Summary
Abstract
Cefuroxime axetil, a prodrug of the cephalosporin cefuroxime, has proven in vitro antibacterial activity against several Gram-positive and Gram-negative organisms, including those most frequently associated with various common community-acquired infections.
In numerous randomised, controlled trials, 5 to 10 days’ treatment with oral cefuroxime axetil (250 or 500mg twice daily) was an effective treatment in patients with upper (URTI) and lower respiratory tract infections (LRTI) as assessed by clinical and bacteriological criteria. The drug was as effective as several other cephalosporins, quinolones, macrolides and amoxicillin/clavulanic acid. Shorter courses (5 to 10 days’) of cefuroxime axetil were at least as effective as a 10 day course.
Furthermore, sequential therapy with intravenous cefuroxime (750mg 2 or 3 times daily for 2 to 5 days) followed by oral cefuroxime axetil (500mg twice daily for 3 to 8 days) proved an effective treatment in adult patients with community-acquired pneumonia (CAP). This approach provided similar efficacy to intravenous ampicillin/sulbactam followed by oral amoxicillin/clavulanic acid, a full parenteral course of cefuroxime, or intravenous then oral azithromycin or clarithromycin.
Additionally, cefuroxime axetil was an effective treatment in patients with genitourinary, skin and soft-tissue infections, and erythema migrans associated with early stage Lyme disease.
The drug is well tolerated by adult and paediatric patients, with adverse effects that are consistent with those of other cephalosporins. The majority of adverse events (primarily gastrointestinal disturbances) were mild to moderate in intensity and reversible upon discontinuation of treatment, with very few serious adverse events reported.
Conclusions: Cefuroxime axetil is a broad spectrum antibacterial agent with a pharmacokinetic profile that permits convenient twice-daily administration. The drug is an effective and well tolerated treatment in patients with various infections, including otitis media, pharyngitis, sinusitis, CAP and acute exacerbations of chronic bronchitis. Cefuroxime axetil proved effective as a component of intravenous/oral sequential therapy in the treatment of CAP, although there are currently no dosage recommendations available for this regimen in some countries. Cefuroxime axetil may be considered as an empirical therapy for a range of community-acquired infections, including those in which β-lactamase-producing strains of common respiratory pathogens are identified as the causative organisms. In an era of rapidly emerging bacterial resistance, empirical treatment with agents such as cefuroxime axetil may ensure the appropriate use of newer antibacterial agents, potentially preventing the emergence of bacterial resistance to these newer drugs.
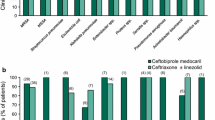
Antibacterial Activity
Cefuroxime axetil, a cephalosporin antibacterial agent, prevents bacterial growth primarily by inhibiting penicillin-binding protein 3, resulting in bacterial elongation and leakage and, eventually, cell death. The drug shows good activity against a broad range of Gram-positive and Gram-negative bacteria in vitro, including those most commonly associated with respiratory tract infections [e.g. Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, S. pyogenes and methicillin-sensitive Staphylococcus aureus (MSSA)].
Against Gram-positive bacteria, cefuroxime is active against penicillin-susceptible strains of S. pneumoniae [mean minimal inhibitory concentrations required for 90% of strains (MIC90) range ≤0.06 to ≤0.25 mg/L], shows some activity against isolates of S. pneumoniae that are intermediately susceptible to penicillin (mean MIC90 range 2 to 4 mg/L), but has no activity against penicillin-resistant S. pneumoniae (mean MIC90 2 to ≥8 mg/L). In a recent study, against S. pyogenes isolates, cefuroxime (mean MIC90≤0.25 mg/L) antibacterial activity was comparable with that of other cephalosporins. Mean MIC90 values for cefuroxime axetil against MSSA ranged from 2 to 4 mg/L worldwide. Like most other β-lactam antibiotics, cefuroxime has no activity against methicillin-resistant strains of Staphylococcus species (including MRSA).
Cefuroxime also shows good activity against several Gram-negative bacteria, including β-lactamase-positive and -negative strains of H. influenzae (mean MIC90 range 1 to 2 and 2 to 4 mg/L, respectively), M. catarrhalis (mean MIC90 2 and 0.5 mg/L) and Neisseria gonorrhoeae (mean MIC90 0.125 and 0.06 mg/L). In recent studies, ≥95% of H. influenzae and ≥99% of M. catarrhalis isolates were susceptible to cefuroxime. The drug also exhibited activity against the common urinary tract pathogen Escherichia coli, with mean MIC90 values of 4 and 8 mg/L in 2 recent studies. However, in a recent worldwide study, the susceptibility of E. coli (4509 isolates) to cefuroxime in different regions of the world was generally lower than this and showed greater variation, with mean MIC90 values ranging from 8 to 32 mg/L (median MIC90 16 mg/L). Cefuroxime showed limited activity against Klebsiella pneumoniae strains (mean MIC90 range 16 to >16 mg/L). In addition, cefuroxime shows limited or no activity against most other Enterobacteriaceae, including Citrobacter spp. and Serratia marcescens, or against Pseudomonas aeruginosa and Acinetobacter spp.
The spectrum of pathogens susceptible to cefuroxime axetil has not changed substantially over the last decade, with the exception of some nosocomial isolates of Enterobacteriaceae (notably K. pneumoniae and E. coli) that have developed resistance to cefuroxime and other cephalosporins by producing TEM and SHV extended spectrum β-lactamases. Cefuroxime has shown stability to the most common plasmid-mediated β-lactamases TEM-1, TEM-2, OXA-1 and OXA-2 produced by E. coli, and to SHV-1-producing K. pneumoniae.
Pharmacodynamic/pharmacokinetic analyses suggest that the time cefuroxime concentrations are above the MIC90 values for relevant pathogens (e.g. S. pneumoniae isolates that are susceptible or intermediately-susceptible to penicillin, and β-lactamase-positive and -negative H. influenzae isolates) exceeds 50% of the dosage interval in most situations.
Pharmacokinetic Properties
The lipophilic acetoxyethyl-ester prodrug cefuroxime axetil is well absorbed from the gastrointestinal tract and is rapidly hydrolysed by nonspecific esterases in the intestinal mucosa and blood to cefuroxime and the ester group.
The mean absolute oral bioavailability of cefuroxime axetil was 67.9% (n = 12). The extent of absorption was increased from 36 to 52% when the drug was coadministered with food.
The pharmacokinetic profile of cefuroxime after oral cefuroxime axetil (administered immediately after a meal) is linear over the 125 to 1000mg dose range. The peak plasma concentration (Cmax) ranged from 2.1 to 13.6 mg/L over this dose range while the corresponding values for elimination half-life (t½), time to Cmax (tmax) and area under the plasma concentration time-curve (AUC) were 2.2 to 3 hours, 1.2 to 1.3 hours and 6.7 to 50 mg/L · h, respectively, when the drug was administered as an oral tablet.
After ingestion of cefuroxime axetil 250mg in either tablet or suspension form following a meal, there was little difference in the t½ or tmax of cefuroxime; however, both the AUC (10.22 vs 14.02 mg/L · h) and the Cmax (2.48 vs 4.04 mg/L) were significantly lower after ingestion of the suspension than after the tablet (p = 0.001 for both comparisons). Thus the 2 formulations are not bioequivalent.
The protein binding of cefuroxime after oral cefuroxime axetil has not been studied, but the plasma protein binding of cefuroxime after intravenous injection of cefuroxime has been variously reported as 33% and 50%. The volume of distribution of cefuroxime is ≈0.25 to 0.3 L/kg.
The highest levels of penetration of cefuroxime after oral cefuroxime axetil (single dose of 375 or 500mg) are seen in sinus tissue (38.1 to 106% with tissue levels of 0.4 to 2.4 mg/kg). Penetration into bronchial mucosa and tonsil tissue was also good (35 to 90%). In addition, after a single dose of cefuroxime axetil 250mg or 15 mg/kg to children with acute otitis media, cefuroxime was shown to penetrate into middle ear effusion. Mean tissue concentrations in these patients were 1.2 and 1.3 mg/kg and in 1 of these studies 29.8% tissue penetration was reported. Penetration into aqueous humor was 13.8% and the mean concentration of cefuroxime obtained (0.5 mg/L) was below the MIC90 for most, but not all, of the organisms frequently involved in intraocular infections.
Cefuroxime is released from cefuroxime axetil by de-esterification, but is not metabolised further and approximately 50% of the drug is eliminated unchanged in the urine within 12 hours. In healthy adult volunteers who received a single oral dose of cefuroxime axetil 250mg urinary recovery ranged from 42.8 to 57%.
Because cefuroxime axetil is eliminated renally the ty, increases with decreasing renal function. The pharmacokinetics of cefuroxime in elderly volunteers who received the suspension formulation of cefuroxime axetil were similar to those in younger volunteers who received the same preparation.
