Abstract
Objective
The benefit of organized breast assessment on wait times to treatment among asymptomatic women is unknown. The Ontario Breast Screening Program (OBSP) offers screening and organized assessment through Breast Assessment Centres (BAC). This study compares wait times across the treatment pathway among screened women diagnosed with breast cancer through BAC and usual care (UC).
Methods
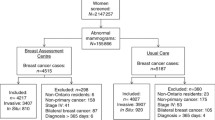
A retrospective design identified two concurrent cohorts of postmenopausal women aged 50–69 within the OBSP diagnosed with screen-detected invasive breast cancer and assessed in BAC (n = 2010) and UC (n = 1844) between 2002 and 2010. Demographic characteristics were obtained from the OBSP. Medical chart abstraction provided prognostic and treatment data. Multinomial logistic regression examined associations of assessment type with wait times from abnormal mammogram to surgery, chemotherapy or radiotherapy.
Results
Compared with through UC, postmenopausal women diagnosed through BAC were significantly less likely to have longer wait times (days) from an abnormal mammogram to definitive surgery (> 89 vs. ≤ 47; OR = 0.63; 95% CI = 0.52–0.77), from final surgery to radiotherapy (> 88 vs. ≤ 55; OR = 0.71; 95% CI = 0.54–0.93) and from final chemotherapy to radiotherapy (> 41 vs. ≤ 28; OR = 0.52; 95% CI = 0.36–0.76). Conversely, women assessed through BAC compared with through UC were more likely to experience longer wait times from final surgery to chemotherapy (> 64 vs. ≤ 40; OR = 1.49; 95% CI = 1.04–2.14).
Conclusion
Shorter wait times to most treatments for postmenopausal women diagnosed in BAC further supports that women with an abnormal mammogram should be managed through organized assessment. Continued evaluation of factors influencing wait times to treatment is essential for quality improvement and patient outcomes.
Résumé
Objectif
On ignore si l’évaluation organisée de la santé du sein réduit les délais d’attente de traitement des femmes asymptomatiques. Le Programme ontarien de dépistage du cancer du sein (PODCS) offre le dépistage et l’évaluation organisée dans des centres d’évaluation de la santé du sein (CÉSS). Notre étude compare les délais d’attente selon la voie de traitement pour les femmes ayant subi un dépistage et reçu un diagnostic de cancer du sein dans des CÉSS ou par les soins habituels (SH).
Méthode
Un protocole rétrospectif a permis de définir au sein du PODCS deux cohortes parallèles de femmes postménopausées âgées de 50 à 69 ans atteintes d’un cancer invasif du sein détecté par dépistage et évaluées dans des CÉSS (n = 2 010) et par les SH (n = 1 844) entre 2002 et 2010. Leurs caractéristiques démographiques ont été extraites du PODCS. Un résumé analytique des dossiers médicaux a fourni les données de pronostic et de traitement. Par régression logistique multinomiale, nous avons examiné les associations entre le type d’évaluation et les délais d’attente entre une mammographie anormale et la chirurgie, la chimiothérapie ou la radiothérapie.
Résultats
Comparativement à celles ayant reçu un diagnostic par les soins habituels, les femmes postménopausées ayant reçu un diagnostic dans un centre d’évaluation de la santé du sein étaient significativement moins susceptibles d’avoir enduré des délais d’attente plus longs (en jours) entre une mammographie anormale et la chirurgie définitive (> 89 c. ≤ 47; RC = 0,63; IC de 95 % = 0,52-0,77), entre la dernière chirurgie et la radiothérapie (> 88 c. ≤ 55; RC = 0,71; IC de 95 % = 0,54-0,93) et entre la dernière chimiothérapie et la radiothérapie (> 41 c. ≤ 28; RC = 0,52; IC de 95 % = 0,36-0,76). À l’inverse, les femmes évaluées dans les CÉSS étaient plus susceptibles que celles évaluées par les soins habituels d’avoir enduré des délais d’attente plus longs entre la dernière chirurgie et la chimiothérapie (> 64 c. ≤ 40; RC = 1,49; IC de 95 % = 1,04-2,14).
