Abstract
Purpose
It is hypothesized that vitamin B12 may prevent tumor initiation during the early stage of carcinogenesis such as esophageal precancerous lesions (EPL), whereas an excessive level may promote tumor progression during the later stages of carcinogenesis. This study aimed to determine the role of vitamin B12 in EPL by detecting vitamin B12-related markers in both blood and diet.
Methods
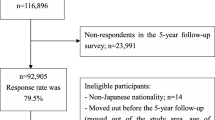
This case–control study based on 3-day duplicated diet samples was conducted in a high-risk area of Huai'an, China. A 100 EPL cases and 100 healthy controls matched by gender, age (± 2 years) and villages were included. Dietary intake of vitamin B12 and cobalt, plasma cobalt level, the serum levels of vitamin B12 and transcobalamin II (TC II) were quantitatively analyzed.
Results
Dietary vitamin B12 intake (p for trend = 0.384) and plasma cobalt level (p for trend = 0.253) were not associated with EPL risk, but high dietary cobalt intake (p for trend = 0.034), increased serum levels of vitamin B12 (p for trend = 0.036) and TC II (p for trend < 0.001) were significantly associated with the reduced EPL risk. However, the significant negative association between dietary cobalt intake, plasma cobalt level or serum vitamin B12 level and EPL was only found in female or male subjects.
Conclusion
Excellent transport capability of bio-active vitamin B12 in vivo and adequate levels of vitamin B12 and cobalt may play preventive roles in EPL. Additionally, the association between vitamin B12, cobalt and the risk of EPL may vary in different genders.


Similar content being viewed by others
Availability of data and material
All data generated or analyzed during this study are included.
Code availability
The technical appendix and statistical procedure are available from the corresponding author.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence: interval
- DHQ:
-
Dietary history questionnaire
- EAC:
-
Esophageal adenocarcinoma
- EC:
-
Esophageal cancer
- EDETPEC:
-
Early Diagnosis and Early Treatment Project of Esophageal Cancer
- ELISA:
-
Enzyme-linked immunosorbent assay
- EPL:
-
Esophageal precancerous lesion
- ESCC:
-
Esophageal squamous cell carcinoma
- FFQ:
-
Food frequency questionnaire
- MTHFR:
-
5,10-Methylenetetrahydrofolate reductase
- OD:
-
Optical density
- OR:
-
Odds ratio
- TC II:
-
Transcobalamin II
References
Pan D, Su M, Zhang T, Miao C, Fu L, Yang L, Song G, Raine PJ, Wang S, Sun G (2019) A distinct epidemiologic pattern of precancerous lesions of esophageal squamous cell carcinoma in a high-risk Area of Huai’an, Jiangsu Province. China Cancer Prev Res 12(7):449–462. https://doi.org/10.1158/1940-6207.capr-18-0462
Rustgi AK, El-Serag HB (2014) Esophageal carcinoma. N Engl J Med 371(26):2499
Zhang T, Pan D, Su M, Fu LM, Miao CY, Yan QY, Wang J, Yang LG, Wang SK, Sun GJ (2018) Determination of dietary nitrite in patients with esophageal pre-cancerous lesion and normal people: a duplicate diet study. Food Addit Contam A 35(12):2298–2308. https://doi.org/10.1080/19440049.2018.1546906
Wang S, Pan D, Zhang T, Su M, Sun G, Wei J, Guo Z, Wang K, Song G, Yan Q (2020) Corn flour intake, aflatoxin B1 exposure, and risk of esophageal precancerous lesions in a high-risk area of huai’an, china: a case-control study. Toxins 12(5):299. https://doi.org/10.3390/toxins12050299
Wang S, Pan D, Su M, Huang G, Sun G (2020) Moderately high folate level may offset the effects of aberrant DNA methylation of P16 and P53 genes in esophageal squamous cell carcinoma and precancerous lesions. Genes & Nutrition 15(1):18. https://doi.org/10.1186/s12263-020-00677-x
Abnet CC, Arnold M, Wei WQ (2018) Epidemiology of esophageal squamous cell carcinoma. Gastroenterology 154(2):360–373. https://doi.org/10.1053/j.gastro.2017.08.023
Qiang Y, Li Q, Xin Y, Fang X, Tian Y, Ma J, Wang J, Wang Q, Zhang R, Wang J, Wang F (2018) Intake of dietary one-carbon metabolism-related b vitamins and the risk of esophageal cancer: a dose-response meta-analysis. Nutrients 10(7):835
