Abstract
Hyperactive performance monitoring is a robust finding in obsessive–compulsive disorder (OCD). Patients show increased amplitudes of the error-related negativity (ERN) and correct-related negativity (CRN). Recently, two temporo-spatial factors were shown to contribute to both ERPs in healthy individuals. In the present study, it was investigated whether the factor structure underlying ERN and CRN is similar in OCD and which factors differ between groups. A principal component analysis (PCA) was employed to investigate the temporo-spatial factor structure of ERN and CRN. Twenty-six OCD patients and 26 healthy controls conducted a flanker task. EEG data were analyzed as conventional ERP components and as factor scores derived from temporo-spatial PCA. ERP results showed expected increases in ERN and CRN amplitudes in OCD patients. For both groups, the PCA confirmed the assumed factor structure of a central and a fronto-parietal factor contributing to ERN and CRN. Factor scores of both factors were differently affected by response correctness in OCD. Alterations in factor scores indicate increased activity in both an outcome-independent monitoring process and an error-sensitive process, contributing to overactive performance monitoring in OCD.
Similar content being viewed by others
Introduction
Obsessive–compulsive disorder (OCD) is a severe psychopathological condition characterized by symptoms of recurring intrusive thoughts or impulses (obsessions) and/or repetitive actions and rituals (compulsions) with various manifestations (DSM–IV, APA, 2000). Neurobiological models of OCD are based on findings from neuroimaging studies, indicating overactivity in fronto-striatal brain regions (Aouizerate et al., 2004; Menzies et al., 2008), altered connectivity patterns (Beucke et al., 2013), and structural abnormalities (Kuhn et al., 2013). Studies on performance monitoring in OCD have initially been driven by the assumption that OCD symptoms may result from dysfunctional comparisons between actual and intended actions, leading to exaggerated error signals and the feeling that something is “not just right” even in the absence of actual errors (Pitman, 1987). Performance monitoring can be investigated with event-related potentials (ERPs). Errors in reaction time tasks elicit a negative deflection in the ERP, referred to as the error negativity (Ne; Falkenstein, Hohnsbein, Hoormann, & Blanke, 1990) or error-related negativity (ERN; Gehring, Goss, Coles, Meyer, & Donchin, 1993). The ERN appears as a sharp negative deflection, reaching its maximum about 50–100 ms after the onset of an erroneous response. The anterior cingulate cortex (ACC) or, more precisely, the posterior medial frontal cortex has been commonly suggested as the neural source of the ERN (Debener et al., 2005). Notably, some studies also have reported a similar component following correct responses, the correct-related negativity (CRN; Coles, Scheffers, & Holroyd, 2001; Ford, 1999; Vidal, Burle, Bonnet, Grapperon, & Hasbroucq, 2003; Vidal, Hasbroucq, Grapperon, & Bonnet, 2000). The CRN resembles the ERN with respect to time course but is characterized by a slightly different topography (Vocat, Pourtois, & Vuilleumier, 2008). Despite numerous studies, the relation of both components is still subject to debate, and it remains unclear whether these components reflect similar or different processes. It is mainly discussed whether both components reflect a common process that is differentially active after correct or incorrect responses (Falkenstein, Hoormann, Christ, & Hohnsbein, 2000; Hoffmann & Falkenstein, 2010; Roger, Benar, Vidal, Hasbroucq, & Burle, 2010; Vidal et al., 2000) or whether they reflect different processes (Yordanova, Falkenstein, Hohnsbein, & Kolev, 2004). A recent study provided partial support for both interpretations. With the help of a temporo-spatial principal component analysis (PCA), a combination of two temporo-spatial factors was found to contribute to ERN and CRN (Endrass, Klawohn, Gruetzmann, Ischebeck & Kathmann, 2012). These factors were interpreted as being error-specific and outcome-independent processes, respectively.
Several studies reported increased ERN amplitudes in OCD patients (Endrass, Klawohn, Schuster, & Kathmann, 2008; Endrass et al., 2010; Gehring, Himle, & Nisenson, 2000; Hajcak, Franklin, Foa, & Simons, 2008; Johannes et al., 2001; Riesel, Endrass, Kaufmann, & Kathmann, 2011; Ruchsow et al., 2005; Stern, Liu, et al., 2010), as well as in individuals with obsessive–compulsive symptoms (Grundler, Cavanagh, Figueroa, Frank, & Allen, 2009; Hajcak & Simons, 2002; Santesso, Segalowitz, & Schmidt, 2006). Accordingly, increased ACC activity in OCD patients has also been shown by several imaging studies (Fitzgerald et al., 2005; Maltby, Tolin, Worhunsky, O’Keefe, & Kiehl, 2005; Ursu, Stenger, Shear, Jones, & Carter, 2003). Moreover, the ERN enhancement remained stable even after successful symptom remission with psychotherapy (Hajcak et al., 2008) and was found in unaffected first-degree relatives of OCD patients (Riesel et al., 2011). Hence, ERN alterations were suggested to represent a neurocognitive endophenotype or biomarker of OCD (Olvet & Hajcak, 2008; Riesel et al., 2011). Several studies found not only increased ERN, but also increased CRN amplitudes in OCD (Endrass et al., 2008; Endrass et al., 2010; Hajcak & Simons, 2002; Riesel et al., 2011). Furthermore, brain imaging studies revealed increased ACC activity in OCD patients on error trials as well as on high-conflict trials that were correctly performed (Maltby et al., 2005; Ursu et al., 2003). Taken together, enhanced ERP amplitudes following correct and incorrect actions point toward a general hyperactivity of performance-monitoring-related brain processes in OCD patients. The enhancement of both performance monitoring signals is well in accordance with clinical symptoms of OCD, which are characterized not only by excessive reactions to errors, but also by increased effort to monitor and control actions even when they are correct (Maltby et al., 2005).
ERP studies investigating performance monitoring often also report a later parietal positivity following incorrect responses, the error positivity (Pe; Falkenstein, Hohnsbein, Hoormann, & Blanke, 1991; for a review, see Overbeek, Nieuwenhuis, & Ridderinkhof, 2005). The Pe has been associated with error awareness (Endrass, Franke, & Kathmann, 2005; Endrass, Klawohn, Preuss & Kathmann, 2012) and individual error significance (Falkenstein et al., 2000). Although an increase of Pe amplitudes might be expected in OCD, considering the increased relevance of errors for patients, studies so far did not find alterations of this ERP component in OCD (Endrass et al., 2008; Riesel et al., 2011; Ruchsow et al., 2005).
In conclusion, numerous findings suggest overactive performance monitoring in OCD following incorrect and correct responses. These ERP components (ERN and CRN) have been shown to result from a combination of two topographically distinct temporo-spatial factors. A previous study using a temporo-spatial PCA revealed two temporo-spatial factors contributing to ERN and CRN (Endrass, Klawohn, Gruetzmann, et al., 2012). These factors were characterized by a central and a fronto-parietal distribution, respectively. The central factor varied between correct and incorrect responses and, therefore, was suggested to reflect error-sensitive processing. However, the fronto-parietal factor was found active for both response types and, therefore, was suggested to reflect outcome-independent processing or general response monitoring. With the present study, we examined these subcomponents of performance monitoring in OCD. Thus, we expected to replicate the previously reported two-factor solution contributing to ERN and CRN. Furthermore, we examined underlying components of performance monitoring in OCD patients, since group differences regarding the differential contribution of these factors might indicate which one of the assumed processes is disturbed in OCD. On the basis of enhanced ERN and CRN amplitudes in previous studies, a selective alteration of error processing appears unlikely.
