Abstract
Introduction
The superior surface of the anatomical neck is presented in the classification of scapular fractures as a 2-cm-long structure, which does not correspond to reality. This issue has not yet been adequately addressed in the literature. The aim of the study was to assess the variability of a notch between the upper rim of the glenoid and the coracoid base, the so-called coracoglenoid notch (CGN), and its clinical significance.
Materials and methods
The study was based on the examination of 204 dry bone specimens of adult scapulae (92 male and 112 female). We have determined quantitative criteria for the evaluation of the CGN type, measuring the offset of anatomical neck using a digital caliper. The findings were compared with 3D CT reconstructions of fractures of the scapular anatomical neck.
Results
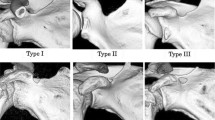
Three basic types of CGN have been identified: type A—a well-developed notch in 31%, type B—a shallow notch in 53% and type C—an absent notch in 16%. No significant difference in CGN was found between the sexes, or between the right and left sides. When compared with our six cases of the anatomical neck fracture of the scapula, two patients displayed CGN type A and type B, respectively; but in four patients, it was impossible to distinguish between types A and B.
Conclusion
The study has documented a high variability of CGN. Its presentation in the classification schemes does not correspond to anatomical reality. The presence of a deep, or shallow, notch may constitute an anatomical predisposition to a fracture of the anatomical neck.










Similar content being viewed by others
References
Anetzberger H, Putz R (1996) The scapula: principles of construction and stress. Acta Anat 156:70–80. https://doi.org/10.1159/000147830
Armitage BM, Wijdicks CA, Tarkin IS, Schroder LK, Marek DJ, Zlowodzki M, Cole PA (2009) Mapping of scapular fractures with three-dimensional computed tomography. J Bone Jt Surg Am 91-A:2222–2228. https://doi.org/10.2106/jbjs.h.00881
Arts V, Louette L (1999) Scapular neck fractures; an update of the concept of floating shoulder. Injury 30:146–148. https://doi.org/10.1016/s0020-1383(98)00231-9
Bartoníček J, Cronier P (2010) History of the treatment of scapular fractures. Arch Orthop Trauma Surg 130:83–92. https://doi.org/10.1007/s00402-009-0884-y
Bartoníček J, Tuček M, Frič V (2013) Fractures of the anatomical neck of the scapula. Two cases and review of the literature. Arch Orthop Trauma Surg 133:1115–1119. https://doi.org/10.1007/s00402-013-1783-9
Bartoníček J, Tuček M, Frič V, Obruba P (2014) Fractures of the scapular neck. Diagnosis—classifications—treatment. Int Orthop 38:2163–2173. https://doi.org/10.1007/s00264-014-2434-7
Bartoníček J, Tuček M, Klika D, Chochola A (2016) Pathoanatomy and computed tomography classification of glenoid fossa fractures based on 90 patients. Int Orthop 40:2383–2392. https://doi.org/10.1007/s00264-016-3169-4
Bartoníček J (2015) Scapular fractures. In: Court-Brown CH, Heckman AD, McQueen MM, Ricci WM, Tornetta P (eds) Rockwood and Green’s fractures in adults, 8th edn. Wolters Kluwer, Philadelphia, pp 1475–1501
Burke CS, Roberts CS, Nyland JA, Radmacher PG, Acland RD, Voor MJ (2006) Scapular thickness—implications for fracture fixation. J Shoulder Elb Surg 15:645–648. https://doi.org/10.1016/j.jse.2005.10.005
Casier SJ, Van den Broecke R, Van Houcke J, Audenaert E, De Wilde LF, Van Tongel A (2018) Morphologic variations of the scapula in 3-dimensions: a statistical shape model approach. J Shoulder Elb Surg 27:2224–2231. https://doi.org/10.1016/j.jse.2018.06.001
Decoulx P, Minet P, Lemerle (1956) Fractures de l´omoplate. Lille Chir 11:217–227
Donders JCE, Prins J, Kloen P, Streekstra GJ, Cole PA, Kleipool RP, Dobbe JGG (2020) Three-dimensional topography of scapular nutrient foramina. Surg Radiol Anat 42(8):887–892. https://doi.org/10.1007/s00276-020-02458-y
Ebraheim NA, Xu R, Haman SP, Mielder JD, Yeasting RA (2000) Quantitative anatomy of the scapula. Am J Orthop 29:287–292
Edelson JG (1992) Anatomy of the coraco-acromial arch. J Bone Jt Surg Br 74-B:589–594
Edelson JG (1996) Variations in the anatomy of the scapula with reference to the snapping scapula. Clin Orthop Relat Res 322:111–115
Euler E, Rüedi T (1996) Skapulafraktur. In: Habermeyer P, Schweiberer L (eds) Schulterchirurgie. Urban und Schwarzenberg, München, pp 261–272
Fojtík P, Kostlivý K, Bartoníček J, Naňka O (2020) The fibular notch—an anatomical study. Surg Radiol Anat. https://doi.org/10.1007/s00276-020-02476-w
Frazer JES (1946) The anatomy of the human skeleton. Churchill, London
Galina M, Santamaria E, Doro T (1998) Anthropometry of the scapula: clinical and surgical consideration. J Shoulder Elb Surg 7:284–291. https://doi.org/10.1016/s1058-2746(98)90057-x
