Abstract
Purpose
To assess the technical feasibility and outcomes of adrenal metastases cryoablation.
Materials and methods
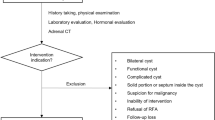
This is an IRB approved retrospective review of adrenal metastases cryoablation between April 2003 and October 2018. Forty percutaneous cryoablation procedures were performed on 40 adrenal metastases in 34 patients. Histology, tumor size, ablation zone size, major vessel proximity, local recurrences, complications, and anesthesia-managed hypertension monitoring was collected. Complications were graded according to the Common Terminology of Complications and Adverse Events (CTCAE).
Results
Mean tumor and ablation size was 3.2 cm and 5.2 cm, respectively. Local recurrence rate was 10.0% (N = 4/40) for a mean follow-up time of 1.8 years. Recurrences for tumors > 3 cm (21.0%, N = 4/19) was greater than for tumors ≤ 3 cm (0.0%, N = 0/21) (p = 0.027). Proximity of major vasculature (i.e., IVC & aorta) did not statistically effect recurrence rates (p = 0.52), however, those that recurred near vasculature were > 4 cm. Major complication (≥ grade 3) rate was 5.0% (N = 2/40), with one major complication attributable to the procedure. Immediate escalation of blood pressure during the passive stick phase (between freeze cycles) or post procedure thaw phase was greater in patients with residual adrenal tissue (N = 21/38) versus masses replacing the entire adrenal gland (N = 17/38), (p = 0.0020). Lower blood pressure elevation was noted in patients with residual adrenal tissue who were pre-treated with alpha blockade (p = 0.015).
Conclusions
CT-guided percutaneous cryoablation is a safe, effective and low morbidity alternative for patients with adrenal metastases. Transient hypertension is related only to residual viable adrenal tissue but can be safely managed and prophylactically treated.



Similar content being viewed by others
References
Arnold, D.T., J.B. Reed, and K. Burt, Evaluation and management of the incidental adrenal mass. Proc (Bayl Univ Med Cent), 2003. 16(1): p. 7-12 https://doi.org/10.1080/08998280.2003.11927882.
Brunt, L.M. and J.F. Moley, Adrenal incidentaloma. World J Surg, 2001. 25(7): p. 905-13 https://doi.org/10.1007/s00268-001-0029-0.
Thippeswamy, R., et al., Stage IV lung cancer: Is cure possible? Indian J Med Paediatr Oncol, 2013. 34(2): p. 121-5 https://doi.org/10.4103/0971-5851.116207.
Popper, H.H., Progression and metastasis of lung cancer. Cancer Metastasis Rev, 2016. 35(1): p. 75-91 https://doi.org/10.1007/s10555-016-9618-0.
Gryn, A., et al., Patient selection for laparoscopic excision of adrenal metastases: A multicenter cohort study. Int J Surg, 2015. 24(Pt A): p. 75-80 https://doi.org/10.1016/j.ijsu.2015.10.038.
Strong, V.E., et al., Laparoscopic adrenalectomy for isolated adrenal metastasis. Ann Surg Oncol, 2007. 14(12): p. 3392-400 https://doi.org/10.1245/s10434-007-9520-7.
Tamura, T., et al., Specific organ metastases and survival in metastatic non-small-cell lung cancer. Mol Clin Oncol, 2015. 3(1): p. 217-221 https://doi.org/10.3892/mco.2014.410.
Patel, J.K., et al., Metastatic pattern of malignant melanoma. A study of 216 autopsy cases. Am J Surg, 1978. 135(6): p. 807–10 DOI: https://doi.org/10.1016/0002-9610(78)90171-x.
Ng, L. and J.M. Libertino, Adrenocortical carcinoma: diagnosis, evaluation and treatment. J Urol, 2003. 169(1): p. 5-11 https://doi.org/10.1097/01.ju.0000030148.59051.35.
Allolio, B. and M. Fassnacht, Clinical review: Adrenocortical carcinoma: clinical update. J Clin Endocrinol Metab, 2006. 91(6): p. 2027-37 https://doi.org/10.1210/jc.2005-2639.
Elder, E.E., G. Elder, and C. Larsson, Pheochromocytoma and functional paraganglioma syndrome: no longer the 10% tumor. J Surg Oncol, 2005. 89(3): p. 193-201 https://doi.org/10.1002/jso.20177.
Kebebew, E., et al., Results of laparoscopic adrenalectomy for suspected and unsuspected malignant adrenal neoplasms. Arch Surg, 2002. 137(8): p. 948–51; discussion 952–3 DOI: https://doi.org/10.1001/archsurg.137.8.948.
Muth, A., et al., Prognostic factors for survival after surgery for adrenal metastasis. Eur J Surg Oncol, 2010. 36(7): p. 699-704 https://doi.org/10.1016/j.ejso.2010.04.002.
Rudra, S., et al., Stereotactic body radiation therapy for curative treatment of adrenal metastases. Technol Cancer Res Treat, 2013. 12(3): p. 217-24 https://doi.org/10.7785/tcrt.2012.500320.
Ahmed, K.A., et al., Stereotactic body radiotherapy in the treatment of adrenal metastases. Am J Clin Oncol, 2013. 36(5): p. 509-13 https://doi.org/10.1097/COC.0b013e3182569189.