Therapeutic Efficacy
Upper respiratory tract infections: In adult and adolescent patients with acute sinusitis, randomised controlled trials have shown that cefuroxime axetil (250mg twice daily for 8 to 10 days) provided comparable clinical and bacteriological efficacy to that of 7 to 10 days’ treatment with a quinolone agent, including moxifloxacin, gemifloxacin, sparfloxacin and ciprofloxacin. In clinically evaluable patients, satisfactory clinical responses occurred in 83 to 90% of cefuroxime axetil recipients versus 83 to 97% of patients receiving a quinolone comparator agent. Overall presumed or documented bacteriological eradication paralleled satisfactory clinical response rates, with eradication occurring in 89 to 95% of microbiologically evaluable cefuroxime axetil recipients versus 94 to 97% of those receiving a quinolone. Cefuroxime axetil also provided comparable clinical efficacy to that of clarithromycin or amoxicillin/clavulanic acid as assessed by clinical and bacteriological criteria. Furthermore, clinical (85 vs 87% of patients) and bacteriological response rates (89 vs 91%) indicated that 5 days’ treatment with cefuroxime axetil (250mg twice daily) was as effective as 10 days’ treatment in a double-blind trial.
In children and adults with group A β-haemolytic streptococcal (GABHS) tonsillopharyngitis, clinical (95 to 96% vs 94 to 98% of patients) and bacteriological (88 vs 92% of evaluable patients) response rates were similar with either 5 or 10 days’ treatment with cefuroxime axetil (250 or 500 mg/day, or 20 mg/kg/day) in 2 comparative randomised trials. Additionally, a 5-day course of cefuroxime axetil (500 mg/day or 20 mg/kg/day) was superior to 10 days’ treatment with phenoxymethylpenicillin (50 000 IU/kg/day) in a large phase IV, non-blind, multicentre study in children and adolescents (as assessed using a 2-sided analysis). At 7 to 8 weeks’ follow-up, asymptomatic carriage of GABHS occurred at an equivalent rate in both treatment groups (11.1% of cefuroxime axetil recipients vs 13.8%). At 12 months’ follow-up, no cefuroxime axetil recipients had experienced serious sequelae (e.g. glomerular nephritis or rheumatic fever) and 1 incident of glomerular nephritis had occurred in a patient who had received phenoxymethylpenicillin.
Cefuroxime axetil was also as effective as cefpodoxime proxetil, cefaclor or clarithromycin in treating children (aged ≤12 years) with acute otitis media (≥93% satisfactory clinical response in each treatment group). Notably, short-course (5 days) cefuroxime axetil treatment was as effective as 10 days’ treatment with the drug or 8 to 10 days’ of amoxicillin/clavulanic acid in terms of either clinical or bacteriological criteria.
Lower respiratory tract infections: Cefuroxime axetil was efficacious in patients with acute bronchitis or acute exacerbations of chronic bronchitis (AECB). The drug was as effective as cefixime, cefpodoxime proxetil, cefprozil, cefdinir, ciprofloxacin, levofloxacin, telithromycin, clarithromycin, roxithromycin and amoxicillin/clavulanic acid. In clinically evaluable patients, clinical response rates (cure or improvement) at the end of therapy in cefuroxime axetil (250 or 500 mg twice daily) recipients ranged from 66 to 94% and were generally similar to those achieved in recipients of comparator drugs (range 74 to 95%). Overall, at the end of treatment, bacteriological eradication (presumed or documented) rates with cefuroxime axetil (60 to 93% of patients) were generally comparable to those achieved with comparator antibacterial drugs (69 to 96%) in microbiologically evaluable patients. In a randomised, double-blind trial, significantly fewer cefuroxime axetil recipients achieved a successful clinical response than gatifloxacin-treated (400mg once daily) patients (77 vs 89% of patients; p < 0.035).
In adult patients with community-acquired pneumonia (CAP), oral cefuroxime axetil (with or without erythromycin) provided similar clinical and bacteriological efficacy to that of oral trovafloxacin.
Sequential therapy with intravenous cefuroxime followed by oral cefuroxime axetil (with or without erythromycin) was as clinically effective as intravenous ampicillin/sulbactam followed by oral amoxicillin/clavulanic acid, a full parenteral course of cefuroxime, intravenous then oral azithromycin or intravenous then oral clarithromycin in adult patients with CAP. 85 to 94% of cefuroxime axetil recipients achieved a satisfactory clinical response versus 90 to 94% of patients treated with comparator agents in per-protocol analyses. In a large non-blind study, clinical (90 vs 96% of patients; 95% CI -10.7, -1.3) and bacteriological (85 vs 98%; 95% CI -21.6, -4.8) success rates were significantly (no p-values reported) lower in evaluable patients receiving combinations of intravenous ceftriaxone (1 to 2g once or twice daily) and/or oral cefuroxime axetil (500mg twice daily) than those in recipients of intravenous and/or oral levofloxacin (500mg once daily).
In paediatric patients with CAP, cefuroxime axetil was as effective as cefpodoxime proxetil or ampicillin/sulbactam. Furthermore, cefuroxime axetil proved clinically effective as a second-line therapy in children who had failed previous antibacterial therapy. Notably, significantly more cefuroxime axetil than ceftibuten recipients experienced a satisfactory clinical response in a randomised multicentre trial in 140 children with CAP (93 vs 80% of patients; p = 0.04), with similar bacteriological eradication rates in both treatment groups (32 vs 36% of patients).
Genitourinary tract infections: Cefuroxime axetil (250mg twice daily), administered for 10 to 12 days, provided similar clinical (92 vs 95% of patients) and bacteriological (no numerical data reported) response rates to those of ofloxacin (200mg twice daily) in adult outpatients with uncomplicated pyelonephritis.
In the treatment of 832 adult patients with uncomplicated gonorrhoea, a single oral dose of cefuroxime axetil 1g or ciprofloxacin 500mg produced similar rates of bacteriological eradication from the cervix of women and urethra of men infected with penicillinase-producing strains of N. gonorrhoeae (≥96% of patients in all treatment groups). In female patients, overall bacteriological eradication rates (i.e. for all N. gonorrhoeae isolates) from the cervix were also similar (≥97% in all treatment groups). However, in male patients, overall eradication rates from the urethra were significantly lower with cefuroxime axetil than with ciprofloxacin (93 vs 100% of patients; p < 0.001).
Other infections: Cefuroxime axetil (250mg twice daily for 10 to 12 days) also appears to be an effective treatment in patients with uncomplicated skin and soft tissue infections, providing similar clinical and bacteriological efficacy to that of cefpodoxime proxetil and cefditoren pivoxil. Additionally, cefuroxime axetil 30 mg/kg/day for 14 days was as effective as 14 days’ treatment with phenoxymethylpenicillin 100 000 IU/kg/day in children with erythema migrans associated with early stage Lyme disease.
Pharmacoeconomic Considerations
Pharmacoeconomic analyses of cefuroxime axetil have generally considered costs associated with treatment only from an institutional perspective. Indirect and societal costs have not been assessed to date.
Resource utilisation costs associated with cefuroxime axetil were compared with those associated with comparator antibacterial agents in 2 studies using data collected from trials conducted in the US and Canada in patients with CAP. In 1 study, a sensitivity analysis excluding patients receiving treatment for <48 hours indicated that per patient total healthcare costs were markedly higher with cefuroxime axetil (500mg twice daily) treatment than with levofloxacin (500mg once daily) [US$883 vs US$660 in 1997 dollars; p = 0.008], although differences in base-case analysis were not significantly different. In the other study, cefuroxime axetil costs per treatment were considered to be comparable to those of erythromycin, clarithromycin and amoxicillin/clavulanic acid.
Intravenous cefuroxime/oral cefuroxime axetil sequential therapy was less costly than a full parenteral course of cefuroxime in a retrospective single-centre, cost analysis calculating drug-related costs in 128 hospitalised patients in Canada (US$15.66 vs $26.21 per day of treatment in 1992 dollars; p > 0.001); this cost difference reflected the reduced costs of oral compared with parenteral therapy.
In a US cost-minimisation analysis in hospitalised patients with CAP, the mean length of stay in hospital was significantly (p < 0.05) reduced in those receiving 2 days’ compared with 5 days’ intravenous cefuroxime prior to switching to oral cefuroxime axetil or in those receiving a full parenteral course of cefuroxime (mean length of stay of 6, 8 and 11 days, respectively). A reduction in the standard 13-day hospital stay to 6 days would potentially result in a 53.9% reduction in the cost of treatment of CAP in US Veterans Affairs facilities.
Tolerability
Oral cefuroxime axetil 250mg or 500mg twice daily for 5 to 10 days was generally well tolerated in children and adults with various bacterial infections. The majority of adverse events were mild to moderate in intensity and reversible upon discontinuation of treatment, with very few serious adverse events reported. Less than 1 to 6% of patients withdrew because of adverse events attributable to cefuroxime axetil treatment.
Most adverse events that occurred during treatment with cefuroxime axetil were of gastrointestinal nature (diarrhoea, nausea, vomiting), although headache, dizziness and skin reactions were also occasionally reported. In recent clinical trials, the most common drug-related adverse events were diarrhoea (2 to 10.2% of patients), nausea (0 to 5%), vomiting (1 to 5%), abdominal pain (2 to 2.8%), dizziness (0.8 to 3%), headache (1 to 3.7%), vaginitis (1 to 2%), and skin rash (3%). The nature and incidence of adverse events was similar with either 5 or 10 days’ treatment with cefuroxime axetil.