Method
Participants
Twenty-six patients with OCD (15 female) and 26 healthy control (HC) participants (15 female) took part in the present study. All participants volunteered for the investigation and received monetary compensation. In accordance with the ethical guidelines of the Declaration of Helsinki, all participants gave written informed consent prior to the experiment. Demographic and clinical characteristics of OCD and HC groups are displayed in Table 1. All OCD patients met DSM–IV criteria for OCD and were seeking or receiving treatment at the specialized outpatient clinic at Humboldt-Universität zu Berlin. Diagnoses were made by trained clinical psychologists after conducting the Structured Clinical Interview for DSM–IV (SCID–I, German version; Wittchen, Zaudig, & Fydrich, 1997). Obsessive–compulsive symptom severity was determined with the Yale–Brown Obsessive Compulsive Scale (Y-BOCS; Goodman et al., 1989). Sixteen OCD patients had current comorbid diagnoses: affective disorder (n = 13), anxiety disorder (n = 9), personality disorder (n = 7), eating disorder (n = 3), and posttraumatic stress disorder (n = 1). Patients with comorbid psychotic or substance disorders were not included. Twelve OCD patients took psychotropic medication (selective serotonin reuptake inhibitors, SSRIs). HC participants were free of past and present mental disorders and were carefully matched to the patient group with respect to age, gender, and verbal intelligence, as measured with a German vocabulary test (WST; Schmidt & Metzler, 1992). Furthermore, all participants were examined with the Obsessive–Compulsive Inventory–Revised (OCI–R; Foa et al., 2002) and rated their depressive symptoms with the Beck Depression Inventory–II (BDI–II; Steer, Ball, Ranieri, & Beck, 1997). All participants had normal or corrected-to-normal vision, and none of the participants had a history of head trauma or neurological disease.
Task and experimental procedure
We employed an arrow version of the flanker task (Eriksen & Eriksen, 1974; Kopp, Rist, & Mattler, 1996) displayed using Presentation software (Neurobehavioral Systems Inc., Albany, CA). Participants were instructed to respond with their left and right index fingers according to the direction of the arrow located in the middle. Half of the trials were compatible (i.e., target and flankers pointing in the same direction); the other half were incompatible (i.e., target and flankers pointing in opposite directions). Stimuli were presented in pseudorandomized order regarding compatibility and target direction. Each trial started with the presentation of a fixation stimulus lasting 900–1,500 ms (M = 1,200 ms). Flanker stimuli were presented 100 ms in advance of the target stimulus, which was then displayed together with flankers for another 50 ms. During the time window of the required response, a fixation stimulus was presented again for 1,000 ms. Overall, 480 trials were presented in eight blocks with short breaks in between, resulting in a total task duration of approximately 25 min. The importance of speed and accuracy was equally emphasized in the instruction.
EEG recording and ERP analysis
Electroencephalographic (EEG) recordings were acquired with 65 electrodes, including Cz as recording reference. Electrodes were positioned using electrode caps with 61 equidistant electrode locations (EasyCap, Hersching, Germany). In addition, 4 external electrodes were placed below the left and right eyes (IO1, IO2), as well as at the nasion and neck. The ground electrode was placed below T1. All electrode impedances were below 5 kΩ. Continuous EEG recordings were conducted with BrainAmp amplifiers (BrainProducts, Gilching, Germany) at a sampling rate of 500 Hz and were amplified with a band-pass filter of 0.1–100 Hz.
For ERP analysis, continuous EEG data were filtered offline with a high-pass filter of 0.5 Hz (24 db/Oct) and a low-pass filter of 40 Hz (24 db/Oct) and were then rereferenced to average reference. Correction for eye movement and blink artifacts was applied using the multiple-source eye correction method (Berg & Scherg, 1994) as implemented in BESA 5.1 (Brain Electrical Source Analysis, MEGIS Software GmbH, Gräfelfing, Germany). Subsequently, epochs of 1,000 ms, comprising 200 ms prior to and 800 ms after the first response on each trial, were extracted. Epochs that contained amplitude changes of more than 300 μV or voltage steps between consecutive data points exceeding 50 μV were excluded from analysis by automatic artifact rejection. Baseline correction was conducted by subtracting averaged activity in the first 200 ms of each epoch.Footnote 1 Averages for correct and incorrect responses with reaction times within 100 and 600 ms were computed for each participant. Errors on compatible trials, which were very rare, were excluded from analyses. ERN and CRN amplitudes were quantified as peak-to-peak amplitudes at fronto-central electrodes (FCz, Fz, and Cz). The difference between the most negative peak (0–100 ms) and the preceding positive peak (−50–50 ms) was calculated. Peaks were defined as local maxima and searched semiautomatically in the respective time windows. Pe amplitudes were analyzed as mean amplitudes from 200 to 400 ms postresponse at electrodes FCz, Cz, CPz, and Pz.
Principal component analysis
Response-related ERPs of both groups were submitted to a temporo-spatial PCA. At first, separate PCAs were conducted for each group to verify the factor structure within each group (group-specific PCAs). Then a second temporo-spatial PCA was applied to the whole data set comprising all participants (overall PCA). This analysis provided the possibility of comparing the variability of the resulting factors between groups and response types. For all analyses, we employed a two-step temporo-spatial PCA procedure (Dien, 2010b) implemented in the ERP PCA toolkit 2.06 (Dien, 2010a). A covariance matrix and Kaiser normalization were employed in each PCA described here (Dien, Beal, & Berg, 2005; Kayser & Tenke, 2003). Response-locked individual averages comprising 200 ms before and 800 ms following response were obtained for correct and incorrect responses of each participant (500 data points in time and 65 electrodes). First, a temporal PCA was conducted on averages of each participant for correct and incorrect responses. A Promax rotation was used, and the number of extracted factors was limited by the resulting scree plot. Second, the spatial distribution of these factor scores was analyzed using a spatial PCA (Infomax rotation). Separate spatial PCAs were applied to each temporal factor, which can be considered to be a virtual epoch. Thereby, the temporo-spatial PCA reveals temporo-spatial factors, which are characterized by their time course and topography. Factor scores are extracted for each condition and participant. For the group-specific PCAs, equivalent numbers of temporal and spatial factors were extracted for both groups. From all PCA results, only those temporo-spatial factors accounting for more than 1 % of the total variance in the data were considered for further analysis (Foti, Hajcak, & Dien, 2009; Foti, Weinberg, Dien, & Hajcak, 2011; Kayser & Tenke, 2005). Please note that the amount of explained variance by one factor is related to the total variance in the data—that is, all time points and all electrodes. Factor scores of these temporo-spatial factors were then averaged across participants separately for correct and incorrect responses (“virtual ERPs”). Since we were interested in PCA components reflecting ERN/CRN activity, temporal factors were selected on the basis of their temporal characteristics (peak latency) (Dien et al., 2005; Dien, Michelson, & Franklin, 2010; Foti et al., 2011). Furthermore, remaining temporo-spatial factors were examined with regard to differences between groups or correct and incorrect responses.