Xiao Q, Freedman ND, Ren J, Hollenbeck AR, Abnet CC, Park Y (2014) Intakes of folate, methionine, vitamin B6, and vitamin B12 with risk of esophageal and gastric cancer in a large cohort study. Br J Cancer 110(5):1328–1333
Matejcic M, de Batlle J, Ricci C, Biessy C, Perrier F, Huybrechts I, Weiderpass E, Boutron-Ruault MC, Cadeau C, His M, Cox DG, Boeing H, Fortner RT, Kaaks R, Lagiou P, Trichopoulou A, Benetou V, Tumino R, Panico S, Sieri S, Palli D, Ricceri F, Bueno-de-Mesquita HB, Skeie G, Amiano P, Sanchez MJ, Chirlaque MD, Barricarte A, Quiros JR, Buckland G, van Gils CH, Peeters PH, Key TJ, Riboli E, Gylling B, Zeleniuch-Jacquotte A, Gunter MJ, Romieu I, Chajes V (2017) Biomarkers of folate and vitamin B12 and breast cancer risk: report from the EPIC cohort. Int J Cancer 140(6):1246–1259. https://doi.org/10.1002/ijc.30536
Hultdin J, Van Guelpen B, Bergh A, Hallmans G, Stattin P (2005) Plasma folate, vitamin B12, and homocysteine and prostate cancer risk: a prospective study. Int J Cancer 113(5):819–824. https://doi.org/10.1002/ijc.20646
Price AJ, Travis RC, Appleby PN, Albanes D, Barricarte Gurrea A, Bjorge T, Bueno-de-Mesquita HB, Chen C, Donovan J, Gislefoss R, Goodman G, Gunter M, Hamdy FC, Johansson M, King IB, Kuhn T, Mannisto S, Martin RM, Meyer K, Neal DE, Neuhouser ML, Nygard O, Stattin P, Tell GS, Trichopoulou A, Tumino R, Ueland PM, Ulvik A, de Vogel S, Vollset SE, Weinstein SJ, Key TJ, Allen NE, Endogenous Hormones NB, Prostate Cancer Collaborative G (2016) Circulating folate and vitamin B12 and risk of prostate cancer: a collaborative analysis of individual participant data from six cohorts including 6875 cases and 8104 controls. Eur Urol 70(6):941–951. https://doi.org/10.1016/j.eururo.2016.03.029
de Vogel S, Meyer K, Fredriksen A, Ulvik A, Ueland PM, Nygard O, Vollset SE, Tell GS, Tretli S, Bjorge T (2013) Serum folate and vitamin B12 concentrations in relation to prostate cancer risk–a Norwegian population-based nested case-control study of 3000 cases and 3000 controls within the JANUS cohort. Int J Epidemiol 42(1):201–210. https://doi.org/10.1093/ije/dys199
Pan D, Su M, Huang G, Luo P, Zhang T, Fu L, Wei J, Wang S, Sun G (2019) MTHFR C677T genetic polymorphism in combination with serum vitamin B2, B12 and aberrant DNA methylation of P16 and P53 genes in esophageal squamous cell carcinoma and esophageal precancerous lesions: a case-control study. Cancer Cell Int 19:288. https://doi.org/10.1186/s12935-019-1012-x
Arendt JFH, Sorensen HT, Horsfall LJ, Petersen I (2019) Elevated vitamin B12 levels and cancer risk in UK primary care: a THIN database cohort study. Cancer Epidemiol Biomarkers Prev 28(4):814–821. https://doi.org/10.1158/1055-9965.EPI-17-1136
Araghi SO, Kiefte-de Jong JC, van Dijk SC, Swart KMA, van Laarhoven HW, van Schoor NM, de Groot LCPGM, Lemmens V, Stricker BH, Uitterlinden AG, van der Velde N (2019) Folic acid and vitamin B12 supplementation and the risk of cancer: long-term follow-up of the B vitamins for the prevention of osteoporotic fractures (B-PROOF) trial. Cancer Epidemiol Biomarkers Prev 28(2):275–282. https://doi.org/10.1158/1055-9965.EPI-17-1198
Collin SM, Metcalfe C, Refsum H, Lewis SJ, Zuccolo L, Smith GD, Chen L, Harris R, Davis M, Marsden G, Johnston C, Lane JA, Ebbing M, Bonaa KH, Nygard O, Ueland PM, Grau MV, Baron JA, Donovan JL, Neal DE, Hamdy FC, Smith AD, Martin RM (2010) Circulating folate, vitamin B12, homocysteine, vitamin B12 transport proteins, and risk of prostate cancer: a case-control study, systematic review, and meta-analysis. Cancer Epidemiol Biomarkers Prev 19(6):1632–1642. https://doi.org/10.1158/1055-9965.EPI-10-0180
Lajous M, Willett W, Lazcano-Ponce E, Sanchez-Zamorano LM, Hernandez-Avila M, Romieu I (2006) Folate, vitamin B12 and vitamin B6 intake and the risk of breast cancer among Mexican women. Am J Epidemiol 161(11):S14–S14