Comparative studies indicated that the tolerability profile of cefuroxime axetil appeared to be generally similar to that of a broad range of comparator antibacterial agents, including cephalosporins (cefpodoxime proxetil and cefprozil), quinolones (sparfloxacin, ciprofloxacin, trovafloxacin, levofloxacin, gatifloxacin and moxifloxacin), clarithromycin, telithromycin and phenoxymethylpenicillin. Notably, the tolerability of cefuroxime axetil was superior to that of amoxicillin/clavulanic acid in investigations that included patients with upper and lower respiratory tract infections. Both the overall incidence of gastrointestinal adverse events and the incidence of nausea and vomiting were markedly lower in the cefuroxime axetil than amoxicillin/clavulanic acid groups.
Stevens-Johnson syndrome and toxic dermal necrolysis, Clostridium difficile- related pseudomembranous colitis and hypersensitivity reactions (urticaria, serum sickness and anaphylaxis) have occasionally been reported during cefuroxime axetil treatment.
Dosage and Administration
For adults and children aged ≥13 years with mild to moderate upper and lower respiratory tract infections caused by susceptible bacteria, the usual effective dose of cefuroxime axetil is 250mg twice daily for 7 to 10 days. To optimise absorption, cefuroxime axetil should be administered with food. The treatment of severe lower respiratory tract infections, including CAP, requires a higher dosage of cefuroxime axetil (usually 500mg twice daily). Currently, in the US prescribing information there are no dosage recommendations available for the use of intravenous cefuroxime/oral cefuroxime axetil sequential therapy. In the UK, in patients with AECB the recommended dosages for sequential therapy are intravenous or intramuscular cefuroxime 750mg twice daily for 2 to 3 days followed by oral cefuroxime axetil 500mg twice daily for 7 days; in patients with CAP, the recommended dosage of parenteral cefuroxime is 1.5g twice daily for 2 to 3 days, followed by cefuroxime axetil 500mg for 7 days.
A single 1g dose of cefuroxime axetil is recommended for the treatment of gonorrhoea. The recommended dosage of cefuroxime for adults and adolescents with early stage Lyme disease is 500mg twice daily for 20 days. In the UK, for children aged ≥3 months with upper respiratory tract infections r impetigo, the recommended dosage of cefuroxime axetil tablet and suspension formulations is 125mg and 10 mg/kg twice daily, respectively; patients aged ≥2years with acute otitis media may require treatment with a higher dosage (usually 250mg and 15 mg/kg twice daily, respectively). In the US, the recommended dosage in children aged >3 months with pharyngitis/tonsillitis is 125mg and 10 mg/kg twice daily with tablet and suspension formulations, respectively; in those with acute otitis media, acute maxillary sinusitis or impetigo, the respective recommended dosage of the drug is 250mg and 15 mg/kg twice daily. As cefuroxime axetil has not been studied in infants aged ≤3 months, there are currently no recommendations for the treatment of infections in infants of this age group.
No dosage modifications are required in patients with renal impairment [creatinine clearance ≥1.2 L/h (20 ml/min)] or on renal dialysis or in the elderly at dosages up to 1g per day.



















Similar content being viewed by others
References
Perry CM, Brogden RN. Cefuroxime axetil: a review of its antibacterial activity, pharmacokinetic properties and therapeutic efficacy. Drugs 1996 Jul; 52: 125–58
Fluit AC, Jones ME, Schmitz F-J, et al. Antimicrobial susceptibility and frequency of occurrence of clinical blood isolates in Europe from the SENTRY Antimicrobial Surveillance Program, 1997 and 1998. Clin Infect Dis 2000 Mar; 30: 454–60
Schmitz FJ, Verhoef J, Fluit AC, et al. Comparative activity of 27 antimicrobial compounds against 698 Streptococcus pneumoniae isolates originating from 20 European university hospitals. Eur J Clin Microbiol Infect Dis 1999; 18: 450–3
Jones RN, Jenkins SG, Hoban DJ, et al. In vitro activity of selected cephalosporins and erythromycin against staphylococci and pneumococci isolated at 38 North American medical centers participating in the SENTRY Antimicrobial Surveillance Program, 1997–1998. Diagn Microbiol Infect Dis 2000 Jun; 37: 93–8
Jones RN, Croco MAT, Kugler KC, et al. Respiratory tract pathogens isolated from patients hospitalized with suspected pneumonia: frequency of occurrence and antimicrobial susceptibility from the SENTRY Antimicrobial Surveillance Program (United States and Canada), 1997). Diagn Microbiol Infect Dis 2000; 37: 115–25
Jones RN, Jenkins SG, Hoban DJ, et al. In vitro efficacy of six cephalosporins tested against Enterobacteriaceae isolated at 38 North American medical centres participating in the SENTRY Antimicrobial Surveillance Program, 1997–1998. Int J Antimicrob Agents 2000; 15: 111–8
Sader HS, Gales AC, Granacher TD, et al. Prevalance of antimicrobial resistance among respiratory tract isolates in Latin America: results from SENTRY Antimicrobial Surveillance Program (1997–1998). Brazilian Journal Infectious Diseases 2000; 4(5): 245–54
Doern GV, Jones RN, Pfaller MA, et al. Haemophilus influenzcie and Moraxella catarrhalis from patients with community acquired respiratory tract infections: antimicrobial susceptibility patterns from the SENTRY antimicrobial surveillance program (United States and Canada, 1997). Antimicrob Agents Chemother 1999; 43(2): 385–9
Felmingham D, Grüneberg RN, Alexander Project Group. The Alexander Project 1996–1997: latest susceptibility data from this international study of bacterial pathogens from community-acquired lower respiratory tract infections. J Antimicrob Chemother 2000 Feb; 45: 191–203
Curtis NAC, Orr D, Ross GW, et al. Competition of β-lactam antibiotics for the penicillin-binding proteins of Pseudomonas aeruginosa, Enterobacter cloacae, Klebsiella aerogenes, Proteus rettgeri: and Escherichia coli: comparison with antibacterial activity and effects upon bacterial morphology. Antimicrob Agents Chemother 1979; 16(3): 325–8
Dellamonica P. Cefuroxime axetil. Int J Antimicrob Agents 1994; 4: 23–36
National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial tests for bacteria that grow aerobicallly; approved standard: 5th ed. Document M7-A5.2000 Jan; 20 (2)
Jones ME, Staples AM, Critchley I, et al. Benchmarking the in vitro activity of moxifloxacin against recent isolates of Streptococcus pneumoniae, Moraxella catarrhalis, and Haemophilus influenzae: a European multi-centre study. Diagn Microbiol Infect Dis 2000 Jul; 37: 203–11
Mason Jr EO, Lamberth LB, Kershaw NL, et al. Streptococcus pneumoniae in the USA: in vitro susceptibility and pharmacodynamic analysis. J Antimicrob Chemother 2000 May; 45: 623–31
Zhanel GG, Karlowsky JA, Palatnick LP, et al. In vitro activity of MK-0826 against Canadian respiratory isolates of Streptococcus pneumoniae and Haemophilus influenzae [abstract]. 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17, Toronto (ON), 164
Baquero F, Garcia-Rodriguez JA, De Lomas JG, et al. Antimicrobial resistance of 1,113 Streptococcus pneumoniae isolates from patients with respiratory tract infections in Spain: results of a 1-year (1996–1997) multicenter surveillance study. Antimicrob Agents Chemother 1999 Feb; 43: 357–9
Baquero F, Garcia-Rodriguez JA, De Lomas JG, et al. Antimicrobial resistance of 914 beta-hemolytic streptococci isolated from pharyngeal swabs in Spain: results of a 1-year (1996–1997) multicenter surveillance study. Antimicrob Agents Chemother 1999 Jan; 43: 178–80
Hoban DJ, Karlowsky JA, Zhanel GG. Gemifloxacin demonstrates potent activity against Canadian lower respiratory tract infection pathogens isolated in 1999/2000 [abstract]. 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17, Toronto (ON), 189
Hoban DJ, Low DE, Karlowsky JA, et al. Comparative activity of the new respiratory fluoroquinolones against Canadian respiratory tract pathogens [abstract]. Can J Infect Dis 1999 Sep–Oct; 10 Suppl. D: 33