Statistical analysis
Behavioral data were analyzed with respect to error rates and reaction times. Error rates were compared between groups by independent samples t-test. Reaction times were analyzed with repeated measures analyses of variance (ANOVAs) including the within-subjects factor of response type (correct vs. incorrect) and the between-subjects factor of group (OCD vs. HC). ERP amplitudes were statistically analyzed with repeated measures ANOVAs including the within-subjects factors of response type and electrode (FCz, Fz, vs. Cz), and the between-subjects factor of group. Factor scores of the temporo-spatial factors contributing to ERN and CRN were submitted to statistical analysis using a repeated measurement ANOVA with response type as a within-subjects factor and group as a between-subjects factor. Analysis of Pe amplitudes was performed by a repeated measures ANOVA including the factors of response type and electrode (FCz, Cz, CPz, Pz) and the between-subjects factor of group. Effects of psychotropic medication on ERP, as well as PCA data, were analyzed for the OCD group by repeated measurement ANOVAs with response type as a within-subjects factor and medication (medicated, unmedicated) as a between-subjects factor. For all analyses, Greenhouse–Geisser correction and Bonferroni correction were applied when appropriate. Subsequent to the PCA and the selection of relevant temporo-spatial factors, two multiple linear regression analyses with backward elimination were conducted to predict the relative contributions of selected factors to the ERN and CRN, quantified as mean amplitudes at Fz electrodes.
Results
Behavioral data
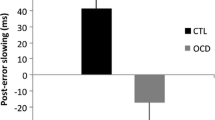
Behavioral results can be found in Table 2. There were no significant group differences with respect to reaction times or error rates (both ps > .05). A significant main effect of response type on reaction times was found, F(1, 50) = 1,395.49, p < .001, η 2 = .965, indicating that reaction times were shorter for errors than for correct responses. This difference was present for both groups, since neither the interaction of response type with group, F(1,50) = 1.18, p = .282, nor the main effect of group, F(1,50) = 0.20, p = .887, was significant.
ERP results
Response-locked ERPs for both groups are displayed in Fig. 1. For both experimental groups, ERN and CRN are present as negative deflections at fronto-central electrodes peaking about 50 ms after response execution. Mean peak amplitudes are presented in Table 2. The repeated measures ANOVA of response-related negativity peak amplitudesFootnote 2 revealed significant main effects of response type, F(1, 50) = 98.82, p < .001, η 2 = .664, with ERN amplitudes being higher than CRN amplitudes, and electrode, F(2, 100) = 21.18, p < .001, η 2 = .298, ε = .688, as well as group, F(1, 50) = 8.71, p = .005, η 2 = .148. Moreover, significant interaction effects were found for response type with electrode, F(2, 100) = 75.09, p < .001, η 2 = .600, ε = .678, and response type with group, F(1, 50) = 4.37, p = .042, η 2 = .080, as well as for response type, electrode, and group, F(2, 50) = 3.62, p = .049, η 2 = .067, ε = .678, whereas the interaction of electrode with group was not significant, F(2, 100) < 1.5. Post hoc analyses concerning the interactions of response type with group revealed that the ERN–CRN difference was present in both experimental groups (all ps < .01), but more pronounced for the OCD group (6.23 μV) than in HCs (4.12 μV). Furthermore, post hoc analysis of the interaction of response type and electrode, as well as the three-way interaction, indicates a difference in electrode location of maximal amplitudes for ERN and CRN, which was present in groups. ERN peaks were most prominent and of similar amplitude at FCz and Cz (p > .30) and significantly larger than at Fz (all ps < .05). CRN amplitudes did not differ significantly between Fz and FCz (p > .60), and amplitudes at these electrodes were significantly larger than at Cz (both ps < .005). In addition, post hoc analyses of the three-way interaction showed significant group differences in ERN amplitudes at all electrode sites (all ps < .05), whereas group differences in CRN amplitude were present at statistical trend level at electrodes Fz, t(50) = 1.87, p = .067, and FCz, t(50) = 1.73, p = .089, and not at Cz, t(50) = 0.82, p = .418.
Pe amplitudes were more positive for erroneous than for correct responses, F(1, 50) = 125.79, p < .001, η 2 = .716. The significant main effect of electrode, F(3, 150) = 36.40, p < .001, η 2 = .421, and the interaction of electrode and response type, F(3, 150) = 13.79, p < .001, η 2 = .216, suggest that this difference varied between electrodes. The correctness effect was significant at all electrodes (all ps < .001) but was more pronounced at Cz, CPz, and Pz (mean difference: >5.29 μV) relative to FCz (mean difference: 3.52 μV). A significant main effect of group or an interaction of response type and group was not found, F(1, 50) < 1.5. However, the interaction of electrode and group, F(3, 150) = 5.30, p = .012, η 2 = .096, and the three-way interaction, F(3, 150) = 2.92, p = .036, η 2 = .055, were significant. The difference between erroneous and correct responses was significant at all electrodes sites and in both groups (all ps < .01). However, OCD patients showed reduced positivity for error trials at FCz, as compared with HCs, t(50) = 2.44, p = .018.
The analysis of ERN/CRN peak latencies revealed a shorter peak latency for CRN (M = 40 ms) than for ERN (M = 60 ms) amplitudes, F(1, 50) = 33.81, p < .001, η 2 = .403. No main effect of group or interaction of response type and group was found, F(1, 50) < 1.0, p > .4.
Additionally, the influence of medication on ERN and CRN peak amplitudes was analyzed. Neither a significant main effect of medication, F(1, 24) = 0.89, p = .353, nor an interaction of medication and response type, F(1, 24) = 1.57, p = .222, was found. However, the analysis of mean amplitudes revealed a trend for attenuated ERN and CRN amplitudes in patients who were currently taking SSRIs, as compared with patients without current medication, F(1, 24) = 2.95, p = .099, η 2 = .109 (see Fig. 2).
PCA results
The results of the two group-specific PCAs revealed two temporo-spatial factors contributing to ERN and CRN. In each group, 12 temporal factors were extracted with Promax rotation and four spatial factors for the Infomax rotation. For both groups, the PCA yielded two temporo-spatial factors corresponding to ERN and CRN, peaking at 62 ms for the HC group and at 74 ms for the OCD group. One factor was characterized by a central topographical maximum, and the other factor by a frontal negativity and a parietal positivity (fronto-parietal factor; Fig. 3). Significant main effects of response type were obtained for the central factor (TF4-SF1) in OCD patients, F(1, 25) = 111.12, p < .001, η 2 = .816, and in HCs, F(1, 25) = 25.99, p < .001, η 2 = .510, respectively. In contrast, for the fronto-parietal factor (TF4-SF2), a significant main effect of response type was found only in the patient group, F(1, 25) = 11.08, p = .003, η 2 = .307, but not in the control group, F(1, 25) = 2.55, p = .123, η 2 = .092.
