Abstract
Matrix-assisted laser desorption/ionisation mass spectrometry imaging (MALDI-MSI) is a common molecular imaging modality used to characterise the abundance and spatial distribution of lipids in situ. There are several technical challenges predominantly involving sample pre-treatment and preparation which have complicated the analysis of clinical tissues by MALDI-MSI. Firstly, the common embedding of samples in optimal cutting temperature (O.C.T.), which contains high concentrations of polyethylene glycol (PEG) polymers, causes analyte signal suppression during mass spectrometry (MS) by competing for available ions during ionisation. This suppressive effect has constrained the application of MALDI-MSI for the molecular mapping of clinical tissues. Secondly, the complexity of the mass spectra is obtained by the formation of multiple adduct ions. The process of analyte ion formation during MALDI can generate multiple m/z peaks from a single lipid species due to the presence of alkali salts in tissues, resulting in the suppression of protonated adduct formation and the generation of multiple near isobaric ions which produce overlapping spatial distributions. Presented is a method to simultaneously remove O.C.T. and endogenous salts. This approach was applied to lipid imaging in order to prevent analyte suppression, simplify data interpretation, and improve sensitivity by promoting lipid protonation and reducing the formation of alkali adducts.
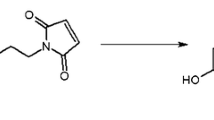
Graphical abstract







Similar content being viewed by others
Data availability
Available on request
References
Angel PM, Norris-Caneda K, Drake RR. In situ imaging of tryptic peptides by MALDI imaging mass spectrometry using fresh-frozen or formalin-fixed, paraffin-embedded tissue. Curr Protoc Protein Sci. 2018;94(1):e65. https://doi.org/10.1002/cpps.65.
Beine B, Diehl HC, Meyer HE, Henkel C. Tissue MALDI mass spectrometry imaging (MALDI MSI) of peptides. Methods Mol Biol (Clifton, NJ). 2016;1394:129–50. https://doi.org/10.1007/978-1-4939-3341-9_10.
Chatterji B, Dickhut C, Mielke S, Kruger J, Just I, Glage S, et al. MALDI imaging mass spectrometry to investigate endogenous peptides in an animal model of Usher’s disease. Proteomics. 2014;14(13–14):1674–87. https://doi.org/10.1002/pmic.201300558.
Mutuku SM, Trim PJ, Prabhala BK, Irani S, Bremert KL, Logan JM, et al. Evaluation of small molecule drug uptake in patient-derived prostate cancer explants by mass spectrometry. Sci Rep. 2019;9(1):15008. https://doi.org/10.1038/s41598-019-51549-3.
Ntshangase S, Mdanda S, Singh SD, Naicker T, Kruger HG, Baijnath S, et al. Mass spectrometry imaging demonstrates the regional brain distribution patterns of three first-line antiretroviral drugs. ACS Omega. 2019;4(25):21169–77. https://doi.org/10.1021/acsomega.9b02582.
Schulz S, Becker M, Groseclose MR, Schadt S, Hopf C. Advanced MALDI mass spectrometry imaging in pharmaceutical research and drug development. Curr Opin Biotechnol. 2019;55:51–9. https://doi.org/10.1016/j.copbio.2018.08.003.
Berry KA, Li B, Reynolds SD, Barkley RM, Gijon MA, Hankin JA, et al. MALDI imaging MS of phospholipids in the mouse lung. J Lipid Res. 2011;52(8):1551–60. https://doi.org/10.1194/jlr.M015750.
Gode D, Volmer DA. Lipid imaging by mass spectrometry - a review. Analyst. 2013;138(5):1289–315. https://doi.org/10.1039/c2an36337b.
Goto T, Terada N, Inoue T, Nakayama K, Okada Y, Yoshikawa T, et al. The expression profile of phosphatidylinositol in high spatial resolution imaging mass spectrometry as a potential biomarker for prostate cancer. PLoS One. 2014;9(2):e90242. https://doi.org/10.1371/journal.pone.0090242.
Meisenbichler C, Doppler C, Bernhard D, Muller T. Improved matrix coating for positive- and negative-ion-mode MALDI-TOF imaging of lipids in blood vessel tissues. Anal Bioanal Chem. 2019;411(15):3221–7. https://doi.org/10.1007/s00216-019-01826-x.