Zhanel GG, Karlowsky JA, Low DE, et al. Antibiotic resistance in respiratory tract isolates of Haemophilus influenzae and Moraxella catarrhalis collected from across Canada in 1997–1998. J Antimicrob Chemother 2000 May; 45: 655–62
Richter SS, Brueggemann AB, Huynh HK, et al. A 1997–1998 national surveillance study: Moraxella catarrhalis and Haemophilus influenzae antimicrobial resistance in 34 US institutions. Int J Antimicrob Agents 1999; 13(2): 99–107
National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing. Document M100-S7. 1997 Dec; 17 (22)
Jones RN. Can antimicrobial activity be sustained? An appraisal of orally administered drugs used for respiratory tract infections. Diagn Microbiol Infect Dis 1997 Jan–Feb; 27: 21–8
Hoban DJ, Bouchillon SK, Stevens TM, et al. Global resistance patterns of quinolones, macrolides and beta-lactams from a multi-center, multi-country study of >9,000 isolates: the Gemifloxacin Surveillance Study [abstract]. 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 17 Sep: Toronto, Ontario, 187
Wiedemann B. Unchanged activity of cefuroxime axetil towards most common pathogens in Germany [abstract/poster no.46.002]. 9th International Congress of Infectious Diseases, 2000 Apr 10–13, Buenos Aires
Cars O. Efficacy of beta-lactam antibiotics: integration of pharmacokinetics and pharmacodynamics. Diagn Microbiol Infect Dis 1997; 27: 29–33
Sahm DF, Jones ME, Hickey ML, et al. Resistance surveillance of Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis isolated in Asia and Europe, 1997–1998. J Antimicrob Chemother 2000 Apr; 45: 457–66
Chambers HF. Penicillin-binding protein-mediated resistance in pneumococci and staphylococci. J Infect Dis 1999 Mar; 179 Suppl. 2: S353–359
Thornsberry C, Sahm DF. Antimicrobial resistance in respiratory tract pathogens: results of an international surveillance study. Chemotherapy 2000; 46 Suppl. 1: 15–23
Schumacher H, Skibsted U, Hansen DS, et al. Cefuroxime resistance in Klebsiella pneumoniae: susceptibility to cefotaxime and ceftazidime despite production of ESBLs. APMIS 1997 Sep; 105: 708–16
Schumacher H, Skibsted U, Skov R, et al. Cefuroxime resistance in Escherichia coli: resistance mechanisms and prevalence. APMIS 1996 Jul–Aug; 104: 531–8
Schumacher H, Scheibel J, Møller JK. Cross-resistance patterns among clinical isolates of Klebsiella pneumoniae with decreased susceptibility to cefuroxime. J Antimicrob Chemother 2000 Aug; 46: 215–21
Craig WA. Choosing an antibiotic on the basis of pharmacodynamics. Ear, Nose Throat J 1998; 77 Suppl.: 7–12
Garraffo R, Drageon HB, Chiche D. Pharmacokinetics and pharmacodynamics of two oral forms of cefuroxime axetil. Fundam Clin Pharmacol 1997; 11: 90–5
Cazzola M, Matera MG, Donner CF. Pharmacokinetics and pharmacodynamics of newer oral cephalosporins: implications for treatment of community-acquired lower respiratory tract infections. Clin Drug Invest 1998; 16: 335–46
Stoeckel K, Hayton WL, Edwards DJ, et al. Clinical pharmacokinetics of oral cephalosporins. Antibiot Chemother 1995; 47: 34–71
Stein GE, Schooley S, Walker RD, et al. Pharmacodynamic activity of five oral cephalosporins against Haemophilus influenzae. Pharmacotherapy 1997; 17(2): 235–41
Dan M, Poch F, Edelman A, et al. Serum bactericidal activity of newer oral cephalosporins in healthy volunteers. J Antimicrob Chemother 1998 Apr; 41: 485–8
Lacy MK, Owens Jr RC, Xu X, et al. Comparison of bactericidal activity after multidose administration of clarithromycin, azithromycin, and ceruroxime axetil against Streptococcus pneumoniae. Int J Antimicrob Agents 1998 Nov; 10: 279–83
Dubois J, St-Pierre C. In vitro study of the post-antibiotic effect and the bactericidal activity of cefditoren and ten other oral antimicrobial agents against upper and lower respiratory tract pathogens. Diagn Microbiol Infect Dis 2000 Jul; 37: 187–93
Davies TA, Kelly LM, Pankuch GA, et al. Antipneumococcal activities of gemifloxacin compared to those of nine other agents. Antimicrob Agents Chemother 2000 Feb; 44: 304–10
Finn A, Straughn A, Meyer M, et al. Effect of dose and food on the bioavailability of cefuroxime axetil. Biopharm Drug Dispos 1987 Nov–Dec; 8: 519–26
GlaxoWellcome US. Ceftin tablets and oral suspension. Available from: URL: http://www.glaxowellcome.com/product.htm [Accessed 2001 Jun 4]
Veyssier P, Darchis JP, Devillers A. Pharmacokinetics of cefuroxime-axetil after oral administration during six days treatment in elderly patients [in French]. Therapie 1988 Jun–Jul 4; 43 Suppl. 4: 355–9
Wood GC, Ling MR, Herring VL, et al. Pharmacokinetics of cefuroxime axetil oral suspension in elderly volunteers [abstract]. Pharmacotherapy 2000 Oct; 20: 1243
Lang C, Moreland TA, Davey PG. Bioavailability of cefuroxime axetil: comparison of standard and abbreviated methods. J Antimicrob Chemother 1990 Apr; 25: 645–50
Baldwin DR, Andrews JM, Wise R, et al. Bronchoalveolar distribution of cefuroxime axetil and in-vitro efficacy of observed concentrations against respiratory pathogens. J Antimicrob Chemother 1992 Sep; 30: 377–85
Drewelow B, Kock K. Penetration of cefuroxime into bronchial secretions in patients with pneumonia during sequential therapy with cefuroxime/cefuroxime axetil. 18th International Congress of Chemotherapy; 1993 Jun–Jul; Stockholm
Walstad R, Vilsvik J, Thurmann Nielsen E, et al. Pharmacokinetics of cefuroxime axetil in patients with LRTI: a profile of cefuroxime axetil. Proceedings of a one-day symposium held at the Royal College of Physicians, London, 1988 Apr; 76–77
Wise R, Baldwin DR, Honeybourne D, et al. Penetration of antibiotics into the bronchial mucosa: a review. Res Clin Forum 1990; 12(4): 1–5
Winter J, Dhillon P. Penetration of cefuroxime into bronchial mucosa following oral administration of cefuroxime axetil [letter]. J Antimicrob Chemother 1991 Apr; 27: 556–8
Jetlund O, Thurmann Nielsen E, Walstad RA. Comparison of the serum and tissue concentrations of cefuroxime from cefuroxime axetil and phenoxymethylpenicillin in patients undergoing tonsillectomy. Int J Clin Pharmacol Res 1991; 11: 1–6
Foord RD. Cefuroxime: human pharmacokinetics. Antimicrob Agents Chemother 1976; 9: 741
Sudderick RM, Lund VJ, Thomson JP, et al. An evaluation of the penetration of cefuroxime axetil into human paranasal sinus tissue. Rhinology 1992 Mar; 30: 11–6
Stoeckel K, Harell M, Dan M. Penetration of cefetamet pivoxil and cefuroxime axetil into the maxillary sinus mucosa at steady state. Antimicrob Agents Chemother 1996 Mar; 40: 780–3
Dinis PB, Monteiro MC, Lobato R, et al. Penetration of cefuroxime into chronically inflamed sinus mucosa. Laryngoscope 1999 Nov; 109: 1841–7
Haddad Jr J, Isaacson G, Respler DS, et al. Concentration of cefuroxime in serum and middle ear effusion after single dose treatment with cefuroxime axetil. Pediatr Infect Dis J 1991 Apr; 10: 294–8
Thoroddsen E, Marr C, Efthymiopoulos C, et al. Concentration of cefuroxime in middle ear effusion of children with acute otitis media. Pediatr Infect Dis J 1997 Oct; 16: 959–62
Ghia M, Lotti R, Traverso C, et al. Penetration of oral cefuroxime axetil into the human aqueous humor. Ophthalmologica 1997; 211: 229–31
Tan JS, Salstrom SM, File TM. Cefadroxil, cefaclor, cefuroxime: interstitial fluid concentrations determined through a skin window. Adv Ther 1994; 11(3): 154–62
Renneberg J, Christensen OM, Thomsen NOB, et al. Cefuroxime concentrations in serum, joint fluid and bone in elderly patients undergoing arthroplasty after administration of cefuroxime axetil. J Antimicrob Chemother 1993 Nov; 32: 751–5
Robson HJ, Craig DQ, Deutsch D. An investigation into the release of cefuroxime axetil from taste-masked stearic acid microspheres. Part 1: the influence of the dissolution medium on the drug release profile and the physical integrity of the microspheres. Int J Pharm 1999 Nov 15; 190: 183–92
Konishi K, Suzuki H, Hayashi M. Pharmacokinetics of cefuroxime axetil in patients with normal and impaired renal function. J Antimicrob Chemother 1993 Mar; 31: 413–20