The overall PCA yielded 12 temporal factors and 4 spatial factors, resulting in 48 temporo-spatial factor combinations. With respect to the ERN/CRN time window, the temporo-spatial PCA yielded one relevant temporal factor (TF4) peaking at 70 ms, with two of the corresponding temporo-spatial factors uniquely accounting for more than 1 % of total variance (TF4-SF1 and TF4-SF2). Time courses (“virtual ERPs”) and topographies of both temporo-spatial factors assumed to correspond to ERN and CRN are presented in Fig. 4 for both groups. One factor (TF4-SF1) uniquely accounted for 2.33 % of total variance in the solution and displayed a central topography. Statistical analysis of factor scores by repeated measures ANOVA confirmed a significant variation of the central factor with response type, F(1, 50) = 116.12, p < .001, η 2 = .699, as well as with group, F(1, 50) = 7.94, p = .007, η 2 = .137. The interaction of response type and group reached only a statistical trend level, F(1, 50) = 3.68, p = .061, η 2 = .069. Examination of the response type effect showed that factor scores were negative for errors and positive for correct responses in both groups [HC and OCD, both ts(25) > 5.5, p < .001]. Furthermore, factor scores of errors were more negative in OCD patients than in HCs, t(50) = 2.96, p = .005, whereas the group difference in factor scores for correct responses was not significant, t(50) = 1.32, p = .193. The second temporo-spatial factor (TF4-SF2) accounted for 1.30 % of variance in the solution and was characterized by a frontal negativity along with a parietal positivity.Footnote 3 Statistical analysis revealed a significant main effect of response type, F(1, 50) = 14.08, p < .001, η 2 = .220, further qualified by a significant interaction of response type and group, F(1, 50) = 4.07, p = .049, η 2 = .075, while no significant main effect of group was found, F(1, 50) = 1.36, p = .249, η 2 = .027. Factor scores of the fronto-parietal factor were, in general, more negative for correct than for incorrect responses, but when analyzed separately for both groups, this difference was significant only for OCD patients, t(25) = 3.95, p < .001, but not for HC, t(25) = 1.27, p = .216. Furthermore, factor scores corresponding to correct responses were significantly more negative for the OCD group than for the control group, t(50) = 2.03, p = .048, whereas both groups did not differ with respect to factor scores corresponding to errors, t(50) = 0.05, p = .957.
Two multiple linear regression analyses were conducted to predict contributions of both temporo-spatial factors to ERPs of incorrect and correct responses. Results indicate that both factors significantly contribute to ERN, R 2 = .863, F(2, 49) = 154.78, p < .001, as well as CRN amplitudes, R 2 = .806, F(2, 49) = 101.821, p < .001. The central factor (TF4SF1) and fronto-parietal factor (TF4SF2) contributed both to ERN [β = .841, t(49) = 1 5.61, p < .001; β = .262, t(49) = 4.86, p < .001] and CRN [β = .800, t(49) = 12.60, p < .001; β = .313, t(49) = 4.93, p < .001] amplitudes.
Furthermore, the possible influence of medication on PCA factors was examined. For the central factor (TF4SF1), a significant main effect of medication was present, F(1, 24) = 5.58, p = .027, η 2 = .189, indicating that factor scores were more pronounced in the unmedicated patients subgroup (please see Fig. 2). This difference was not significantly modulated by response type (p > .8). The fronto-parietal factor (TF4SF2) did not display a significant main effect of medication or interaction of response type and medication (p > .4).
Besides the above described factors contributing to ERN and CRN, further temporo-spatial factors were identified by the PCA. Factors accounting for more than 1 % of total variance in the data and showing significant modulations between groups or response types will be described. Within the first temporal factor, corresponding to a late slow wave potential peaking at 654 ms, one temporo-spatial factor displayed a significant effect of response type, F(1, 50) = 70.0, p > .001, η 2 = .583, and is characterized by a larger centro-parietal negativity for correct responses.
Furthermore, within the second temporal factor (latency of 214 ms), one temporo-spatial factor (TF2SF1) varied with response type, F(1, 50) = 201.60, p < .001, η 2 = .801, and is characterized by a larger parietal positivity for errors. The second temporo-spatial factor (TF2SF2) displaying a fronto-central positivity and factor scores showed a main effect of response type, F(1, 50) = 8.53, p = .005, η 2 = .146, as well as of group, F(1, 50) = 9.88, p = .003, η 2 = .165, and a significant interaction of response type and group, F(1, 50) = 4.28, p = .044, η 2 = .079. Post hoc tests indicate more positive factor scores for incorrect than for correct responses only for the control group, t(25) = 4.71, p < .001, but not the OCD group, t(25) = 0.50, p = .620, and a significant group difference was observed only for error trials, t(50) = 3.52, p = .001.
Within the third temporal factor (394 ms), two relevant temporo-spatial factors were identified, characterized by a parietal positivity (TF3SF1) and a central positivity (TF3SF2). Factor scores of both temporo-spatial factors were more positive for incorrect than for correct responses, F(1, 50) = 43.74, p < .001, η 2 = .467, and F(1, 50) = 36.21, p < .001, η 2 = .420, respectively.
Finally, within the fifth temporal factor (−16 ms), one temporo-spatial factor (TF5SF1) was characterized by a frontal negativity and displayed a more negative deflection for incorrect than for correct responses, F(1, 50) = 18.87, p < .001, η 2 = .274. This factor might reflect the baseline difference between correct and incorrect trials.
Discussion
This study investigated performance monitoring following correct and incorrect responses in patients with OCD and HCs. ERP analysis confirmed earlier findings in that ERN and CRN amplitudes were enlarged for the OCD group, as compared with HCs, although this increase was more pronounced for the ERN than for the CRN (Endrass et al., 2008; Gehring et al., 2000; Hajcak et al., 2008; Johannes et al., 2001; Riesel et al., 2011; Ruchsow et al., 2005). In addition to ERP analysis, a temporo-spatial PCA was used to examine underlying factors contributing to ERN and CRN (Endrass, Klawohn, Gruetzmann, et al., 2012). The aim was to replicate the previously found factor configuration in patients with OCD and, most important, to examine how amplitude enhancements of ERN and CRN in OCD relate to alterations of these underlying factors.
The group-specific PCAs replicated the previously reported two-factor structure underlying ERN and CRN (Endrass, Klawohn, Gruetzmann, et al., 2012) independently in both groups. A central and a fronto-parietal factor were identified in this study, which strongly resemble those of our prior investigation with respect to time course, topographies, and modulations. Importantly, this factor solution was found using a flanker task, while our previous study employed a visual discrimination task. Hence, the present results confirm two PCA factors, both contributing to ERN and CRN. Notably, this factor structure was identical in the OCD group, with topographies and time courses remarkably similar to those in control participants. Thus, overactive performance monitoring in OCD appears to rely on the same underlying brain activities that may differentially contribute to ERN and CRN components.
The question of whether PCA factors differentially contribute to performance monitoring in patients and controls was addressed with an overall PCA including both groups. Interestingly, group differences were obtained for both PCA factors. The error-sensitive centrally distributed factor was more pronounced for errors in the patient group, as compared with healthy controls. In contrast, the second factor showing a frontal negativity and a parietal positivity and formerly shown as outcome independent (Endrass, Klawohn, Preuss, et al., 2012) varied between groups only on correct, but not incorrect, responses. While this factor was insensitive for response correctness in healthy participants, factor scores were more negative for correct than for incorrect responses in OCD patients.