Goss TP (1994) Fractures of the glenoid neck. J Shoulder Elb Surg 3:42–52. https://doi.org/10.1016/S1058-2746(09)80007-4
Gumina S, Postachini F, Orsina L, Cinotti G (1999) The morphometry of coracoid process—its aetiologic role in subcoracoid impingement syndrome. Int Orthop 23:198–201. https://doi.org/10.1007/s002640050349
Hardegger F, Simpson LA, Weber BG (1984) The operative treatment of scapular fractures. J Bone Jt Surg Br 66-B:725–731
Hovelacque A (1933) Ostéologie. Fascicule 1. Doin & Cie, Paris, pp 7–22
Ideberg R, Grevsten S, Larsson S (1995) Epidemiology of scapula fractures. Acta Orthop Scand 66:395–397. https://doi.org/10.3109/17453679508995571
Jaeger M, Lambert S, Südkamp NP, Kellam JF, Madsen JE, Babst R, Andermahr J, Li W, Audigé L (2013) The AO Foundation and Orthopaedic Trauma Association (AO/OTA) scapular fracture classification system: focus on glenoid fossa involvement. J Shoulder Elb Surg 22:512–520
Jeong GK, Zuckerman JD (2005) Scapula fractures. In: Zuckerman JD, Koval KJ (eds) Shoulder fractures. Thieme, New York, pp 199–222
Karelse A, Kegels L, de Wilde L (2005) The pillars of the scapula. Clin Anat 20:392–399. https://doi.org/10.1002/ca.20420
Kelly DP, Roberts ZV (2016) Case report of an isolated fracture of the anatomic neck of the scapula. Case Stud Surg 2:23–26
Li MM, Goetti P, Sandman E, Rouleau DM (2020) Influence of coracoid anatomy on the location of glenoid rim defects in anterior shoulder instability: 3D CT-scan evaluation of 51 patients. Surg Radiol Anat 42(8):895–901. https://doi.org/10.1007/s00276-020-02492-w
Mallon WJ, Brown HR, Vogler JB, Martinez S (1982) Radiographic and geometric anatomy of the scapula. Clin Orthop Relat Res 277:142–154
Neuhaus V, Bot AGJ, Guitton TG, Ring DC (2014) Scapula fractures: interobserver reliability of classification and treatment. J Orthop Trauma 28:124–129. https://doi.org/10.1097/BOT.0b013e31829673e2
Orthopaedic Trauma Association (2007) Fracture and dislocation compendium. Scapula fractures. J Orthop Trauma 21(Suppl 1):S68–S71
Orthopaedic Trauma Association (2018) Fracture and dislocation compendium. Scapula fractures. J Orthop Trauma (Suppl) 32:S101–S104. https://doi.org/10.1097/BOT.0000000000001070
Reckova M, Rosengarten C, de Almeida A, Stanley CP, Wessels A, Gourdie R, Thompson RP, Sedmera D (2003) Hemodynamics is a key epigenetic factor in development of the cardiac conduction system. Circ Res 93(1):77–85. https://doi.org/10.1161/01.RES.0000079488.91342.B7
Simon P, Diaz M, Cusick M, Santoni B, Frankle M (2018) 3D image-based morphometric analysis of the scapular neck length in subject undergoing reverse shoulder arthroplasty. Clin Anat 31:43–55. https://doi.org/10.1002/ca.22911
Singh N, Chauhan P, Loh HK, Kohli M, Suri RK (2018) Enigma of scapular foramen and tunnels: an untold story. Surg Radiol Anat 40:327–332. https://doi.org/10.1007/s00276-017-1931-y
Sinha RR, Kumar B, Kulkarni JP (2018) Morphometry and morphology of glenoid fossa of scapula. Indian J Clin Anat Physiol 5:303–307
Tanton J (1915) Fractures en général-Fractures des membres supérieurs. JB Baillière, Paris, pp 785–819
Totlis T, Konstantidinis GA, Karanassos MT, Sofidis G, Anastasopoulos N, Natsis K (2014) Bony structures related to snapping scapula: correlation to gender, side and age. Surg Radiol Anat 36:3–9. https://doi.org/10.1007/s00276-013-1130-4
Tuček M, Bartoníček J, Frič V (2011) Osseous anatomy of scapula: its importance for classification of scapular body fractures. Ortopedie 5:104–109
Alfaro-Gomez U, Fuentes-Ramirez LD, Chavez-Blanco KI, Vilchez-Cavazos JF, Zdilla MJ, Elizondo-Omana RE, Guerra-Leal JD, Elizondo-Riojas G, Pinales-Razo R, Guzman-Lopez S, Quiroga-Garza A (2020) Anatomical variations of the acromial and coracoid process: clinical relevance. Surg Radiol Anat 42(8):877–885. https://doi.org/10.1007/s00276-020-02497-5
von Schroeder HP, Kuiper SD, Botte MJ (2001) Osseous anatomy of the scapula. Clin Orthop Relat Res 383:131–139. https://doi.org/10.1097/00003086-200102000-00015
Zhang L, Guo X, Liu Y, Ou M, Lin X, Qi J, Xu Y, Wang G, Fu S (2019) Classification of the superior angle of the scapula and its correlation with the suprascapular notch: a study on 303 scapulae. Surg Radiol Anat 41:377–383. https://doi.org/10.1007/s00276-018-2156-4
Acknowledgements
The authors wish to thank Prof. Chris Colton MB BS FRCS and Ludmila Bébarová PhD for their assistance in editing of the manuscript.
Funding
Supported by IP DZRVO MO1012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants, or animals, performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in our scapular research.
Disclaimer
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Strnad, T., Bartoníček, J., Naňka, O. et al. The coracoglenoid notch: anatomy and clinical significance. Surg Radiol Anat 43, 11–17 (2021). https://doi.org/10.1007/s00276-020-02527-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-020-02527-2