Pichichero ME, Disney FA, Aronovitz GH, et al. A multicenter, randomized, single-blind evaluation of cefuroxime axetil and phenoxymethyl penicillin in the treatment of streptococcal pharyngitis. Clin Pediatr Phila 1987 Sep; 26: 453–8
Gehanno P, Chiche D. Treatment of group A β-haemolytic streptococcal tonsillitis with cefuroxime axetil for 4 days: a comparative study with penicillin V for 10 days [in French]. Med Mal Infect 1991 Sep; 21 Suppl.: 66–70
Aujard Y, Boucot I, Brahimi N, et al. Comparative efficacy and safety of four-day cefuroxime axetil and ten-day penicillin treatment of group A beta-hemolytic streptococcal pharyngitis in children. Pediatr Infect Dis J 1995 Apr; 14: 295–300
Bégué P, Lacroix J. Cefuroxime axetil and respiratory tract infection: results of a multicenter trial conducted in pediatric offices [in French]. Med Mal Infect 1991 Sep; 21 Suppl.: 75–8
Holm S, Henning C, Grahn E. Is penicillin the appropriate treatment for recurrent tonsillopharyngitis? Results from a comparative randomized blind study of cefuroxime axetil and phenoxymethylpenicillin in children. Scand J Infect Dis 1995; 27(3): 221–8
Gooch III WM, Swenson E, Higbee MD, et al. Cefuroxime axetil and penicillin V compared in the treatment of group A beta-hemolytic streptococcal pharyngitis. Clin Ther 1987; 9: 670–7
Gooch III WM, McLinn SE, Aronovitz GH, et al. Efficacy of cefuroxime axetil suspension compared with that of penicillin V suspension in children with group A streptococcal pharyngitis. Antimicrob Agents Chemother 1993 Feb; 37: 159–63
Pichichero M, Aronovitz GH, Gooch WM, et al. Comparison of cefuroxime axetil, cefaclor, and amoxicillin-clavulanate potassium suspensions in acute otitis media in infants and children. South Med J 1990 Oct; 83: 1174–7
Stahl JP, Archimbaud A. Treatment of acute otitis media in children: comparison of cefuroxime axetil and amoxicillin-clavulanate suspensions [in French]. Med Mal Infect 1995 Feb; 25: 147–53
McLinn SE, Moskal M, Goldfarb J, et al. Comparison of cefuroxime axetil and amoxicillin-clavulanate suspensions in treatment of acute otitis media with effusion in children. Antimicrob Agents Chemother 1994 Feb; 38: 315–8
Gooch IIIWM, Blair E, Puopolo A, et al. Clinical comparison of cefuroxime axetil suspension and amoxicillin/clavulanate suspension in the treatment of pediatric patients with acute otitis media with effusion. Clin Ther 1995; 17(5): 838–51
Syrogiannopoulos GA, Goumas PD, Haliotis FA, et al. Cefuroxime axetil in the treatment of acute otitis media in children. J Chemother 1992 Aug; 4: 221–4
Brodie DP, Griggs JV, Cunningham K. Comparative study of cefuroxime axetil suspension and amoxycillin syrup in the treatment of acute otitis media in general practice. J Int Med Res 1990 May–Jun; 18: 235–9
Dellamonica P, Choutet P, Lejeune JM, et al. Efficacy and safety of cefotiam hexetil in the treatment of acute otitis media. A comparative double blind randomized study versus cefuroxime axetil [in French]. Med Mal Infect 1995 Apr; 25: 599–604
Dellamonica P, Choutet P, Lejeune JM, et al. Efficacy and safety of cefotiam hexetil in the treatment of chronic otitis media. A comparative double blind randomized study versus cefuroxime axetil [in French]. Med Mal Infect 1995 May; 25: 733–9
McLinn SE, Werner K, Cochetto DM. Clinical trial of cefuroxime axetil versus cefaclor for acute otitis media with effusion. Curr Ther Res 1988; 43(1): 1–11
Brodie DP, Knight S, Cunningham K. Comparative study of cefuroxime axetil and amoxycillin in the treatment of acute sinusitis in general practice. J Int Med Res 1989 Nov–Dec; 17: 547–51
Camacho AE, Cobo R, Otte J, et al. Clinical comparison of cefuroxime axetil and amoxicillin/clavulanate in the treatment of patients with acute bacterial maxillary sinusitis. Am J Med 1992 Sep; 93: 271–6
Freche C, Fombeur JP, Pappo M. Evaluation of cefuroxime-axetil in the treatment of acute sinusitis in adults: comparative study with cefaclor [in French]. Therapie 1988 (43) Suppl. 4: 365–8
Gehanno P, Boucot I, Chiche D, et al. Treatment of community acquired acute sinusitis: cefuroxime axetil vs cefixime [in French]. Med Mal Infect 1991 Sep; 21 Suppl.: 61–5
Sydnor Jr A, Gwaltney Jr JM, Cocchetto DM, et al. Comparative evaluation of cefuroxime axetil and cefaclor for treatment of acute bacterial maxillary sinusitis. Arch Otolaryngol Head Neck Surg 1989 Dec; 115: 1430–3
Pessey JJ, Gobert P, le Groupe de Travail ORL, et al. Efficacy and safety of cefpodoxime proxetil versus cefuroxime axetil in the treatment of patients with acute sinusitis [in French]. Med Mal Infect 1994 Jun; 22 Spec. issue: 686–92
Brankston ER, Conter HS, Corriveau R, et al. Cefprozil versus cefuroxime axetil in the treatment of acute sinusitis. Clin Drug Invest 1998; 15(2): 81–90
Burke T, Villanueva C, Mariano Jr H, et al. Comparison of moxifloxacin and cefuroxime axetil in the treatment of acute maxillary sinusitis. Sinusitis Infection Study Group. Clin Ther 1999 Oct; 21: 1664–77
Ferguson BJ, Anon JB, Hendrick KC, et al. Efficacy of once daily gemifloxacin for 7 days compared with cefuroxime twice daily for 10 days in the treatment of acute bacterial sinusitis [abstract]. 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17: Toronto (ON), 475
Gehanno P, Berche P. Sparfloxacin versus cefuroxime axetil in the treatment of acute purulent sinusitis. Sinusitis Study Group. J Antimicrob Chemother 1996 May; 37 Suppl. A: 105–14
Johnson PA, Rodriguez HP, Wazen JJ, et al. Ciprofloxacin versus cefuroxime axetil in the treatment of acute bacterial sinusitis. Sinusitis Infection Study Group. J Otolaryngol 1999 Feb; 28: 3–12
Siegert R, Gehanno P, Nikolaidis P, et al. A comparison of the safety and efficacy of moxifloxacin (BAY 12-8039) and cefuroxime axetil in the treatment of acute bacterial sinusitis in adults. Sinusitis Study Group. Respir Med 2000 Apr; 94: 337–44
Weis M, Hendrick K, Tillotson G, et al. Multicenter comparative trial of ciprofloxacin versus cefuroxime axetil in the treatment of acute rhinosinusitis in a primary care setting. Rhinosinusitis Investigation Group. Clin Ther 1998 Sep–Oct; 20: 921–32
Elies W. Five days of treatment with cefuroxime axetil compared with 10 days of treatment with clarithromycin in acute sinusitis [abstract]. Clinical Microbiology and Infection 1999; 5 Suppl. 3: 277
Stefansson P, Jacovides A, Jablonicky P, et al. Cefuroxime axetil versus clarithromycin in the treatment of acute maxillary sinusitis. Rhinology 1998 Dec; 36: 173–8
Henry DC, Sydnor Jr A, Settipane GA, et al. Comparison of cefuroxime axetil and amoxicillin/clavulanate in the treatment of acute bacterial sinusitis. Clin Ther 1999 Jul; 21: 1158–70
Namyslowski G, Misiolek M. Comparison of the efficacy and tolerability of amoxycillin/clavulanic acid, 875 mg bid, with cefuroxime, 500 mg bid, in the treatment of chronic sinusitis in adults [abstract]. 39th Interscience Conference on Antimicrobial Agents and Chemotherapy; 1999 26 Sep, San Francisco, (CA): 710
Mylan Zagam Discontinued: charges total $4.7 mil. in fiscal third quarter. FDC Rep Pink Sheet 2001; 63(6): 29
Elies W. Oral sequential therapy with cefuroxime axetil. Results in patients with severe bacterial sinusitis [in German]. Chemotherapie J 1996; 5(3): 136–42
Dubreuil C, Gehanno P, Goldstein F, et al. Treatment of acute maxillary sinusitis in adult outpatients: comparison of a five versus ten day-course of cefuroxime axetil. Med Mal Infect 2001; 31: 70–8
Belohradsky BH, Weiss M, Huber K, et al. Randomized comparative trial of cefuroxime axetil once daily for 5 or 10 days in patients with streptococcal pharyngitis [abstract]. Antiinfective Drugs Chemother 1998; 16 Suppl. 1: 86
Mehra S, van-Moerkerke M, Welck J, et al. Short course therapy with cefuroxime axetil for group A streptococcal tonsillopharyngitis in children. Pediatr Infect Dis J 1998 Jun; 17: 452–7