Group differences with regard to an error-sensitive process are well in line with previous studies showing larger ERN amplitudes in OCD patients, as compared with HCs (Endrass et al., 2008; Riesel et al., 2011). The potential source of this centrally distributed factor was found to be located within the posterior medial frontal cortex (Endrass, Klawohn, Gruetzmann, et al., 2012), most likely in the dorsal ACC or supplementary motor area. Increased activity of that factor during error trials would also be in line with functional imaging studies reporting increased ACC activity for OCD patients after errors (Fitzgerald et al., 2005; Ursu et al., 2003). Beyond that, patients with OCD report great preoccupation with the occurrence of errors, with special emphasis on their negative valence and the importance of preventing their occurrence. This is in line with findings of Stern et al. (2011), who found patients with OCD more strongly flustered and frustrated by errors.
Findings with regard to the second factor, which was insensitive for response correctness in healthy participants, are more difficult to interpret. The function of this factor as a general performance-monitoring process still needs clarification and further investigation (Endrass, Klawohn, Gruetzmann, et al., 2012). However, OCD patients show more negative factor scores for correct than for erroneous responses. The increased activation might correspond to an amplified evaluation effort or a sensation of doubt regarding the correctness of the given response in OCD patients that is absent on trials when an error is clearly present and doubt is replaced by error processing, reflected by the central factor. Among various individual manifestations of OCD symptoms, a common aspect is the occurrence of “not-just-right experiences,” unsettling sensations of imperfection and error (Coles, Frost, Heimberg, & Rheaume, 2003). These subjective experiences may contribute to a perfectionistic trait in OCD patients (Ghisi, Chiri, Marchetti, Sanavio, & Sica, 2010). Most compulsive behaviors can be conceptualized as “evidence gathering” behavior in order to reduce distress resulting from not-just-right experiences and uncertainty (Stern et al., 2012). The present finding of altered general performance monitoring and also enhanced CRN amplitudes could represent the underlying neural basis of these symptoms. Furthermore, OCD patients not only express concern about errors, but also strongly worry about the correctness of their actions and the avoidance of possible future errors. Exaggerated monitoring, or dysfunctional error signaling during correct actions in combination with overactive error monitoring, may provide a better model of OCD symptoms such as persistent doubt or a not-just-right experience (Maltby et al., 2005).
In conclusion, the two factors found to contribute to ERN and CRN were assumed to correspond to different aspects of performance monitoring. While the central factor was suggested to reflect error-sensitive processing, the fronto-parietal factor might reflect outcome-independent general monitoring activity, which is more strongly activated in OCD patients on correct trials, possibly indicating increased doubt about action correctness. The present results suggest that both aspects of performance monitoring, error-specific processing and general monitoring, are overactive in OCD. Increased activity of both performance-monitoring subprocesses might be equivalent to a state of heightened error significance, also in healthy subjects. In line with this, ERN and CRN amplitudes have been shown to increase when errors are punished, resulting in amplitudes similar to those of OCD patients (Endrass et al., 2010).
Increased error-related brain activity occurs not only in OCD patients, but also in other anxiety disorders (Weinberg, Olvet, & Hajcak, 2010). It was speculated that anxiety as a psychopathological condition might alter performance monitoring qualitatively (Aarts & Pourtois, 2010). However, the present study revealed equivalent PCA factors contributing to response-related negativities in HCs and OCD patients. Thus, performance monitoring in OCD appears to rely on the same underlying brain mechanisms as in HCs, but their functional modulation is significantly altered in OCD. Furthermore, the present study might provide a possible strategy for investigating differential alterations between OCD and other anxiety disorders. Overactive performance monitoring in patients with generalized anxiety disorder (Xiao et al., 2011) and major depression (Chiu & Deldin, 2007) challenges the specificity of overactive performance monitoring to OCD. Interestingly, patients with generalized anxiety disorder showed enhanced ERN amplitudes in one study (Xiao et al., 2011) but enhanced error minus correct amplitudes (∆ERN) in two other studies (Weinberg, Klein, & Hajcak, 2012; Weinberg et al., 2010). Therefore, temporo-spatial PCA could help to elucidate differential alterations between clinical groups.
Additionally, the Pe did not differ between groups, which is consistent with earlier studies in OCD (Endrass et al., 2008; Endrass et al., 2010; Riesel et al., 2011; Ruchsow et al., 2005). Nonetheless, a larger frontal positivity following errors was found in HCs, as compared with OCD patients, while no group difference was found at parietal electrodes. This effect was also observed for a corresponding fronto-central PCA factor (TF2SF2). Interestingly, similar fronto-central positivities were obtained in two previous studies (Arbel & Donchin, 2009; Endrass, Klawohn, Gruetzmann, et al., 2012). Notably, this component resembles the ERN with regard to topographic distribution and was considered as a fronto-central or early Pe component (Endrass, Reuter, & Kathmann, 2007; O’Connell et al., 2007; Ruchsow et al., 2005; Van Veen & Carter, 2002). The early frontal Pe was considered as functionally related to the ERN or even as an inactivation of the ERN (Van Veen & Carter, 2002). In accord with this, similar to the ERN, the early Pe did not vary with error awareness, while the later parietal Pe was reduced for unaware, as compared with aware, errors (Endrass et al., 2007; O’Connell et al., 2007). In contrast, Arbel and Donchin (2009) showed a functional distinction between ERN and early Pe. Only one study examined this component in OCD, and no group difference was observed (Ruchsow et al., 2005). However, a visual inspection of ERP figures of previous studies suggests that a similar reduction of the early Pe component might also have been present in some studies (Endrass et al., 2010; Gehring et al., 2000; Hajcak et al., 2008; Hajcak & Simons, 2002). Nevertheless, the present finding of a reduced frontal Pe and enhanced ERN in OCD patients supports the idea that this component is not a second ERN but that it reflects functionally distinct aspects (Arbel & Donchin, 2009).
Some potential limitations of the present study have to be considered. In the OCD group, several participants were included that were currently taking medication (SSRIs). However, the analysis of medication effects indicates that overactive performance monitoring is not due to psychotropic medication. A trend for attenuated amplitudes was found in patients currently taking SSRIs, as compared with unmedicated patients (Endrass et al., 2008; Riesel et al., 2011; Stern, Liu, et al., 2010). Although this suggests that medication did not interfere with the present findings, further studies should directly examine medication by also considering type and duration of psychotropic medication. Furthermore, the present sample size did not allow for a comparison of different symptom profiles or comorbidity in the patient group. While comorbid disorders are very common among OCD patients and, thus, the patient sample represents a naturalistic OCD group, it would also be interesting to examine a larger group of OCD patients without comorbid diagnoses.