Conclusion
Les délais d’attente plus courts avant la plupart des traitements chez les femmes postménopausées ayant reçu un diagnostic dans un centre d’évaluation de la santé du sein constituent une preuve supplémentaire que les femmes ayant subi une mammographie anormale devraient être prises en charge par un programme d’évaluation organisé. Il est essentiel de poursuivre l’analyse des facteurs qui influent sur les délais d’attente de traitement pour améliorer la qualité des soins et l’issue pour les patientes.

Similar content being viewed by others
References
American Joint Committee on Cancer. (2002). Cancer staging manual (6th ed.). New York: Springer-Verlag.
Balduzzi, A., Leonardi, M. C., Cardillo, A., Orecchia, R., Dellapasqua, S., Iorfida, M., et al. (2010). Timing of adjuvant systemic therapy and radiotherapy after breast-conserving surgery and mastectomy. Cancer Treatment Reviews, 36(6), 443–450 Epub 2010 Mar 20.
Benk, V., Przybysz, R., McGowan, T., & Paszat, L. (2006). Waiting times for radiation therapy in Ontario. Canadian Journal of Surgery, 49(1), 16–21.
Canadian Cancer Society’s Steering Committee. Canadian Cancer Statistics. (2011). Toronto (p. 2011). ON: Canadian Cancer Society.
Cancer Care Ontario. (2010).Wait Times. from: http://www.cancercare.on.ca/cms/One.aspx?portalId=1377&pageId=8836. Accessed 04/29/2013, 2013.
Cancer Care Ontario. (2016). Ontario Cancer Screening Performance Report 2016. Toronto.
Caplan, L. S., May, D. S., & Richardson, L. C. (2000). Time to diagnosis and treatment of breast cancer: Results from the National Breast and Cervical Cancer Early Detection Program, 1991-1995. American Journal of Public Health, 90(1), 130–134.
Chen, Z., King, W., Pearcey, R., Kerba, M., & Mackillop, W. J. (2008). The relationship between waiting time for radiotherapy and clinical outcomes: a systematic review of the literature. Radiotherapy and Oncology, 87(1), 3–16 Epub 2007 Dec 21.
Chiarelli, A. M., Edwards, S. A., Prummel, M. V., Muradali, D., Majpruz, V., Done, S. J., et al. (2013). Digital compared with screen-film mammography: performance measures in concurrent cohorts within an organized breast screening program. Radiology., 268(3), 684–693.
Chiarelli, A. M., Muradali, D., Blackmore, K. M., Smith, C. R., Mirea, L., Majpruz, V., et al. (2017). Evaluating wait times from screening to breast cancer diagnosis among women undergoing organised assessment vs usual care. British Journal of Cancer, 116(10), 1254.
Hammond, M. E., Hayes, D. F., Dowsett, M., Allred, D. C., Hagerty, K. L., Badve, S., et al. (2010). American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridged version). Archives of Pathology & Laboratory Medicine, 134(7), e48–e72.
Haynes, W. (2013). Wilcoxon rank sum test. In Encyclopedia of Systems Biology (pp. 2354–2355). Berlin: Springer.
Huang, J., Barbera, L., Brouwers, M., Browman, G., & Mackillop, W. J. (2003). Does delay in starting treatment affect the outcomes of radiotherapy? A systematic review. Journal of Clinical Oncology, 21(3), 555–563.
Jaro, M. A. (1995). Probabilistic linkage of large public health data files. Statistics in Medicine, 14(5–7), 491–498.
Lohrisch, C., Paltiel, C., Gelmon, K., Speers, C., Taylor, S., Barnett, J., et al. (2006). Impact on survival of time from definitive surgery to initiation of adjuvant chemotherapy for early-stage breast cancer. Journal of Clinical Oncology, 24(30), 4888–4894 Epub 2006 Oct 2.
Olivotto, I. A., Lesperance, M. L., Truong, P. T., Nichol, A., Berrang, T., Tyldesley, S., et al. (2009). Intervals longer than 20 weeks from breast-conserving surgery to radiation therapy are associated with inferior outcome for women with early-stage breast cancer who are not receiving chemotherapy. Journal of Clinical Oncology, 27(1), 16–23 Epub 2008 Nov 17.
Ontario Breast Screening Program. (2001). Multidisciplinary Roles and Expectations for Breast Assessment in Ontario. Toronto: The Breast Assessment Collaborative Group.