Adam D, Scholz H, Helmerking M. Comparison of short-course (5 day) cefuroxime axetil with a standard 10 day oral penicillin V regimen in the treatment of tonsillopharyngitis. J Antimicrob Chemother 2000 Feb; 45 Topic 1: 23–30
Olivier C. Rheumatic fever: is it still a problem? J Antimicrob Chemother 2000; 45 Topic T1: 13–21
Adam D. Introduction. J Antimicrob Chemother 2000; 45 Topic T1: 1–2
Triqlia JM, Gaudelus J, Riebbels V, et al. Cefuroxime axetil (CAE) compared with cefpodoxime axetil (CPD) for treatment of acute otitis media (AOM) in pediatric patients [abstract/poster no. P298]. Clin Microbio Infec 1999; 5 Suppl. 3: 164
Turik MA, Johns Jr D. Comparison of cefaclor and cefuroxime axetil in the treatment of acute otitis media with effusion in children who failed amoxicillin therapy. J Chemother 1998 Aug; 10: 306–12
Kafetzis DA, Malaka Z-C, Bairamis T, et al. Comparison of the efficacy and tolerability of clarithromycin suspension and cefuroxime axetil suspension in the treatment of acute otitis media in paediatric patients. Clin Drug Invest 1997; 14(3): 192–9
Gooch WM, Blair E, Puopolo A, et al. Effectiveness of five days of therapy with cefuroxime axetil suspension for treatment of otitis media. Pediatr Infect Dis J 1996; 15: 157–64
Pessey JJ, Gehanno P, Thoroddsen E, et al. Short course therapy with cefuroxime axetil for acute otitis media: results of a randomized multicenter comparison with amoxicillin/clavulanate. Pediatr Infect Dis J 1999 Oct; 18: 854–9
Higuera F, Hidalgo H, Feris J, et al. Comparison of oral cefuroxime axetil and oral amoxycillin/clavulanate in the treatment of community-acquired pneumonia. J Antimicrob Chemother 1996; 37: 555–64
Henry D, Ruoff GE, Rhudy J, et al. Effectiveness of shortcourse therapy (5 days) with cefuroxime axetil in the treatment of secondary bacterial infections of acute bronchitis. Antimicrob Agents Chemother 1995; 39(11): 2528–34
Landau Z, Schlaffer F, Pitlik S. Cefuroxime axetil vs. augmentin for the treatment of acute bronchitis and exacerbation of chronic obstructive pulmonary disease. Isr J Med Sci 1992 Nov; 28: 797–9
Schnelle K. Therapy of acute exacerbations of chronic bronchitis: clinical comparison of the antibiotics cefuroxime axetil and amoxicillin/clavulanic acid [in German]. Med Welt 1993 Apr; 44: 293–8
Stahl JP, Pappo M. A multicenter randomized trial of cefuroxime-axetil versus amoxicillin with calvulanic acid in community-acquired ENT and lower respiratory tract infections [in French]. Semin Hôp Paris 1989 Feb 2: 247–51
Yangco BG, Lowe J, Nolen TM, et al. A multicenter trial comparing the efficacy and safety of cefuroxime axetil and cefaclor in pneumonia of adults. Clin Ther 1990 Sep–Oct; 12: 440–6
Nolen TM, Phillips HL, Hutchison J, et al. Comparison of cefuroxime axetil and cefaclor for patients with lower respiratory tract infections presenting to a rural family practice clinic. Curr Ther Res 1988 November; 44(5): 821–9
Schleupner CJ, Anthony WC, Tan J, et al. Blinded comparison of cefuroxime to cefaclor for lower respiratory tract infections. Arch Intern Med 1988 Feb; 148: 343–8
Camus P, Beraud A, Philip-Joet F, et al. Five days’ treatment of acute purulent bronchitis in the elderly with cefpodoxime proxetil [in French]. Med Mal Infect 1994 Jun; 22 Spec. issue: 681–5
Shalit I, Dagan R, Engelhard D, et al. Cefuroxime efficacy in pneumonia: sequential short-course IV/oral suspension therapy. Isr J Med Sci 1994 Sep; 30: 684–9
Ducroix JP, Martin F, Smail A, et al. Cefuroxime IM followed by cefuroxime axetil PO: evaluation of a therapeutic protocole for the therapy of community acquired respiratory infections in adults [in French]. Med Mal Infect 1991 Sep; 21 Suppl.: 82–6
Barlinski J, Kolinski P. Parenteral cefuroxime followed by cefuroxime axetil in thhe treatment of children with community acquired pneumonia. Pediatria Polska 1994; 69(1): 43–7
Brambilla C, Kastanakis S, Knight S, et al. Cefuroxime and cefuroxime axetil versus amoxicillin plus clavulanic acid in the treatment of lower respiratory tract infections. Eur J Clin Microbiol Infect Dis 1992 Feb; 11: 118–24
Stille W, Kranz-Jansen M, Maass A-B, et al. Sequential therapy of community acquired pneumonia: intravenous cefuroxime versus intravenous cefuroxime followed by cefuroxime axetil in the treatment of primary pneumoniae. 18th International Congress of Chemotherapy, 1993; Stockholm
Kohl KF. A multicentre clinical trial to compare antibiotic regime in patients with LRTIs: cefuroxime i.v. followed by cefuroxime axetil vs. cefotiam i.v. 17th International Congress of Chemotherapy; 1991 Jun 23–28, Berlin
Li JT, Zhao MW, Zhang JL, et al. Cefuroxime (CXM) followed by cefuroxime axetil (CAE) vs cefoperazone (CPZ) in the treatment of lower respiratory tract infection (LRTI) [[abstract]]. 18th International Congress of Chemotherapy; 1993; Stockholm, 134
Arthur M, McAdoo M, Guerra J, et al. Clinical comparison of cefuroxime axetil with cefixime in the treatment of acute bronchitis. Am J Ther 1996; 3(9): 622–9
Gaillat J, Baranes C, Amsellem D, et al. Traitement des exacerbations aigues de bronchite chronique: efficacite et tolerance du cefuroxime axetil comparees a celles du cefpodoxime proxetil. Med Mal Infect 2001; 31: 52–60
Puopolo A, Littlejohn TW, Nolen T, et al. A randomized, multicenter, comparative trial of cefprozil and cefuroxime axetil in the treatment of acute bacterial bronchitis and AECB. Infect Med 1997; 14 Suppl.: 51–9
Van Herwaarden CL, Langan CE, Siemon G, et al. International study comparing cefdinir and cefuroxime axetil in the treatment of patients with acute exacerbation of chronic bronchitis. Int J Infect Dis 2000; 4: 26–33
Chodosh S, McCarty J, Farkas S, et al. Randomized, double-blind study of ciprofloxacin and cefuroxime axetil for treatment of acute bacterial exacerbations of chronic bronchitis. The Bronchitis Study Group [see comments]. Clin Infect Dis 1998 Oct; 27: 722–9
DeAbate CA, Russell M, McElvaine P, et al. Safety and efficacy of oral levofloxacin versus cefuroxime axetil in acute bacterial exacerbation of chronic bronchitis. Respir Care 1997; 42(2): 206–13
De Abate CA, McIvor RA, McElvaine P, et al. Smokers treated with gatifloxacin had a high clinical cure rate: gatifloxacin vs cefuroxime axetil in patients with acute exacerbations of chronic bronchitis. J Respir Dis 1999; 20 (11) Suppl.: S23-9
Shah PM, Maesen FP, Dolmann A, et al. Levofloxacin versus cefuroxime axetil in the treatment of acute exacerbation of chronic bronchitis: results of a randomized, double-blind study. J Antimicrob Chemother 1999 Apr; 43: 529–39
DeAbate CA, Heyder A, Leroy B, et al. Oral telithromycin (HMR 3647; 800mg od) for 5 days is well tolerated and as effective as cefuroxime axetil (500mg bid) for 10 days in adults with acute exacerbations of chronic bronchitis [abstract]. 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Toronto (ON), 471
Langan C, Clecner B, Cazzola CM, et al. Short-course cefuroxime axetil therapy in the treatment of acute exacerbations of chronic bronchitis. Int J Clin Pract 1998 Jul–Aug; 52: 289–97
Vogel F, Huber K. Effectiveness of short-course therapy (5 days) with cefuroxime axetil vs. roxithromycin (7 days) in treatment of acute exacerbation of chronic bronchitis [abstract]. Antiinfect Drugs Chemothey 1998; 16 Suppl. 1: 85
Henry DC, Ruoff GE, Noonan M, et al. Comparison of the efficacy and tolerability of short-course cefuroxime axetil and amoxicillin/clavulanic acid in the treatment of secondary bacterial infections of acute bronchitis. Clin Drug Invest 1999; 18(5): 335–44
Henry D, Ruoff GE, Rhudy J, et al. Clinical comparison of 5-or 10-days treatment with cefuroxime axetil and 10-days treatment with amoxicillin/clavulanate in patients with acute bronchitis [abstract]. 7th International Congress for Infectious Diseases; 1996 Jun 10: Hong Kong, 297
Anthonisen NR, Manfreda J, Warren CP, et al. Antibiotic therapy in exacerbations of chronic obstructive disease. Ann Intern Med 1987; 106: 196–204
Peterson J, Trovofloxacin Study Group. Oral trovafloxacin vs oral cefuroxime ±erythromycin in community-acquired pneumonia. Drugs 1999; 58 Suppl. 2: 301–3