Randall EC, Zadra G, Chetta P, Lopez BGC, Syamala S, Basu SS, et al. Molecular characterization of prostate cancer with associated Gleason score using mass spectrometry imaging. Mol Cancer Res. 2019;17(5):1155–65. https://doi.org/10.1158/1541-7786.Mcr-18-1057.
Nakashima Y, Setou M. Distribution of antisense oligonucleotides in rat eyeballs using MALDI imaging mass spectrometry. Mass Spectrom (Tokyo). 2018;7(1):A0070. https://doi.org/10.5702/massspectrometry.A0070.
Yokoi H, Kasahara Y, Obika S, Doi T, Kamada H. Development of a detection method for antisense oligonucleotides in mouse kidneys by matrix-assisted laser desorption/ionization imaging mass spectrometry. Rapid Commun Mass Spectrom. 2018;32(23):1984–90. https://doi.org/10.1002/rcm.8274.
Ucal Y, Durer ZA, Atak H, Kadioglu E, Sahin B, Coskun A, et al. Clinical applications of MALDI imaging technologies in cancer and neurodegenerative diseases. Biochim Biophys Acta, Proteins Proteomics. 2017;1865(7):795–816. https://doi.org/10.1016/j.bbapap.2017.01.005.
Blanc L, Lenaerts A, Dartois V, Prideaux B. Visualization of mycobacterial biomarkers and tuberculosis drugs in infected tissue by MALDI-MS imaging. Anal Chem. 2018;90(10):6275–82. https://doi.org/10.1021/acs.analchem.8b00985.
Kadesch P, Quack T, Gerbig S, Grevelding CG, Spengler B. Lipid topography in Schistosoma mansoni cryosections, revealed by microembedding and high-resolution atmospheric-pressure matrix-assisted laser desorption/ionization (MALDI) mass spectrometry imaging. Anal Chem. 2019;91(7):4520–8. https://doi.org/10.1021/acs.analchem.8b05440.
Santos T, Theron L, Chambon C, Viala D, Centeno D, Esbelin J, et al. MALDI mass spectrometry imaging and in situ microproteomics of Listeria monocytogenes biofilms. J Proteome. 2018;187:152–60. https://doi.org/10.1016/j.jprot.2018.07.012.
Kurreck A, Vandergrift LA, Fuss TL, Habbel P, Agar NYR, Cheng LL. Prostate cancer diagnosis and characterization with mass spectrometry imaging. Prostate Cancer Prostatic Dis. 2018;21(3):297–305. https://doi.org/10.1038/s41391-017-0011-z.
Veloso A, Fernandez R, Astigarraga E, Barreda-Gomez G, Manuel I, Giralt MT, et al. Distribution of lipids in human brain. Anal Bioanal Chem. 2011;401(1):89–101. https://doi.org/10.1007/s00216-011-4882-x.
Mallah K, Quanico J, Trede D, Kobeissy F, Zibara K, Salzet M, et al. Lipid changes associated with traumatic brain injury revealed by 3D MALDI-MSI. Anal Chem. 2018;90(17):10568–76. https://doi.org/10.1021/acs.analchem.8b02682.
Flinders B, Huizing LRS, van Heerden M, Cuyckens F, Neumann UP, van der Laan LJW, et al. Cross-species molecular imaging of bile salts and lipids in liver: identification of molecular structural markers in health and disease. Anal Chem. 2018;90(20):11835–46. https://doi.org/10.1021/acs.analchem.8b01378.
Goto T, Terada N, Inoue T, Kobayashi T, Nakayama K, Okada Y, et al. Decreased expression of lysophosphatidylcholine (16:0/OH) in high resolution imaging mass spectrometry independently predicts biochemical recurrence after surgical treatment for prostate cancer. Prostate. 2015;75(16):1821–30. https://doi.org/10.1002/pros.23088.
Schwamborn K. Imaging mass spectrometry in biomarker discovery and validation. J Proteome. 2012;75(16):4990–8. https://doi.org/10.1016/j.jprot.2012.06.015.
Longuespee R, Alberts D, Pottier C, Smargiasso N, Mazzucchelli G, Baiwir D, et al. A laser microdissection-based workflow for FFPE tissue microproteomics: important considerations for small sample processing. Methods. 2016;104:154–62. https://doi.org/10.1016/j.ymeth.2015.12.008.