Holy, R., et al., Stereotactic body radiation therapy (SBRT) for treatment of adrenal gland metastases from non-small cell lung cancer. Strahlenther Onkol, 2011. 187(4): p. 245-51 https://doi.org/10.1007/s00066-011-2192-z.
Scorsetti, M., et al., Long-term local control achieved after hypofractionated stereotactic body radiotherapy for adrenal gland metastases: a retrospective analysis of 34 patients. Acta Oncol, 2012. 51(5): p. 618-23 https://doi.org/10.3109/0284186X.2011.652738.
Frenk, N.E., et al., Local Control and Survival after Image-Guided Percutaneous Ablation of Adrenal Metastases. J Vasc Interv Radiol, 2018. 29(2): p. 276-284 https://doi.org/10.1016/j.jvir.2017.07.026.
Aoun, H.D., et al., Percutaneous Cryoablation of Renal Tumors: Is It Time for a New Paradigm Shift? J Vasc Interv Radiol, 2017. 28(10): p. 1363-1370 https://doi.org/10.1016/j.jvir.2017.07.013.
Welch, B.T., et al., Percutaneous image-guided adrenal cryoablation: procedural considerations and technical success. Radiology, 2011. 258(1): p. 301-7 https://doi.org/10.1148/radiol.10100631.
Welch, B.T., et al., A single-institution experience in image-guided thermal ablation of adrenal gland metastases. J Vasc Interv Radiol, 2014. 25(4): p. 593-8 https://doi.org/10.1016/j.jvir.2013.12.013.
Littrup, P.J., et al., CT-guided percutaneous cryotherapy of renal masses. J Vasc Interv Radiol, 2007. 18(3): p. 383-92 https://doi.org/10.1016/j.jvir.2006.12.007.
Littrup, P.J., et al., Lethal isotherms of cryoablation in a phantom study: effects of heat load, probe size, and number. J Vasc Interv Radiol, 2009. 20(10): p. 1343-51 https://doi.org/10.1016/j.jvir.2009.05.038.
Weber, S.M., et al., Perivascular and intralesional tissue necrosis after hepatic cryoablation: results in a porcine model. Surgery, 1997. 122(4): p. 742-7 https://doi.org/10.1016/s0039-6060(97)90082-9.
Park, M.H., et al., Spectrum of CT findings after radiofrequency ablation of hepatic tumors. Radiographics, 2008. 28(2): p. 379–90; discussion 390–2 https://doi.org/10.1148/rg.282075038.
Team, R.C., R: A language and environment for statistical computing. R Foundation for Statistical Computing, 2013.
Guiou, M., et al., Stereotactic body radiotherapy for adrenal metastases from lung cancer. Journal of Radiation Oncology, 2012. 1(2): p. 155-163 https://doi.org/10.1007/s13566-012-0037-8.
Casamassima, F., et al., Stereotactic radiotherapy for adrenal gland metastases: university of Florence experience. Int J Radiat Oncol Biol Phys, 2012. 82(2): p. 919-23 https://doi.org/10.1016/j.ijrobp.2010.11.060.
Wood, B.J., et al., Radiofrequency ablation of adrenal tumors and adrenocortical carcinoma metastases. Cancer, 2003. 97(3): p. 554-60 https://doi.org/10.1002/cncr.11084.
Wolf, F.J., et al., Adrenal neoplasms: Effectiveness and safety of CT-guided ablation of 23 tumors in 22 patients. Eur J Radiol, 2012. 81(8): p. 1717-23 https://doi.org/10.1016/j.ejrad.2011.04.054.
Hasegawa, T., et al., Unresectable Adrenal Metastases: Clinical Outcomes of Radiofrequency Ablation. Radiology, 2015. 277(2): p. 584-93 https://doi.org/10.1148/radiol.2015142029.
Men, M., et al., Short-Term Outcomes and Safety of Computed Tomography-Guided Percutaneous Microwave Ablation of Solitary Adrenal Metastasis from Lung Cancer: A Multi-Center Retrospective Study. Korean J Radiol, 2016. 17(6): p. 864-873 https://doi.org/10.3348/kjr.2016.17.6.864.
Zerrweck, C., et al., Renal origin and size are independent predictors of survival after surgery for adrenal metastasis. Ann Surg Oncol, 2012. 19(11): p. 3621-6 https://doi.org/10.1245/s10434-012-2464-6.
Fintelmann, F.J., et al., Catecholamine Surge during Image-Guided Ablation of Adrenal Gland Metastases: Predictors, Consequences, and Recommendations for Management. J Vasc Interv Radiol, 2016. 27(3): p. 395-402 https://doi.org/10.1016/j.jvir.2015.11.034.
Nguyen, M.C., et al., The Adrenal Gland as a Sanctuary Site of Metastases After Pembrolizumab Treatment: A Case Series. J Natl Compr Canc Netw, 2018. 16(11): p. 1279-1283 https://doi.org/10.6004/jnccn.2018.7059.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aoun, H.D., Littrup, P.J., Nahab, B. et al. Percutaneous cryoablation of adrenal metastases: technical feasibility and safety. Abdom Radiol 46, 2805–2813 (2021). https://doi.org/10.1007/s00261-020-02848-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02848-1