File Jr TM, Segreti J, Dunbar L, et al. A multicenter, randomized study comparing the efficacy and safety of intravenous and/or oral levofloxacin versus ceftriaxone and/or cefuroxime axetil in treatment of adults with community-acquired pneumonia. Antimicrob Agents Chemother 1997 Sep; 41: 1965–72
Hatipoglu ON, Tasan Y, Yuksekol I, et al. Sequential IV cefuroxime/oral cefuroxime axetil versus sequential IV ampicillin-salbactam/oral amoxicillin-clavulanate therapy in moderate pneumonia [abstract no. P1727]. 1999 Annual Congress European Respiratory Society; 1999 Oct 9–13, Madrid
Siegel RE, Halpern NA, Almenoff PL, et al. A prospective randomized study of inpatient IV antibiotics for community-acquired pneumonia: the optimal duration of therapy [see comments]. Chest 1996 Oct; 110: 965–71
Siegel RE, Alicea M, Lee A, et al. Comparison of 7 versus 10 days of antibiotic therapy for hospitalized patients with uncomplicated community-acquired pneumonia: a prospective, randomized, double-blind study. Am J Ther 1999; 6(4): 217–22
Stille W, Sass R, Klinge R, et al. Ceftriaxone/cefetametpivoxil versus cefuroxime/cefuroxime axetil. Pharmacoeconomic comparison of sequential intravenous/oral therapy in patients with community acquired pneumonia [in German]. Chemotherapie J 2000; 9(2): 87–92
Vand Den Brande P, Vondra V, Vogel F, et al. Sequential therapy with cefuroxime followed by cefuroxime axetil in community-acquired pneumonia. Chest 1997 Aug; 112: 406–15
Vergis EN, Indorf A, File Jr TM, et al. Azithromycin vs cefuroxime plus erythromycin for empirical treatment of community-acquired pneumonia in hospitalized patients: a prospective, randomized, multicenter trial. Arch Intern Med 2000 May 8; 160: 1294–300
Vetter N, Stamler D, O’Neill S, et al. Clarithromycin vs combined intravenous cefuroxime and erythromycin in the treatment of hospitalised community-acquired pneumonia patients: intravenous followed by oral therapy. Clin Drug Invest 1997 Dec; 14: 439–49
Boulesteix J, Olivier C, Mselati JC, et al. Lower respiratory tract infections in children: compared efficacy of cefuroxime axetil with cefpodoxime proxetil [in French]. Med Mal Infect 2000; 30(9): 581–7
Danisovicova-Nogeova A, Galova K, Sufliarska S, et al. Cefuroxime-axetil versus ampicillin-sulbactam in therapy of community acquired pneumonia: A randomized multicenter study in 149 children. Antiinfect Drugs Chemother 1998; 16(3–4): 219–20
Nogeova A, Galova K, Krizan L, et al. Ceftibuten vs cefuroxime-axetil in initial therapy for community-acquired bronchopneumonia: randomized multicentric study in 140 children. Infect Dis Clin Pract 1997; 6(2): 133–4
Naber KG, Bischoff W, Huber K, et al. Open, randomised, multicentre study with cefuroxime axetil versus ofloxacin in woman with uncomplicated pyelonephritis [abstract]. Antiinfective Drugs Chemother 1998; 16 Suppl. 1: 35
Thorpe Jr EM, Schwebke JR, Hook III EW, et al. Comparison of single-dose cefuroxime axetil with ciprofloxacin in treatment of uncomplicated gonorrhea caused by penicillinase-producing and non-penicillinase-producing Neisseria gonorrhoeae strains. Antimicrob Agents Chemother 1996 Dec; 40: 2775–80
Millikan L, Hahn H, Horn R, et al. Cefditoren is safe and effective treatment for uncomplicated skin and skin structure infections [abstract]. 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17: Toronto (ON), 482
Nakayama I, Yamaji E, Hirata H, et al. Comparative effectiveness and safety of cefpodoxime proxetil versus cefuroxime axetil for the treatment of skin and soft-tissue infections [abstract]. 8th International Congress for Infectious Diseases; 1998 May 15: San Francisco (CA), 710
Iravani A, Richard GA. Single-dose cefuroxime axetil versus multiple-dose cefaclor in the treatment of acute urinary tract infections. Antimicrob Agents Chemother 1989 Aug; 33: 1212–6
Naber KG, Koch EMW. Cefuroxime axetil versus ofloxacin for short-term therapy of acute uncomplicated lower urinary tract infections in women. Infection 1993 Jan–Feb; 21: 34–9
Leigh DA, Joy GE, Tait S, et al. Treatment of acute uncomplicated urinary tract infections with single daily doses of cefuroxime axetil. J Antimicrob Chemother 1989 Feb; 23: 267–73
Williams KJ, Hebblethwaite EM, Brown GW, et al. Cefuroxime axetil in the treatment of uncomplicated UTI: a comparison with cefaclor and augmentin. Drugs Exp Clin Res 1987; 13: 95–9
Cox CE, Sherrill JM, Cocchetto DM. Evaluation of cefuroxime axetil, cefaclor, and cephalexin in the treatment of urinary tract infections in adults. Curr Ther Res 1987 Jul; 42(1): 124–37
Cooper J, Raeburn A, Brumfitt W, et al. Comparative efficacy and tolerability of cephradine and cefuroxime axetil in the treatment of acute dysuria and/or frequency in general practice. Br J Clin Pract 1992; 46(1): 24–7
Vieiralves LFA, Lucena R, Borges CH, et al. Comparative study of cefetamet pivoxil and cefuroxime axetil in complicated urinary tract infections. Drug Invest 1993 Dec; 6: 347–52
Das RP, Jones K, Robinson AJ, et al. Cefuroxime axetil to treat gonorrhoea [letter]. Genitourin Med 1988 Dec; 64: 394
Fong IW, Linton W, Simbul M, et al. Comparative clinical efficacy of single oral doses of cefuroxime axetil and amoxicillin in uncomplicated gonococcal infections. Antimicrob Agents Chemother 1986 Aug; 30: 321–2
Reichman RC, Nolte FS, Wolinsky SM, et al. Single-dose cefuroxime axetil in the treatment of uncomplicated gonorrhea: a controlled trial. Sex Transm Dis 1985 Oct–Dec; 12: 184–7
Kinghorn GR, Spencer RC, Smith TK, et al. Comparative study of cefuroxime axetil and procaine penicillin in the treatment of uncomplicated gonorrhoea. Int J STD AIDS 1990 Jul; 1: 285–7
BaddourLM, Gibbs RS, Mertz G, et al. Clinical comparison of single-oral-dose cefuroxime axetil and amoxicillin with probenecid for uncomplicated gonococcal infections in women. Antimicrob Agents Chemother 1989 Jun; 33: 801–4
Gottlieb A, Mills J. Cefuroxime axetil for treatment of uncomplicated gonorrhea. Antimicrob Agents Chemother 1986 Aug; 30: 333–4
Schift R, Van Ulsen J, Ansink-Schipper MC, et al. Comparison of oral treatment of uncomplicated urogenital and rectal gonorrhoea with cefuroxime axetil ester or clavulanic acid potentiated amoxycillin (Augmentin). Genitourin Med 1986 Oct; 62: 313–7
Wanas TM, Williams PE. Oral cefuroxime axetil compared with oral ampicillin in treating acute uncomplicated gonorrhoea. Genitourin Med 1986 Aug; 62: 221–3
Chaisilwattana P, Osborne NG. Antibiotic treatment of Neisseria gonorrhoeae infections in women. J Gynecol Surg 1994; 10(1): 55–6
Parish LC, Cocchetto DM, Werner K, et al. Cefuroxime axetil in the treatment of cutaneous infections. Int J Dermatol 1987 Jul–Aug; 26: 389–93
Gooch WM, Kaminester L, Cole GW, et al. Clinical comparison of cefuroxime axetil, cephalexin and cefadroxil in the treatment of patients with primary infections of the skin or skin strutures. Dermatologica 1991; 183: 36–43
Jacobs RF, Brown WD, Chartrand S, et al. Evaluation of cefuroxime axetil and cefadroxil suspensions for treatment of pediatric skin infections. Antimicrob Agents Chemother 1992 Aug; 36: 1614–8
Gudgeon AC, Vandenburg MJ, Wight LJ, et al. Is oral cefuroxime axetil suitable for the treatment of unidentified bacterial infection of skin and soft tissue? Br J Clin Pract 1987 Oct; 41: 954–6
Watts HF, Williams AH, Cox DM. A pilot study of cefuroxime axetil (Zinnat) and Augmentin in the treatment of skin and soft tissue infections in general practice. Clin Trials J 1987; 24(5): 356–63
Luger SW, Paparone P, Wormser GP, et al. Comparison of cefuroxime axetil and doxycycline in treatment of patients with early Lyme disease associated with erythema migrans. Antimicrob Agents Chemother 1995 Mar; 39: 661–7
Nadelman RB, Luger SW, Frank E, et al. Comparison of cefuroxime axetil and doxycycline in the treatment of early Lyme disease. Ann Intern Med 1992 Aug 15; 117: 273–80