Plotogea, A., Chiarelli, A. M., Mirea, L., Prummel, M. V., Chong, N., Shumak, R. S., et al. (2013). Factors associated with wait times across the breast cancer treatment pathway in Ontario. SpringerPlus, 2(1), 388. https://doi.org/10.1186/2193-1801-2-388.
Punglia, R. S., Saito, A. M., Neville, B. A., Earle, C. C., & Weeks, J. C. (2010). Impact of interval from breast conserving surgery to radiotherapy on local recurrence in older women with breast cancer: retrospective cohort analysis. Bmj., 340, c845.
Quan, M. L., Shumak, R. S., Majpruz, V., Holloway, C. M., O’Malley, F. P., & Chiarelli, A. M. (2012). Improving work-up of the abnormal mammogram through organized assessment: results from the ontario breast screening program. Journal of Oncology Practice/ American Society of Clinical Oncology, 8(2), 107–112.
Rayson, D., Chiasson, D., & Dewar, R. (2004). Elapsed time from breast cancer detection to first adjuvant therapy in a Canadian province, 1999-2000. CMAJ., 170(6), 957–961.
Rayson, D., Saint-Jacques, N., Younis, T., Meadows, J., & Dewar, R. (2007). Comparison of elapsed times from breast cancer detection to first adjuvant therapy in Nova Scotia in 1999/2000 and 2003/04. CMAJ., 176(3), 327–332.
Saint-Jacques, N., Younis, T., Dewar, R., & Rayson, D. (2007 12/1906/30/received11/10/revised11/13/accepted). Wait times for breast cancer care. British Journal of Cancer, 96(1), 162–168.
SAS Institute Inc. (2013). Statistical Analysis Software, 9.4 ed. Cary: SAS Institute.
Smith, C. R., Chiarelli, A. M., Holloway, C. M., Mirea, L., O'Malley, F. P., Blackmore, K. M., et al. (2018). The impact of organized breast assessment on survival by stage for screened women diagnosed with invasive breast cancer. The Breast, 41, 25–33.
Statistics Canada. Postal code conversion file plus (PCCF+), reference guide, 2014.
Vujovic, O., Yu, E., Cherian, A., Perera, F., Dar, A. R., Stitt, L., et al. (2009). Effect of interval to definitive breast surgery on clinical presentation and survival in early-stage invasive breast cancer. International Journal of Radiation Oncology, Biology, Physics, 75(3), 771–774.
Whelan, T. J., Julian, J., Wright, J., Jadad, A. R., & Levine, M. L. (2000). Does locoregional radiation therapy improve survival in breast cancer? A meta-analysis. Journal of Clinical Oncology, 18(6), 1220–1229 e-pub ahead of print 2000/03/15.
Whelan, T., Olivotto, I., & Levine, M. (2003). Health Canada’s Steering Committee on Clinical Practice Guidelines for the C, Treatment of Breast C. Clinical practice guidelines for the care and treatment of breast cancer: breast radiotherapy after breast-conserving surgery (summary of the 2003 update). CMAJ., 168(4), 437–439.
Wolff, A. C., Hammond, M. E., Schwartz, J. N., Hagerty, K. L., Allred, D. C., Cote, R. J., et al. (2007). American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. Archives of Pathology & Laboratory Medicine, 131(1), 18–43.
Acknowledgements
We thank the study staff, Brittany Speller, Leanne Lindsay, Lucy Leon and Anjali Pandya. We also thank Jessie Cunningham for assisting in the literature search. We acknowledge Cancer Care Ontario for use of its data.
Funding
This work was supported by the Canadian Institutes of Health Research (grant number 130400). This agency had no involvement in the study design, data collection, analysis, interpretation, manuscript preparation or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
We can confirm that we have observed appropriate ethical guidelines and legislation in conducting the study. The study was approved by the University of Toronto Research Ethics Board (Protocol #29342), and informed consent was not required as there was no direct contact with women and the study falls within the ethical domain of non-consensual research. In addition, Research Ethics Board approval was obtained for each regional cancer centre for medical chart abstraction.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Blackmore, K.M., Weerasinghe, A., Holloway, C.M.B. et al. Comparison of wait times across the breast cancer treatment pathway among screened women undergoing organized breast assessment versus usual care. Can J Public Health 110, 595–605 (2019). https://doi.org/10.17269/s41997-019-00210-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/s41997-019-00210-7