Goto-Inoue N, Hayasaka T, Zaima N, Setou M. Imaging mass spectrometry for lipidomics. Biochim Biophys Acta. 2011;1811(11):961–9. https://doi.org/10.1016/j.bbalip.2011.03.004.
Mounfield WP 3rd, Garrett TJ. Automated MALDI matrix coating system for multiple tissue samples for imaging mass spectrometry. J Am Soc Mass Spectrom. 2012;23(3):563–9. https://doi.org/10.1007/s13361-011-0324-4.
Angel PM, Spraggins JM, Baldwin HS, Caprioli R. Enhanced sensitivity for high spatial resolution lipid analysis by negative ion mode matrix assisted laser desorption ionization imaging mass spectrometry. Anal Chem. 2012;84(3):1557–64. https://doi.org/10.1021/ac202383m.
Wang HY, Liu CB, Wu HW. A simple desalting method for direct MALDI mass spectrometry profiling of tissue lipids. J Lipid Res. 2011;52(4):840–9. https://doi.org/10.1194/jlr.D013060.
Schwartz SA, Reyzer ML, Caprioli RM. Direct tissue analysis using matrix-assisted laser desorption/ionization mass spectrometry: practical aspects of sample preparation. J Mass Spectrom. 2003;38(7):699–708. https://doi.org/10.1002/jms.505.
Weston LA, Hummon AB. Comparative LC-MS/MS analysis of optimal cutting temperature (OCT) compound removal for the study of mammalian proteomes. Analyst. 2013;138(21):6380–4. https://doi.org/10.1039/c3an01121f.
Bhandari DR, Shen T, Rompp A, Zorn H, Spengler B. Analysis of cyathane-type diterpenoids from Cyathus striatus and Hericium erinaceus by high-resolution MALDI MS imaging. Anal Bioanal Chem. 2014;406(3):695–704. https://doi.org/10.1007/s00216-013-7496-7.
Enthaler B, Pruns JK, Wessel S, Rapp C, Fischer M, Wittern KP. Improved sample preparation for MALDI-MSI of endogenous compounds in skin tissue sections and mapping of exogenous active compounds subsequent to ex-vivo skin penetration. Anal Bioanal Chem. 2012;402(3):1159–67. https://doi.org/10.1007/s00216-011-5562-6.
Strohalm M, Strohalm J, Kaftan F, Krasny L, Volny M, Novak P, et al. Poly[N-(2-hydroxypropyl)methacrylamide]-based tissue-embedding medium compatible with MALDI mass spectrometry imaging experiments. Anal Chem. 2011;83(13):5458–62. https://doi.org/10.1021/ac2011679.
Andersen MK, Krossa S, Høiem TS, Buchholz R, Claes BSR, Balluff B, et al. Simultaneous detection of zinc and its pathway metabolites using MALDI MS imaging of prostate tissue. Anal Chem. 2020;92(4):3171–9. https://doi.org/10.1021/acs.analchem.9b04903.
Gill EL, Yost RA, Vedam-Mai V, Garrett TJ. Precast gelatin-based molds for tissue embedding compatible with mass spectrometry imaging. Anal Chem. 2017;89(1):576–80. https://doi.org/10.1021/acs.analchem.6b04185.
Rohrbach TD, Boyd AE, Grizzard PJ, Spiegel S, Allegood J, Lima S. A simple method for sphingolipid analysis of tissues embedded in optimal cutting temperature compound. J Lipid Res. 2020;61(6):953–67. https://doi.org/10.1194/jlr.D120000809.
Shah P, Zhang B, Choi C, Yang S, Zhou J, Harlan R, et al. Tissue proteomics using chemical immobilization and mass spectrometry. Anal Biochem. 2015;469:27–33. https://doi.org/10.1016/j.ab.2014.09.017.
Tian Y, Bova GS, Zhang H. Quantitative glycoproteomic analysis of optimal cutting temperature-embedded frozen tissues identifying glycoproteins associated with aggressive prostate cancer. Anal Chem. 2011;83(18):7013–9. https://doi.org/10.1021/ac200815q.
Zhang W, Sakashita S, Taylor P, Tsao MS, Moran MF. Comprehensive proteome analysis of fresh frozen and optimal cutting temperature (OCT) embedded primary non-small cell lung carcinoma by LC-MS/MS. Methods. 2015;81:50–5. https://doi.org/10.1016/j.ymeth.2015.02.008.
