlik TM, Ribero D, et al. Chemotherapy regimen predicts steatohepatitis and an increase in 90-day mortality after surgery for hepatic colorectal metastases. J Clin Oncol. 2006;24(13):2065–2072.
Aloia T, Sebagh M, Plasse M, et al. Liver histology and surgical outcomes after preoperative chemotherapy with fluorouracil plus oxaliplatin in colorectal cancer liver metastases. J Clin Oncol. 2006;24(31):4983–4990.
Nakano H, Oussoultzoglou E, Rosso E, et al. Sinusoidal injury increases morbidity after major hepatectomy in patients with colorectal liver metastases receiving preoperative chemotherapy. Ann Surg. 2008;247(1):118–124.
Cleary JM, Tanabe KT, Lauwers GY, Zhu AX. Hepatic toxicities associated with the use of preoperative systemic therapy in patients with metastatic colorectal adenocarcinoma to the liver. Oncologist. 2009;14(11):1095–1105.
Andreou A, Kopetz S, Maru DM, et al. Adjuvant chemotherapy with FOLFOX for primary colorectal cancer is associated with increased somatic gene mutations and inferior survival in patients undergoing hepatectomy for metachronous liver metastases. Ann Surg. 2012;256(4):642–650.
Araujo R, Gonen M, Allen P, et al. Comparison between perioperative and postoperative chemotherapy after potentially curative hepatic resection for metastatic colorectal cancer. Ann Surg Oncol. 2013;20(13):4312–4321.
Passot G, Chun YS, Kopetz SE, et al. Prognostic factors after resection of colorectal liver metastases following preoperative second-line chemotherapy: Impact of RAS mutations. Eur J Surg Oncol. 2016;42(9):1378–1384.
Kemeny N, Huang Y, Cohen AM, et al. Hepatic arterial infusion of chemotherapy after resection of hepatic metastases from colorectal cancer. N Engl J Med. 1999;341(27):2039–2048.
Kemeny NE, Gonen M. Hepatic arterial infusion after liver resection. N Engl J Med. 2005;352(7):734–735.
Bolton JS, O’Connell MJ, Mahoney MR, et al. Hepatic arterial infusion and systemic chemotherapy after multiple metastasectomy in patients with colorectal carcinoma metastatic to the liver: a North Central Cancer Treatment Group (NCCTG) phase II study, 92-46-52. Clin Colorectal Cancer. 2012;11(1):31–37.
Barth RJ, Jr., Mills JB, Suriawinata AA, et al. Short-term preoperative diet decreases bleeding after partial hepatectomy: results from a multi-institutional randomized controlled trial. Ann Surg. 2019;269(1):48–52.
Funding
This work was supported in part by the NIH/NCI P30 CA008748 Cancer Center Support Grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors have no conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Narayan, R.R., Harris, J.W., Chou, J.F. et al. Prediction of Recurrence Patterns from Hepatic Parenchymal Disease After Resection of Colorectal Liver Metastases. Ann Surg Oncol 27, 188–195 (2020). https://doi.org/10.1245/s10434-019-07934-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07934-3