Moreover, while the approach of this study with the use of a temporo-spatial PCA provides new insight into processes assumed to underlie ERPs, some methodic issues have to be considered. The PCA technique examines variations in amplitudes distributed over electrodes and time. However, this method depends on the data entered in the analysis and is sensitive to baseline correction, similar to other methods quantifying ERPs. Thus, a different factor solution would be obtained by entering longer or shorter time intervals or applying baseline correction for a different time period. Further research will be needed to confirm and clarify the underlying factor structure of ERN and CRN. The idea of two underlying factors that could represent error-specific and general monitoring functions is still preliminary (Endrass, Klawohn, Gruetzmann, et al., 2012). Generally, the ACC supports not only error monitoring, but also many other evaluation processes, like response conflict, response outcomes, and pain (Bush, Luu, & Posner, 2000; Rushworth, Buckley, Behrens, Walton, & Bannerman, 2007). Therefore, general performance monitoring, in addition to error processing reflected in response-related negativities, seems plausible but clearly needs further investigation. However, the present finding that the fronto-parietal factor was selectively enhanced on correct trials in OCD patients does not fully support the interpretation that this factor reflects outcome-independent or general performance monitoring. As outlined above, it may rather be attributed to the increased uncertainty or doubt of OCD patients that is present even following correct responses. Still, conclusions are difficult to draw and further studies using different task sets and experimental manipulations are necessary to determine what is reflected by the two identified PCA factors.
This study investigated the underlying PCA factor structure of performance-monitoring-related EEG responses within OCD and HC groups. The temporo-spatial PCA proved to be a useful tool for the investigation of altered performance monitoring in this patient population. Increased amplitudes of response-related negativities, as known from several studies, were distinguished into alterations of two underlying processes represented by two topographically distinct PCA factors. Furthermore, results indicate that hyperactivity of both processes contributes to overactive performance monitoring associated with OCD.
Notes
This baseline was used on the basis of similar baseline intervals in earlier studies (Hajcak, McDonald, & Simons, 2004; Larson, Fair, Good, & Baldwin, 2010; Riesel et al., 2011; Ruchsow et al., 2005) and because it aligns preresponse activity between groups. However, the baseline interval already includes the peak that is preceding the ERN and CRN.
ERP effects were also analyzed as mean amplitudes (0–100 ms postresponse), and results are in accordance with results from peak analysis. Significant main effects were found for response type, F(1, 50) = 101.97, p < .001, η 2 = .671, and electrode, F(2, 100) = 113.41, p < .001, η 2 = .694, ε = .701, as well as group, F(1, 50) = 7.78, p = .007, η 2 = .135. Interactions were found significant for response type with electrode, F(2, 100) = 56.13, p < .001, η 2 = .529, ε = .691, and there was a trend for response type and group, F(1, 50) = 3.12, p = .084, η 2 = .059.
Since this temporo-spatial factor comprised a frontal negativity and parietal positivity, ERP mean amplitudes of ERN and CRN (0–100 ms) were further analyzed by including frontal as well as parietal electrodes. A repeated measures ANOVA was conducted with the factors of group, response type, and caudality (frontal: Fz, FCz; parietal: Cz, CPz). Results indicate significant main effects of response type, F(1, 50) = 79.98, p < .001, η 2 = .615, caudality, F(1, 50) = 245.67, p < .001, η 2 = .831, and group, F(1, 50) = 4.70, p = .035, η 2 = .086. Significant interactions were present for response type with group, F(1, 50) = 4.54, p = .038, η 2 = .083, as well as caudality with group, F(1, 50) = 5.39, p = .024, η 2 = .097, and response type with caudality, F(1, 50) = 18.98, p < .001, η 2 = .275, while the three-way interaction was not significant, F(1, 50) = 0.001, p = .970, η 2 = .000. The response type effect indicates that amplitudes were more negative for errors than for correct responses, while the main effect of caudality indicated that amplitudes were negative at frontal electrodes and positive at parietal electrodes. The interaction of response type and caudality further showed that the difference between errors and correct responses was larger at frontal electrode sites (mean difference: 3.47 μV), as compared with parietal electrode sites (mean difference: 1.5 μV), although it was, in both cases, significant (both ps < .001). The group main effect suggests more negative amplitudes in the OCD group than in the HC group. The interaction of group with caudality indicates that groups differed significantly at frontal electrode sites (p = .006), but not at parietal electrode sites (p = .802).
References
Aarts, K., & Pourtois, G. (2010). Anxiety not only increases, but also alters early error-monitoring functions. Cognitive, Affective, & Behavioral Neuroscience, 10(4), 479–492. doi:10.3758/Cabn.10.4.479
American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (Vol. 4th ed. Text Revision). Washington, DC: American Psychiatric Association.
Aouizerate, B., Guehl, D., Cuny, E., Rougier, A., Bioulac, B., Tignol, J., & Burbaud, P. (2004). Pathophysiology of obsessive-compulsive disorder—A necessary link between phenomenology, neuropsychology, imagery and physiology. Progress in Neurobiology, 72(3), 195–221. doi:10.1016/j.pneurobio.2004.02.004
Arbel, Y., & Donchin, E. (2009). Parsing the componential structure of post-error ERPs: A principal component analysis of ERPs following errors. Psychophysiology, 46(6), 1179–1189. doi:10.1111/j.1469-8986.2009.00857.x
Berg, P., & Scherg, M. (1994). A multiple source approach to the correction of eye artifacts. Electroencephalography and Clinical Neurophysiology, 90(3), 229–241.
Beucke, J. C., Sepulcre, J., Talukdar, T., Linnman, C., Zschenderlein, K., Endrass, T., … Kathmann, N. (2013). Abnormally high degree connectivity of the orbitofrontal cortex in obsessive-compulsive disorder. Journal of the American Medical Association Psychiatry, 70(6), 619–629. doi: 10.1001/jamapsychiatry.2013.173
Bush, G., Luu, P., & Posner, M. I. (2000). Cognitive and emotional influences in anterior cingulate cortex. Trends in Cognitive Sciences, 4(6), 215–222.
Chiu, P. H., & Deldin, P. J. (2007). Neural evidence for enhanced error detection in major depressive disorder. American Journal of Psychiatry, 164(4), 608–616.
Coles, M. E., Frost, R. O., Heimberg, R. G., & Rheaume, J. (2003). “Not just right experiences”: perfectionism, obsessive-compulsive features and general psychopathology. Behaviour Research and Therapy, 41(6), 681–700.
Coles, M. G. H., Scheffers, M. K., & Holroyd, C. B. (2001). Why is there an ERN/Ne on correct trials? Response representations, stimulus-related components, and the theory of error-processing? Biological Psychology, 56(3), 173–189.
Debener, S., Ullsperger, M., Siegel, M., Fiehler, K., von Cramon, D. Y., & Engel, A. K. (2005). Trial-by-trial coupling of concurrent electroencephalogram and functional magnetic resonance imaging identifies the dynamics of performance monitoring. Journal of Neuroscience, 25(50), 11730–11737.
Dien, J. (2010a). The ERP PCA Toolkit: An open source program for advanced statistical analysis of event-related potential data. Journal of Neuroscience Methods, 187(1), 138–145.
Dien, J. (2010b). Evaluating two-step PCA of ERP data with Geomin, Infomax, Oblimin, Promax, and Varimax rotations. Psychophysiology, 47(1), 170–183.
Dien, J., Beal, D. J., & Berg, P. (2005). Optimizing principal components analysis of event-related potentials: matrix type, factor loading weighting, extraction, and rotations. Clinical Neurophysiology, 116(8), 1808–1825.
Dien, J., Michelson, C. A., & Franklin, M. S. (2010). Separating the visual sentence N400 effect from the P400 sequential expectancy effect: Cognitive and neuroanatomical implications. Brain Research, 1355, 126–140.