Zhang SM, Cook NR, Albert CM, Gaziano JM, Buring JE, Manson JE (2008) Effect of combined folic acid, vitamin B6, and vitamin B12 on cancer risk in women: a randomized trial. JAMA 300(17):2012–2021. https://doi.org/10.1001/jama.2008.555
van den Donk M, Pellis L, Crott JW, van Engeland M, Friederich P, Nagengast FM, van Bergeijk JD, de Boer SY, Mason JB, Kok FJ, Keijer J, Kampman E (2007) Folic acid and vitamin B-12 supplementation does not favorably influence uracil incorporation and promoter methylation in rectal mucosa DNA of subjects with previous colorectal adenomas. The Journal of nutrition 137(9):2114–2120. https://doi.org/10.1093/jn/137.9.2114
Kok DE, Dhonukshe-Rutten RA, Lute C, Heil SG, Uitterlinden AG, van der Velde N, van Meurs JB, van Schoor NM, Hooiveld GJ, de Groot LC, Kampman E, Steegenga WT (2015) The effects of long-term daily folic acid and vitamin B12 supplementation on genome-wide DNA methylation in elderly subjects. Clin Epigenet 7:121. https://doi.org/10.1186/s13148-015-0154-5
Brasky TM, White E, Chen CL (2017) Long-term, supplemental, one-carbon metabolism-related vitamin B use in relation to lung cancer risk in the vitamins and lifestyle (VITAL) cohort. J Clin Oncol 35(30):3440–3448. https://doi.org/10.1200/JCO.2017.72.7735
Bonetti F, Brombo G, Zuliani G (2017) Chapter 15 – The Role of B Group Vitamins and Choline in Cognition and Brain Aging. Nutr Funct Foods Healthy Aging
Kohlmeier M (2003) Vitamin B12. In. pp 603–613. https://doi.org/10.1016/B978-012417762-8.50085-5
Allen RH, Stabler SP (2008) Identification and quantitation of cobalamin and cobalamin analogues in human feces. Am J Clin Nutr 87(5):1324–1335. https://doi.org/10.1093/ajcn/87.5.1324
Albert MJ, Mathan VI, Baker SJ (1980) Vitamin B12 synthesis by human small intestinal bacteria. Nature 283(5749):781–782. https://doi.org/10.1038/283781a0
Carmel R, Herbert V (1969) Deficiency of vitamin B12-binding alpha globulin in two brothers. Blood 33(1):1–12
Oberley MJ, Yang DT (2013) Laboratory testing for cobalamin deficiency in megaloblastic anemia. Am J Hematol 88(6):522–526. https://doi.org/10.1002/ajh.23421
Unal S, Rupar T, Yetgin S, Yarali N, Dursun A, Gursel T, Cetin M (2015) Transcobalamin II deficiency in four cases with novel mutations. Turk J Hematol 32(4):317–322. https://doi.org/10.4274/tjh.2014.0154
Meyers PA, Carmel R (1984) Hereditary transcobalamin-II deficiency with subnormal serum cobalamin levels. Pediatrics 74(5):866–871
Schiff M, de Baulny HO, Bard G, Barlogis V, Hamel C, Moat SJ, Odent S, Shortland G, Touati G, Giraudier S (2010) Should transcobalamin deficiency be treated aggressively? J Inherit Metab Dis 33(3):223–229. https://doi.org/10.1007/s10545-010-9074-x
Pan D, Wang SK, Su M, Wei J, Wang K, Luo PF, Smith JD, Ma GG, Sun GJ (2020) Roles of drinking and diet in the U-shaped relationship between smoking and BMI in middle-aged and elderly Chinese rural adults. Sci Rep-Uk 10 (1)
Chatthanawaree W (2011) Biomarkers of cobalamin (vitamin B12) deficiency and its application. J Nutr Health Aging 15(3):227–231. https://doi.org/10.1007/s12603-010-0280-x
Cui XY, Wang B, Wu YM, Xie LY, Tang QY, Shen XH (2019) Vitamin B12 status of vegetarians in Shanghai. Chin J Clin Nutr 27(2):107–112
Bailey LB (2004) Folate and vitamin B-12 recommended intakes and status in the United States. Nutr Rev 62(6):S14–S20. https://doi.org/10.1111/j.1753-4887.2004.tb00065.x
Coleman HG, Xie SH, Lagergren J (2018) The epidemiology of esophageal adenocarcinoma. Gastroenterology 154(2):390–405. https://doi.org/10.1053/j.gastro.2017.07.046
Mayne ST, Risch HA, Dubrow R, Chow WH, Gammon MD, Vaughan TL, Farrow DC, Schoenberg JB, Stanford JL, Ahsan H, West AB, Rotterdam H, Blot WJ, Fraumeni JF (2001) Nutrient intake and risk of subtypes of esophageal and gastric cancer. Cancer Epidemiol Biomarkers Prev 10(10):1055–1062
O’Doherty MG, Cantwell MM, Murray LJ, Anderson LA, Abnet CC, Grp FS (2011) Dietary fat and meat intakes and risk of reflux esophagitis, Barrett’s esophagus and esophageal adenocarcinoma. Int J Cancer 129(6):1493–1502. https://doi.org/10.1002/ijc.26108