Nassar ZD, Mah CY, Dehairs J, Burvenich IJ, Irani S, Centenera MM, et al. Human DECR1 is an androgen-repressed survival factor that regulates PUFA oxidation to protect prostate tumor cells from ferroptosis. Elife. 2020;9. https://doi.org/10.7554/eLife.54166.
Morikawa-Ichinose T, Fujimura Y, Murayama F, Yamazaki Y, Yamamoto T, Wariishi H, et al. Improvement of sensitivity and reproducibility for imaging of endogenous metabolites by matrix-assisted laser desorption/ionization-mass spectrometry. J Am Soc Mass Spectrom. 2019;30(8):1512–20. https://doi.org/10.1007/s13361-019-02221-7.
Wang C, Wang M, Han X. Applications of mass spectrometry for cellular lipid analysis. Mol BioSyst. 2015;11(3):698–713. https://doi.org/10.1039/c4mb00586d.
Erb WJ, Hanton SD, Owens KG. A study of gas-phase cationization in matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. Rapid Commun Mass Spectrom. 2006;20(14):2165–9. https://doi.org/10.1002/rcm.2568.
Zhang J, Zenobi R. Matrix-dependent cationization in MALDI mass spectrometry. J Mass Spectrom. 2004;39(7):808–16. https://doi.org/10.1002/jms.657.
Moskovets E, Karger BL. Mass calibration of a matrix-assisted laser desorption/ionization time-of-flight mass spectrometer including the rise time of the delayed extraction pulse. Rapid Commun Mass Spectrom. 2003;17(3):229–37. https://doi.org/10.1002/rcm.898.
Jorge S, Capelo JL, LaFramboise W, Dhir R, Lodeiro C, Santos HM. Development of a robust ultrasonic-based sample treatment to unravel the proteome of OCT-embedded solid tumor biopsies. J Proteome Res. 2019;18(7):2979–86. https://doi.org/10.1021/acs.jproteome.9b00248.
Zaima N, Yoshioka S, Sato Y, Shinano S, Ikeda Y, Moriyama T. Enhanced specificity for phosphatidylcholine analysis by positive ion mode matrix-assisted laser desorption/ionization imaging mass spectrometry. Rapid Commun Mass Spectrom. 2014;28(13):1453–8. https://doi.org/10.1002/rcm.6917.
Wang HY, Wu HW, Tsai PJ, Liu CB. MALDI-mass spectrometry imaging of desalted rat brain sections reveals ischemia-mediated changes of lipids. Anal Bioanal Chem. 2012;404(1):113–24. https://doi.org/10.1007/s00216-012-6077-5.
de Macedo CS, Anderson DM, Pascarelli BM, Spraggins JM, Sarno EN, Schey KL, et al. MALDI imaging reveals lipid changes in the skin of leprosy patients before and after multidrug therapy (MDT). J Mass Spectrom. 2015;50(12):1374–85. https://doi.org/10.1002/jms.3708.
de Macedo CS, Anderson DM, Schey KL. MALDI (matrix assisted laser desorption ionization) imaging mass spectrometry (IMS) of skin: aspects of sample preparation. Talanta. 2017;174:325–35. https://doi.org/10.1016/j.talanta.2017.06.018.
Leopold J, Popkova Y, Engel KM, Schiller J. Visualizing phosphatidylcholine via mass spectrometry imaging: relevance to human health. Expert Rev Proteomics. 2018;15(10):791–800. https://doi.org/10.1080/14789450.2018.1526679.
Buchberger AR, DeLaney K, Johnson J, Li L. Mass spectrometry imaging: a review of emerging advancements and future insights. Anal Chem. 2018;90(1):240–65. https://doi.org/10.1021/acs.analchem.7b04733.
Barrett T, Riemer F, McLean MA, Kaggie J, Robb F, Tropp JS, et al. Quantification of total and intracellular sodium concentration in primary prostate cancer and adjacent normal prostate tissue with magnetic resonance imaging. Investig Radiol. 2018;53(8):450–6. https://doi.org/10.1097/rli.0000000000000470.