Endrass, T., Franke, C., & Kathmann, N. (2005). Error awareness in a saccade countermanding task. Journal of Psychophysiology, 19(4), 275–280. doi:10.1027/0269-8803.19.4.275
Endrass, T., Klawohn, J., Gruetzmann, R., Ischebeck, M., & Kathmann, N. (2012). Response-related negativities following correct and incorrect responses: Evidence from a temporospatial principal component analysis. Psychophysiology, 49(6), 733–743. doi:10.1111/j.1469-8986.2012.01365.x
Endrass, T., Klawohn, J., Preuss, J., & Kathmann, N. (2012). Temporospatial dissociation of Pe subcomponents for perceived and unperceived errors. Frontiers in Human Neuroscience, 6, 178. doi:10.3389/Fnhum.2012.00178
Endrass, T., Klawohn, J., Schuster, F., & Kathmann, N. (2008). Overactive performance monitoring in obsessive-compulsive disorder: ERP evidence from correct and erroneous reactions. Neuropsychologia, 46(7), 1877–1887.
Endrass, T., Reuter, B., & Kathmann, N. (2007). ERP correlates of conscious error recognition: aware and unaware errors in an antisaccade task. European Journal of Neuroscience, 26(6), 1714–1720. doi:10.1111/j.1460-9568.2007.05785.x
Endrass, T., Schuermann, B., Kaufmann, C., Spielberg, R., Kniesche, R., & Kathmann, N. (2010). Performance monitoring and error significance in patients with obsessive-compulsive disorder. Biological Psychology, 84(2), 257–263. doi:10.1016/j.biopsycho.2010.02.002
Eriksen, B., & Eriksen, C. B. (1974). Effect of noise letters upon the identification of a target letter in a nonsearch task. Perception and Psychophysics, 16, 143–169.
Falkenstein, M., Hohnsbein, J., Hoormann, J., & Blanke, L. (1990). Effects of errors in choice reaction tasks on the ERP under focused and divided attention. In C. H. M. Brunia, A. W. K. Gaillard, & A. Kok (Eds.), Psychophysiological Brain Research (1st ed., pp. 192–195). Tilburg: Tilburg University Press.
Falkenstein, M., Hohnsbein, J., Hoormann, J., & Blanke, L. (1991). Effects of crossmodal divided attention on late ERP components: II. Error processing in choice reaction tasks. Electroencephalography & Clinical Neurophysiology, 78(6), 447–455.
Falkenstein, M., Hoormann, J., Christ, S., & Hohnsbein, J. (2000). ERP components on reaction errors and their functional significance: A tutorial. Biological Psychology, 51(2–3), 87–107.
Fitzgerald, K. D., Welsh, R. C., Gehring, W. J., Abelson, J. L., Himle, J. A., Liberzon, I., & Taylor, S. F. (2005). Error-related hyperactivity of the anterior cingulate cortex in obsessive-compulsive disorder. Biological Psychiatry, 57(3), 287–294.
Foa, E. B., Huppert, J. D., Leiberg, S., Langner, R., Kichic, R., Hajcak, G., & Salkovskis, P. M. (2002). The Obsessive-Compulsive Inventory: Development and validation of a short version. Psychological Assessment, 14(4), 485–496.
Ford, J. M. (1999). Schizophrenia: The broken P300 and beyond. Psychophysiology, 36, 667–682.
Foti, D., Hajcak, G., & Dien, J. (2009). Differentiating neural responses to emotional pictures: Evidence from temporal-spatial PCA. Psychophysiology, 46(3), 521–530.
Foti, D., Weinberg, A., Dien, J., & Hajcak, G. (2011). Event-Related potential activity in the basal ganglia differentiates rewards from nonrewards: Temporospatial principal components analysis and source localization of the feedback negativity. Human Brain Mapping, 32(12), 2207–2216. doi:10.1002/Hbm.21182
Gehring, W. J., Goss, B., Coles, G. H., Meyer, D. E., & Donchin, E. (1993). A neural system for error detection and compensation. Psychological Science, 4(6), 387–390.
Gehring, W. J., Himle, J., & Nisenson, L. G. (2000). Action-monitoring dysfunction in obsessive-compulsive disorder. Psychological Science, 11(1), 1–6.
Ghisi, M., Chiri, L. R., Marchetti, I., Sanavio, E., & Sica, C. (2010). In search of specificity: “Not just right experiences” and obsessive-compulsive symptoms in non-clinical and clinical Italian individuals. Journal of Anxiety Disorders, 24(8), 879–886. doi:10.1016/j.janxdis.2010.06.011
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L., … Charney, D. S. (1989). The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry, 46(11), 1006–1011.
Grundler, T. O. J., Cavanagh, J. F., Figueroa, C. M., Frank, M. J., & Allen, J. J. B. (2009). Task-related dissociation in ERN amplitude as a function of obsessive-compulsive symptoms. Neuropsychologia, 47(8–9), 1978–1987.
Hajcak, G., Franklin, M. E., Foa, E. B., & Simons, R. F. (2008). Increased error-related brain activity in pediatric obsessive-compulsive disorder before and after treatment. American Journal of Psychiatry, 165(1), 116–123.
Hajcak, G., McDonald, N., & Simons, R. F. (2004). Error-related psychophysiology and negative affect. Brain and Cognition, 56(2), 189–197.
Hajcak, G., & Simons, R. F. (2002). Error-related brain activity in obsessive-compulsive undergraduates. Psychiatry Research, 110(1), 63–72.
Hoffmann, S., & Falkenstein, M. (2010). Independent component analysis of erroneous and correct responses suggests online response control. Human Brain Mapping, 31(9), 1305–1315. doi:10.1002/Hbm.20937
Johannes, S., Wieringa, B.M., Nager, W., Rada, D., Dengler, R., Emrich, H.M., …, Dietrich, D.E. (2001). Discrepant target detection and action monitoring in obsessive-compulsive disorder. Psychiatry Research: Neuroimaging Section, 108, 101–110.
Kayser, J., & Tenke, C. E. (2003). Optimizing PCA methodology for ERP component identification and measurement: theoretical rationale and empirical evaluation. Clinical Neurophysiology, 114(12), 2307–2325. doi:10.1016/S1388-2457(03)00241-4
Kayser, J., & Tenke, C. E. (2005). Trusting in or breaking with convention: Towards a renaissance of principal components analysis in electrophysiology. Clinical Neurophysiology, 116(8), 1747–1753.
Kopp, B., Rist, F., & Mattler, U. (1996). N200 in the flanker task as a neurobehavioral tool for investigating executive control. Psychophysiology, 33(3), 282–294.
Kuhn, S., Kaufmann, C., Simon, D., Endrass, T., Gallinat, J., & Kathmann, N. (2013). Reduced thickness of anterior cingulate cortex in obsessive-compulsive disorder. Cortex, 49(8), 2178–2185. doi:10.1016/j.cortex.2012.09.001
Larson, M. J., Fair, J. E., Good, D. A., & Baldwin, S. A. (2010). Empathy and error processing. Psychophysiology, 47(3), 415–424. doi:10.1111/j.1469-8986.2009.00949.x
Maltby, N., Tolin, D. F., Worhunsky, P., O’Keefe, T. M., & Kiehl, K. A. (2005). Dysfunctional action monitoring hyperactivates frontal-striatal circuits in obsessive-compulsive disorder: An event-related fMRI study. NeuroImage, 24(2), 495–503.