Jorhem L, Sundström B (1993) Levels of lead, cadmium, zinc, copper, nickel, chromium, manganese, and cobalt in foods on the swedish market, 1983–1990. J Food Compos Anal 6(3):223–241. https://doi.org/10.1006/jfca.1993.1025
Xie LY, Wang B, Ma K, Mao XX, Shen XH (2018) The content of vitmain B12 in Chinese common foods. Food Nutr China 24(2):73–76
Rose M (1976) Letter: Vitamin-B12 deficiency in Asian immigrants. Lancet 2(7987):681. https://doi.org/10.1016/s0140-6736(76)92482-x
No author. Contribution Of the Microflora Of the Small-Intestine To the Vitamin-B12 Nutriture Of Man (1980). Nutrition Reviews 38 (8):274–275
Ma Z, Li W (2019) How and why men and women differ in their microbiomes: medical ecology and network analyses of the microgenderome. Adv Sci 6(23):1902054. https://doi.org/10.1002/advs.201902054
Combs GF (2012) Chapter 17 - Vitamin B12. In: Combs GF (ed) The Vitamins, 4th edn. Academic Press, San Diego, pp 377–394. https://doi.org/10.1016/B978-0-12-381980-2.00017-7
De Stefani E, Ronco A, Mendilaharsu M, Deneo-Pellegrini H (1999) Diet and risk of cancer of the upper aerodigestive tract–II. Nutr Oral Oncol 35(1):22–26. https://doi.org/10.1016/s1368-8375(98)00061-x
Jessri M, Rashidkhani B, Hajizadeh B, Jessri M, Gotay C (2011) Macronutrients, vitamins and minerals intake and risk of esophageal squamous cell carcinoma: a case-control study in Iran. Nutr J 10:137. https://doi.org/10.1186/1475-2891-10-137
Tuyns AJ, Riboli E, Doornbos G, Pequignot G (1987) Diet and esophageal cancer in Calvados (France). Nutr Cancer 9(2–3):81–92. https://doi.org/10.1080/01635588709513915
Ibiebele TI, Hughes MC, Pandeya N, Zhao Z, Montgomery G, Hayward N, Green AC, Whiteman DC, Webb PM, Study of Digestive H, Australian Cancer S (2011) High intake of folate from food sources is associated with reduced risk of esophageal cancer in an Australian population. J Nutr 141(2):274–283. https://doi.org/10.3945/jn.110.131235
Acknowledgments
We thank all the participants, researchers and collaborators who were involved in the study for their efforts and contribution. Thanks to Dr. Ying Zhang for providing technical guidance on methods for ICP-MS. Thanks also to Mr Rob Unwin for proof reading. This research was supported by the National Natural Science Foundation of China (No. 81673147), Postgraduate Research & Practice Innovation Program of Jiangsu Province (SJCX20_0063) and the Danone Dietary Nutrition Research and Education Foundation (DIC2020-08). The funding unit had no role in the whole study including study design, collection of data, and analysis of results and composition of the manuscript.
Funding
This research was supported by the National Natural Science Foundation of China (No. 81673147), Postgraduate Research & Practice Innovation Program of Jiangsu Province (SJCX20_0063) and the Danone Dietary Nutrition Research and Education Foundation (DIC2020-08). The funding unit had no role in the whole study including study design, collection of data, analysis of results, and composition of the manuscript.
Author information
Authors and Affiliations
Contributions
DP, SW, and GS designed research; DP, MS, XZ, MGC, ZG, NW, and ZZ conducted research; SW, MS, MC, and GS provided essential materials; DP analyzed data; DP wrote paper; SW had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The study was approved by the Institutional Review Board of Southeast University Zhongda Hospital, in accordance with the Declaration of Helsinki.
Consent to participate
Written informed consent was obtained from each subject.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pan, D., Wang, S., Su, M. et al. Vitamin B12 may play a preventive role in esophageal precancerous lesions: a case–control study based on markers in blood and 3-day duplicate diet samples. Eur J Nutr 60, 3375–3386 (2021). https://doi.org/10.1007/s00394-021-02516-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-021-02516-0