Arnez M, Radsel-Medvescek A, Pleterski-Rigler D, et al. Comparison of cefuroxime axetil and phenoxymethyl penicillin for the treatment of children with solitary erythema migrans. Wien Klin Wochenschr 1999 Dec 10; 111: 916–22
Hilton E, Rindos P. A comparison of cefuroxime axetil versus doxycycline in the treatment of late Lyme disease [abstract]. Clin Infect Dis 1998 Oct; 27: 950
Rittenhouse BE, Stinnett AA, Dulisse B, et al. An economic evaluation of levofloxacin versus cefuroxime axetil in the outpatient treatment of adults with community-acquired pneumonia. Am J Man Care 2000; 6(3): 381–9
Gleason PP, Guay DRP, Piper B, et al. Comparison of erythromycin, clarithromycin, amoxicillin/clavulanate, and cefuroxime axetil for treatment of outpatient community-acquired pneumonia: a cost analysis [abstract]. 39th Interscience Conference on Antimicrobial Agents and Chemotherapy; 1999 Sep 26, San Francisco (CA), 741
Gleason PP, Kapoor WN, Stone RA, et al. Medical outcomes and antimicrobial costs with the use of the American Thoracic Society Guidelines for outpatients with community-acquired pneumonia. JAMA 1997; 278(1): 32–9
Malfair SC, Frighetto L, Nickoloff DM, et al. Evaluation of the use of cefuroxime and cefuroxime axetil in an intravenousoral stepdown program. Ann Pharmacother 1996 Apr; 30: 337–42
GlaxoWellcome. Summary of product characteristics: Zinnat. GlaxoWellcome, UK; 2000
GlaxoWellcome. Zinnat tablets and suspension. In: ABPI Compendium of data sheets and summaries of product characteristics 1999–2000. London: Datapharma Publications Limited, 2000: 534–5
Mosby. Cefuroxime axetil. In: Rabbitt KE, editor. Mosby’s GenRx. 11th ed. Mussouri: Mosby’s Inc, 2001: 459–63
American Society of Hospital Pharmacists. Cefuroxime axetil. In: McEnvoy GK, editor. AHFS Drug Information. Bethesda: Datapharma Publication Limited, 2000: 215–24
Balter SE, Dowell SF. Update on acute otitis media. Curr Opin Infect Dis 2000; 13(2): 165–70
McCracken Jr GH. Prescribing antimicrobial agents for treatment of acute otitis media. Pediatr Infect Dis J 1999; 18(12): 1141–6
Garau J. Basing empiric treatment choices for respiratory tract infection on the results of the Alexander Project. J Chemother 1999; 11: 51–5
Hoppe HL, Johnson CE. Otitis media: focus on antimicrobial resistance and new treatment options. Am J Health Syst Pharm 1998 Sep 15; 55: 1881–97. quiz 1932–3
Pichichero ME. Acute otitis media: Part II. Treatment in an era of increasing antibiotic resistance. Am Fam Physician 2000; 61(8): 2410–6
McCracken Jr GH, Klein JO. Treatment of acute otitis media in an era of increasing microbial resistance. Pediatr Infect Dis J 1998; 17(6): 576–80
Dowell SF, Butler JC, Giebink GS, et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance —a report from the Drug-resistant Streptococcus Pneumoniae Therapeutic Working Group. Pediatr Infect Dis J 1999 Jan; 18: 1–9
Dowell SF, Butler JC, Giebink GS. Acute otitis media: management and surveillance in an era of pneumococcal resistance. Drug-Resistant Streptococcus Pneumoniae Therapeutic Working Group. Nurse Pract 1999 Oct; 24 (10 Suppl.): 1–9. quiz 15–6
Hamer DH. IDCP guidelines: epiglottitis and otitis. Infect Dis Clin Pract 1997; 6(8): 500–5
Noyek A, Brodovsky D, Coyle S, et al. Classification, diagnosis and treatment of sinusitis: evidence-based clinical practice guidelines. Can J Infect Dis 1998 Jul–Aug; 9 Suppl. B: 3–24
Bartlett JG. IDCP guidelines: management of upper respiratory tract infections. Infect Dis Clin Pract 1997 May; 6: 212–20
Antimicrobial treatment guidelines for acute bacterial rhinosinusitis: Sinus and allergy health partnership. Otolaryngol Head Neck Surg 2000; 123(1) Suppl. Pt 2: S1–32
Brook I, Gooch III WM, Reiner SA, et al. Medical management of acute bacterial sinusitis: recommendations of a clinical advisory committee on pediatric and adult sinusitis. Ann Otol Rhinol Laryngol 2000; 109(5): 2–20
Weiss LR. Developing cost-effective guidelines for the appropriate use of antimicrobial therapy in respiratory tract infection. Am J Man Care 1998 Oct; 4 Suppl.: S572-590
Bartlett JG, Breiman RF, Mandell LA, et al. Communityacquired pneumonia in adults: guidelines for management. Clin Infect Dis 1998 Apr; 26: 811–38
Heffelfinger JD, Dowell SF, Jorgensen JH, et al. Management of community-acquired pneumonia in the era of pneumococcal resistance: a report from the Drug-Resistant Streptococcus Pneumoniae Therapeutic Working Group. Arch Intern Med 2000 May 22; 160: 1399–408
Huchon G, Woodhead M, Gialdroni-Grassi G, et al. Management of adult community-acquired lower respiratory tract infections. European Study of Community Acquired Pneumonia (ESOCAP) Committee. Eur Respir Rev 1998; 8: 391–426
Huchon G, Woodhead M, Gialdroni-Grassi G, et al. Guidelines for the management of adult community-acquired lower respiratory tract infections. Eur Respir J 1998; 11: 986–91
Blumer JL. Fundamental basis for rational therapeutics in acute otitis media. Pediatr Infect Dis J 1999; 18(12): 1130–40
Pichichero ME, Reiner SA, Brook I, et al. Controversies in the medical management of persistent and recurrent acute otitis media: recommendations of a clinical advisory committee. Ann Otol Rhinol Laryngol 2000; 109(8) Suppl. 183: 2–12
Klugman KP, Feldman C. The clinical relevance of antibiotic resistance in the management of pneumococcal pneumonia. Infect Dis Clin Pract 1998; 7(4): 180–4
Schito GC, Debbia EA, Marchese A. The evolving threat of reistance in Europe: new data from the Alexander Project. J Antimicrob Chemother 2000; 46 Topic T1: 3–9
Harrison CJ. Using antibiotic concentrations in middle ear fluid to predict potential clinical efficacy. Pediatr Infect Dis J 1997; 16 Suppl. 2: S12–6
Steele RW, Estrada B, Begue RE, et al. A double-blind taste comparison of pediatric antibiotic suspensions. Clin Pediatr 1997; 36(4): 193–9
Schwartz RH. Enhancing children’s satisfaction with antibiotic therapy: a taste study of several antibiotic suspensions. Curr Ther Res Clin Exp 2000; 61(8): 570–81
Siegel R. How short can courses be in lower respiratory tract infections? J Int Med Res 2000; 28 Suppl. 1: 37–47
Adam D. Short-course antibiotic therapy for infections with a single causative pathogen. J Int Med Res 2000; 28 Suppl. 1: 13A–24A
Pichichero ME, Cohen R. Shortened course of antibiotic therapy for acute otitis media, sinusitis and tonsillopharyngitis. Pediatr Infect Dis J 1997; 16(7): 680–95
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: K. Alexander, Duke University Medical School, Department of Paediatrics, Durham, North Carolina, USA; G.W. Amsden, Clinical Pharmacology Research Center, Bassett Healthcare, Cooperstown, New York, USA; A.C. Fluit, University Hospital Utrecht, Utrecht, The Netherlands; K.G. Naber, Hospital St Elisabet, Straubing, Germany; S. Nadel, St Mary’s Hospital, Department of Paediatric Intensive Care, London, England; S.R. Norrby, Swedish Institute for Infectious Control, Solna, Sweden; M.E. Pichichero, University of Rochester Medical Center, Department Microbiology/Immunology, Rochester, New York, USA.
Data Selection
Sources: Medical literature published in any language since July 1996 on Cefuroxime Axetil, identified using Medline and EMBASE, supplemented by AdisBase (a proprietary database of Adis International). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: Medline search terms were ‘Cefuroxime Axetil’ or ‘cefuroxime’. EMBASE search terms were ‘Cefuroxime Axetil’ or ‘cefuroxime’. AdisBase search terms were ‘Cefuroxime Axetil’. Searches were last updated 27th July 2001.
Selection: Studies in patients with various infections who received cefuroxime axetil. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: cefuroxime axetil, cefuroxime, bacterial infections, antibacterials, pharmacodynamics, SENTRY, Alexander, pharmacokinetics, therapeutic use.
Rights and permissions
About this article
Cite this article
Scott, L.J., Ormrod, D. & Goa, K.L. Cefuroxime Axetil. Drugs 61, 1455–1500 (2001). https://doi.org/10.2165/00003495-200161100-00008
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200161100-00008