Broeke NC, Peterson J, Lee J, Martin PR, Farag A, Gomez JA, et al. Characterization of clinical human prostate cancer lesions using 3.0-T sodium MRI registered to Gleason-graded whole-mount histopathology. J Magn Reson Imaging. 2019;49(5):1409–19. https://doi.org/10.1002/jmri.26336.
Wang HY, Liu CB, Wu HW, Kuo JS. Direct profiling of phospholipids and lysophospholipids in rat brain sections after ischemic stroke. Rapid Commun Mass Spectrom. 2010;24(14):2057–64. https://doi.org/10.1002/rcm.4620.
Zhao X, Huffman KE, Fujimoto J, Canales JR, Girard L, Nie G, et al. Quantitative proteomic analysis of optimal cutting temperature (OCT) embedded core-needle biopsy of lung cancer. J Am Soc Mass Spectrom. 2017;28(10):2078–89. https://doi.org/10.1007/s13361-017-1706-z.
Seeley EH, Oppenheimer SR, Mi D, Chaurand P, Caprioli RM. Enhancement of protein sensitivity for MALDI imaging mass spectrometry after chemical treatment of tissue sections. J Am Soc Mass Spectrom. 2008;19(8):1069–77. https://doi.org/10.1016/j.jasms.2008.03.016.
Cerruti CD, Touboul D, Guérineau V, Petit VW, Laprévote O, Brunelle A. MALDI imaging mass spectrometry of lipids by adding lithium salts to the matrix solution. Anal Bioanal Chem. 2011;401(1):75–87. https://doi.org/10.1007/s00216-011-4814-9.
Dufresne M, Patterson NH, Norris JL, Caprioli RM. Combining salt doping and matrix sublimation for high spatial resolution MALDI imaging mass spectrometry of neutral lipids. Anal Chem. 2019;91(20):12928–34. https://doi.org/10.1021/acs.analchem.9b02974.
Funding
Funding for this study was provided by the Movember Foundation/Prostate Cancer Foundation of Australia (MRTA3) and the US Department of Defense Congressionally Directed Medical Research Program grant (ID W81XWH1910566). The mass spectrometer used in this research is located in the Australian Cancer Research Foundation (ACRF) Centre for Integrated Cancer Systems Biology at SAHMRI which was funded by the ACRF. J.X.M. Truong and J. White are supported by a Postgraduate Scholarship from the University of Adelaide; L.M. Butler is supported by a Principal Cancer Research Fellowship awarded by Cancer Council’s Beat Cancer project on behalf of its donors, the State Government through the Department of Health and the Australian Government through the Medical Research Future Fund.
Author information
Authors and Affiliations
Contributions
All authors were involved in the conceptualisation of this research. Funding through the prescribed bodies was acquired by L.M. Butler. The methodology involved in this study was established by P.J. Trim, J.X.M. Truong, X. Spotbeen, and M.F. Snel. Data analysis, collection, and interpretation were performed by J.X.M. Truong, P.J. Trim, J. White, and MFS. Resources were provided by M.F. Snel, P.J. Trim, and L.M. Butler. Drafting and editing were completed by J.X.M. Truong, P.J. Trim, M.F. Snel, and L.M. Butler. All authors contributed to the final review and edit of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval
Approval for the use of human prostate cancer tissues was granted by the Ethics Committees of the University of Adelaide (Adelaide, Australia) (approval number H-2018-222) and St Andrew’s Hospital (Adelaide Australia). The use of prostate xenograft tissues was approved by the Animal Ethics Committee of the University of Adelaide (Adelaide, Australia) (approval number M-2019-037).
Source of biological material
Human prostate cancer tissues were obtained from patients undergoing radical prostatectomies and were provided by the Australian Prostate Cancer BioResource (Adelaide Australia). Prostate xenograft tissues were obtained from another study conducted by the University of Adelaide [40].
Statement of animal welfare
N/A
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Additional information
Published in the topical collection Mass Spectrometry Imaging 2.0 with guest editors Shane R. Ellis and Tiffany Porta Siegel.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 3453 kb)
Rights and permissions
About this article
Cite this article
Truong, J.X.M., Spotbeen, X., White, J. et al. Removal of optimal cutting temperature (O.C.T.) compound from embedded tissue for MALDI imaging of lipids. Anal Bioanal Chem 413, 2695–2708 (2021). https://doi.org/10.1007/s00216-020-03128-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-020-03128-z