Menzies, L., Chamberlain, S. R., Laird, A. R., Thelen, S. M., Sahakian, B. J., & Bullmore, E. T. (2008). Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: The orbitofronto-striatal model revisited. Neuroscience and Biobehavioral Reviews, 32(3), 525–549. doi:10.1016/j.neubiorev.2007.09.005
O’Connell, R. G., Dockree, P. M., Bellgrove, M. A., Kelly, S. P., Hester, R., Garavan, H., … Foxe, J. J. (2007). The role of cingulate cortex in the detection of errors with and without awareness: a high-density electrical mapping study. European Journal of Neuroscience, 25(8), 2571–2579. doi: 10.1111/j.1460-9568.2007.05477.x
Olvet, D. M., & Hajcak, G. (2008). The error-related negativity (ERN) and psychopathology: Toward an endophenotype. Clinical Psychology Review, 28(8), 1343–1354. doi:10.1016/j.cpr.2008.07.003
Overbeek, T. J. M., Nieuwenhuis, S., & Ridderinkhof, K. R. (2005). Dissociable components of error processing: On the functional significance of the Pe vis-a-vis the ERN/Ne. Journal of Psychophysiology, 19(4), 319–329.
Pitman, R. K. (1987). A cybernetic model of obsessive-compulsive psychopathology. Comprehensive Psychiatry, 28(4), 334–343.
Riesel, A., Endrass, T., Kaufmann, C., & Kathmann, N. (2011). Overactive error-related brain activity as a candidate endophenotype for obsessive-compulsive disorder: Evidence from unaffected first-degree relatives. American Journal of Psychiatry, 168(3), 317–324. doi:10.1176/appi.ajp.2010.10030416
Roger, C., Benar, C. G., Vidal, F., Hasbroucq, T., & Burle, B. (2010). Rostral Cingulate Zone and correct response monitoring: ICA and source localization evidences for the unicity of correct- and error-negativities. NeuroImage, 51(1), 391–403. doi:10.1016/j.neuroimage.2010.02.005
Ruchsow, M., Gron, G., Reuter, K., Spitzer, M., Hermle, L., & Kiefer, M. (2005). Error-related brain activity in patients with obsessive-compulsive disorder and in healthy controls. Journal of Psychophysiology, 19(4), 298–304.
Rushworth, M. F. S., Buckley, M. J., Behrens, T. E. J., Walton, M. E., & Bannerman, D. M. (2007). Functional organization of the medial frontal cortex. Current Opinion in Neurobiology, 17(2), 220–227. doi:10.1016/j.conb.2007.03.001
Santesso, D. L., Segalowitz, S. J., & Schmidt, L. A. (2006). Error-related electrocortical responses are enhanced in children with obsessive-compulsive behaviors. Developmental Neuropsychology, 29(3), 431–445. doi:10.1207/s15326942dn2903_3
Schmidt, K. H., & Metzler, P. (1992). Wortschatztest (WST). Weinheim: Beltz.
Steer, R. A., Ball, R., Ranieri, W. F., & Beck, A. T. (1997). Further evidence for the construct validity of the Beck Depression Inventory-II with psychiatric outpatients. Psychological Reports, 80(2), 443–446.
Stern, E. R., Liu, Y. N., Gehring, W. J., Lister, J. J., Yin, G., Zhang, J., … Taylor, S. F. (2010). Chronic medication does not affect hyperactive error responses in obsessive-compulsive disorder. Psychophysiology, 47(5), 913–920. doi: 10.1111/j.1469-8986.2010.00988.x
Stern, E. R., Welsh, R. C., Fitzgerald, K. D., Gehring, W. J., Lister, J. J., Himle, J. A., … Taylor, S. F. (2011). Hyperactive error responses and altered connectivity in ventromedial and frontoinsular cortices in obsessive-compulsive disorder. Biological Psychiatry, 69(6), 583–591. doi: 10.1016/j.biopsych.2010.09.048
Stern, E. R., Welsh, R. C., Gonzalez, R., Fitzgerald, K. D., Abelson, J. L., & Taylor, S. F. (2012). Subjective uncertainty and limbic hyperactivation in obsessive-compulsive disorder. Human Brain Mapping. doi:10.1002/hbm.22038
Ursu, S., Stenger, V. A., Shear, M. K., Jones, M. R., & Carter, C. S. (2003). Overactive action monitoring in obsessive-compulsive disorder: Evidence from functional magnetic resonance imaging. Psychological Science, 14(4), 347–353.
Van Veen, V., & Carter, C. S. (2002). The timing of action-monitoring processes in the anterior cingulate cortex. Journal of Cognitive Neuroscience, 14(4), 593–602. doi:10.1162/08989290260045837
Vidal, F., Burle, B., Bonnet, M., Grapperon, J., & Hasbroucq, T. (2003). Error negativity on correct trials: A reexamination of available data. Biological Psychology, 64(3), 265–282.
Vidal, F., Hasbroucq, T., Grapperon, J., & Bonnet, M. (2000). Is the “error negativity” specific to errors? Biological Psychology, 51(2–3), 109–128.
Vocat, R., Pourtois, G., & Vuilleumier, P. (2008). Unavoidable errors: A spatio-temporal analysis of time-course and neural sources of evoked potentials associated with error processing in a speeded task. Neuropsychologia, 46(10), 2545–2555. doi:10.1016/j.neuropsychologia.2008.04.006
Weinberg, A., Klein, D. N., & Hajcak, G. (2012). Increased error-related brain activity distinguishes generalized anxiety disorder with and without comorbid major depressive disorder. Journal of Abnormal Psychology, 121(4), 885–896. doi:10.1037/a0028270
Weinberg, A., Olvet, D. M., & Hajcak, G. (2010). Increased error-related brain activity in generalized anxiety disorder. Biological Psychology, 85(3), 472–480. doi:10.1016/j.biopsycho.2010.09.011
Wittchen, H. U., Zaudig, M., & Fydrich, T. (1997). Strukturiertes Klinisches Interview für DSM-IV. Göttingen: Hogrefe.
Xiao, Z. P., Wang, J. J., Zhang, M., Li, H., Tang, Y. Y., Wang, Y. A., … Fromson, J. A. (2011). Error-related negativity abnormalities in generalized anxiety disorder and obsessive-compulsive disorder. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 35(1), 265–272. doi: 10.1016/j.pnpbp.2010.11.022
Yordanova, J., Falkenstein, M., Hohnsbein, J., & Kolev, V. (2004). Parallel systems of error processing in the brain. NeuroImage, 22(2), 590–602.
Acknowledgments
This work was supported by the German Research Foundation (DFG; EN 906/1-1).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Klawohn, J., Riesel, A., Grützmann, R. et al. Performance monitoring in obsessive–compulsive disorder: A temporo-spatial principal component analysis. Cogn Affect Behav Neurosci 14, 983–995 (2014). https://doi.org/10.3758/s13415-014-0248-0
Published:
Issue Date:
DOI: https://doi.org/10.3758/s13415-014-0248-0